Platform Presentations
This is an accordion element with a series of buttons that open and close related content panels.
Establishing Normal Renal Tissue Oxygenation Values in Preterm Neonates
Title: Establishing Normal Renal Tissue Oxygenation Values in Preterm Neonates
Condit PE; Chuck J; Lasarev M; Chock VY; Harer M
Background: Near infrared spectroscopy (NIRS) is increasingly being used to non-invasively measure renal regional saturation of oxygen (RrSO2) in preterm neonates. Given rapidly changing renal physiology and the wide range of renal development associated with varying preterm gestational ages, RrSO2 is likely to change significantly in the first week. A previous study showed preterm neonates with acute kidney injury (AKI) had lower RrSO2 on the first day of life than those without AKI. However, normal changes in RrSO2 in a large cohort of preterm neonates from more than one center during the first week have yet to be described. The objective of this study is to describe RrSO2 values during the first week of life for preterm neonates born <32 weeks gestational age (GA).
Design/Methods: A two-site analysis was performed using prospectively measured NIRS data obtained from existing cohorts at two sites (G & H). All neonates born <32 weeks GA without known congenital anomalies of the kidney were included. Both sites used INVOS NIRS monitors, neonatal sensors, and Mepitel for skin protection. Data was visible and available to clinicians at site G and was blinded to clinicians at site H. Continuous RrSO2 values (%) were collected during the first 168 hours of life (HOL) with trends over time analyzed using generalized estimating equations.
Results: The study included 109 neonates (35 from G and 74 from H) with differing GA between sites (median 29.0 vs 26.5 weeks for G vs H; p <0.001). Separately-fitted trends in RrSO2 did not differ (p=0.52) between sites and demonstrated a consistent decrease in RrSO2 during first 60 HOL followed by a stabilization of RrSO2 thereafter. Average RrSO2 was 10.8 points lower for Site G compared to H (p<0.001).
Conclusions: RrSO2 is estimated to decrease 20 points (95% CI: 9.6–30.1) during the first 60 HOL and stabilizes thereafter. While differences in RrSO2 persist between sites, despite controlling for gestational age, mode of delivery, and infant sex, the profiles over time are consistent, allowing for determination of expected RrSO2 trajectories in preterm infants. Large multicenter prospective renal NIRS monitoring studies are needed to further define normal values at all gestational ages so clinical protocols can be developed to treat abnormal values that may be associated with AKI.
Accurate Assessment of Adverse Outcomes of Neonatal Circumcision
Title: Accurate Assessment of Adverse Outcomes of Neonatal Circumcision
Hauser B, Farhart W, Goetz E
Background: Although neonatal circumcision is one of the most frequently performed surgical procedure in males, the incidence of neonatal circumcision adverse outcomes (NCAO) continues to be around 5% and has remained unchanged for decades. Multi-institutional databases may not accurately reflect the true incidence of NCAO as data is assimilated from many institutions with disparate practices. The pediatric health care system in Madison WI provides a unique opportunity to more closely examine NCAO from two birthing hospitals served by one tertiary care center with pediatric urologists. We reviewed the outcome of neonatal circumcision in this system in order to assess incidence and identify possible factors associated with NCAO that could be targeted to reduce complications.
Design/Methods: During a five-year period 01/01/2016 to 10/26/2020, all revisions after neonatal circumcision performed at one of the two birthing centers in Madison WI were reviewed. In order to capture all the different revisions performed, patients were identified through review of surgical procedures performed at the American Family Children’s Hospital (AFCH) and patients coded for circumcision revision (CPT 54161, 54163), or lysis of penile adhesions (CPT 54162). Patient charts were then individually reviewed to account for all NCAO.
Results: During this period, there were 11,060 neonatal circumcisions performed at the two birthing centers in Madison, WI. The total number of revision or repairs due to NCAO was 229. 169 circumcisions required lysis of adhesions or skin bridge and 60 circumcisions required revision for redundant foreskin (17), buried penis (9), incomplete circumcision (33) and retained plastibell (1). The overall complication rate was 2% and was independent of the specialty performing the circumcision and method used. During this time period 55 infants had newborn circumcision deferred due to concerns about anatomy. Of these infants, 51 (93%) went on to have uncomplicated circumcision in first 2 years of life.
Conclusions: Despite our overall low complication rate, the most prevalent complications of adhesions and skin bridge formation, redundant foreskin, incomplete circumcision and buried penis suggest variability in anatomic assessment, circumcision technique, and post-circumcision care among providers performing neonatal circumcision. In addition, the majority of newborns who had circumcision deferred during the birth hospitalization due to anatomic concerns went on to have uncomplicated circumcision within the first 2 years of life, further suggesting variability in anatomic pre-circumcision assessment. A standardized education programs for circumcision may reduce variability and complications.
Comparison of Structural Brain Imaging in Infant Macaques with Prenatal Zika Virus Exposure in Early and Mid-First Trimester
Title: Comparison of Structural Brain Imaging in Infant Macaques with Prenatal Zika Virus Exposure in Early and Mid-First Trimester
Moore B, Hlubek L, Sun A, Pham T, Nair V, Ausderau K, Prabhakaran V, Mohr E
Background: Prenatal Zika virus (ZIKV) infection negatively impacts fetal brain development, and results in a spectrum of developmental outcomes in infants, including infants that develop as neurotypical, with mild-moderate developmental deficits, and infants that develop with congenital Zika syndrome. The pathogenesis leading to differences in neural development, including the impact of gestational age at time of ZIKV infection is not well defined, but the timing of ZIKV exposure during fetal neurodevelopment may be an important predictor of developmental outcomes. Herein, we use a Rhesus macaque model of prenatal ZIKV infection to quantitatively assess structural differences in fetal brain development in infants exposed in early and mid-first trimester of gestation. We hypothesize that infants exposed to ZIKV early in the first trimester will have more brain abnormalities than infants exposed to ZIKV in the middle of the first trimester.
Design/Methods: Pregnant rhesus macaques (n=11) were inoculated by subcutaneous injection with 1.0 x 104 PFU strain of Zika virus at gestational day 30 (n=6) or gestational day 45 (n=5). Infants were delivered via Cesarean section at gestational day 158-160. At three months of age, infant macaques underwent magnetic resonance imaging. Obtained neuroimages were analyzed with an AutoSeg_3.3.2 pipeline to evaluate structural volumetric development of cortical and subcortical brain regions.
Results: Infants exposed to ZIKV at gestational day 45 have significantly reduced structural development in brain areas important for motor function relative to infants infected at gestational day 30. Specifically, infants infected with ZIKV at gestational day 45 have significantly smaller parietal lobe (p=0.0232), caudate (p=0.0423), and putamen (p=0.0298) brain region volumes relative to infants infected at gestational day 30.
Conclusions: These results suggest that gestational age at time of ZIKV exposure impacts structural development of the fetal brain. In contrast to our hypothesis, infants exposed to ZIKV mid-first trimester had more brain abnormalities than those exposed early in the first trimester. Ongoing developmental studies will elucidate how these early brain changes underlie later developmental outcomes. Defining the risk of brain abnormalities and developmental deficits associated with different gestational ages at ZIKV exposure will provide insight for targeted therapeutic interventions during pregnancy.
Translational Read-Through of a KCNJ13 Nonsense Mutation With ELX-01 And ELX-03 Results in Functional Kir7.1 Channels
Title: Translational Read-Through of a KCNJ13 Nonsense Mutation With ELX-01 And ELX-03 Results in Functional Kir7.1 Channels
Zapata Galarza H, Shahi P, McMillin D, Crawford D, Pattnaik B
Background: The KCNJ13 gene encodes the inwardly rectifying potassium channel Kir7.1. Nonsense mutations in this gene are known to cause Leber Congenital Amaurosis 16 (LCA 16), leading to early-onset vision loss. This form of autosomal recessive blindness is characterized by severe vision impairment, nystagmus, and photophobia in the pediatric population. We previously demonstrated a readthrough of the Kir7.1 restored the channel function. In this study, we tested the effect of treating the KCNJ13 nonsense mutation W53X with the novel eukaryotic ribosome selective glycoside compounds ELX-01 and ELX-03.
Design/Methods: Human Embryonic Kidney (HEK293T) cells were plated on a 35mm culture dish until 60-70% confluence. Cells were then transfected with a plasmid carrying KCNJ13 nonsense mutation at 53rd amino acid (c.158G>A, W53X) and fused with Green Fluorescent Protein (GFP). After 24 hours of transfection, the cells were incubated with readthrough compounds ELX-01 and ELX-03 at 1mM for additional 24 hours. The cells were transferred to glass coverslips for whole-cell patch-clamp electrophysiology. Ringer’s solution was continuously perfused as an external solution. Rubidium (Rb+) -Ringer’s solution was used to test the Kir7.1 channel function.
Results: Detection of GFP fluorescence in GFP tagged W53X transfected HEK293T cell membranes confirmed Kir7.1 protein expression. Previously demonstrated, W53X transfection resulted in non-measurable Kir7.1 current because of the truncated protein product. After we treated these cells with ELX-01 and ELX-03 at 1 mM concentration, the current-voltage curve showed inward rectifying Kir7.1 current. The maximum inward current measured at -160 mV was -90.63 ± 8.23 pA and -68.66 ± 30.56 pA, respectively, compared to only -18.61 ± 7.23 pA without the drug treatment. Upon substitution with Rb-Ringer, the maximum current amplitude did not change in non-treated cell measuring -18.92 ± 5.18 pA but increased to -502.93 ± 50.65 pA, a ~5.64-fold increase with ELX-01 treatment. Similarly, ELX-03 increased the maximum current to -768.02 ± 137.84 pA, representing a ~7.1-fold increase.
Conclusions: Both ELX-01 and ELX-03 are able to restore the translation of full-length and functional Kir7.1 channel in HEK cells. Further evaluation of these compounds will ensure readthrough effects on LCA16 patient-derived iPSC-RPE and mouse models for preclinical validation.
Rapid and Motion-Corrected Multiparametric Imaging in Young Children
Title: Rapid and Motion-Corrected Multiparametric Imaging in Young Children
Dean DC III, Kecskemeti S, Heinrich L, DiPiero M, Pletcher C, Takei N, Rettmann D, Banerjee S, Alexander AL
Background: Quantitative magnetic resonance imaging can provide novel insights into brain maturation, yet acquisition of these data are limited by challenges of imaging pediatric populations. Here, we utilized a recently developed 3D multiparametric imaging sequence with prospective motion correction to assess the feasibility in acquiring high quality synthetic MRI and qT1 and qT2 maps in children under 10 years of age.
Design/Methods: MRI Acquisition: 26 typically developing children (Mean Age: 5.5 years, age range: 9 months – 10 years; 9 Female; 17 male) were recruited and imaged using a 32-channel head RF array (Nova Medical, Wakefield, MA) on a 3T GE MR70 scanner. Children under 4 years of age were imaged during natural sleep, while children over 4 years of age were imaged awake while watching a movie or TV show. A prototype of the 3D MAGnetic resonance Image Compilation (3D MAGiC) method.
Results: 3D MAGiC imaging data were acquired from 21 of 26 children (80%). Children in which data were not successfully obtained either woke up prior to or during the scan (3) or wished to stop the imaging session prior to collection (2). Gray/white matter contrast are apparent in the synthetic T1w and T2w images, with images becoming more “adult-like” with increasing age. Decreases of quantitative T1 and T2 relaxation times are observed across the brain, reflecting the progressive decreases in water content and brain myelination associated with the maturing brain. Motion-corrected qT1 and qT2 maps illustrate the effectiveness of prospective motion correction at limiting motion artifacts.
Conclusions: 3D MAGiC with PROMO can provide high resolution multiparametric images in under 10 minutes. Combined with the prospective motion correction, this technique may help advance the use of quantitative imaging in pediatric and other challenging populations.
Transgender and Gender-Diverse Youth Have Higher Prevalence of Certain Autoimmune Disease
Title: Transgender and Gender-Diverse Youth Have Higher Prevalence of Certain Autoimmune Disease
Logel S, Whitehead J, Maru J, Walch A, Brady C, Lasarev M, Rehm J, Millington K
Background: Recent studies have reported an increased prevalence of type 1 diabetes mellitus (T1D) in transgender and gender-diverse (TGD) youth compared to the general population. The objective of this study is to determine the prevalence of autoimmune disease in TGD youth relative to the general population.
Design/Methods: TGD individuals, <26 years old, seen in the gender clinics of 5 United States academic medical centers between January 2013–2019 were identified using ICD-10 diagnostic codes for gender dysphoria. These individuals were screened via chart review for concurrent diagnosis with >1 of the following autoimmune diseases: juvenile idiopathic arthritis, systemic lupus erythematosus, Crohn’s disease, ulcerative colitis, celiac disease, T1D, autoimmune thyroiditis, and Graves’ disease. Patients with differences of sexual differentiation and genetic syndromes that place them at higher risk for the development of autoimmune diseases were excluded from the study. Prevalence rates for each autoimmune disease in the general population were estimated via literature review. A logistic model treating site as a random factor was fitted separately for each autoimmune disease. Analyses were performed using Stata (ver. 15.0; StataCorp LLC, College Station, TX).
Results: There were 128 TGD youth with >1 autoimmune disease out of 3812 total TGD youth included in the analysis. The mean age of TGD youth with >1 autoimmune disease was 17 years (range 8-26 years); 32 (25%) were assigned male at birth and 96 (75%) were assigned female at birth. GnRH agonists and gender-affirming hormone therapy was prescribed for 33 and 86 individuals, respectively. The prevalence rates of T1D (5 times), systemic lupus erythematosus (10 times) and Graves’ disease (up to 20 times) were all higher in TGD youth relative to the general population. The prevalence of autoimmune thyroiditis, celiac disease, Crohn’s disease, ulcerative colitis, and juvenile idiopathic arthritis in TGD youth was similar to previously reported prevalence rates for each disorder.
Conclusions: Certain autoimmune diseases have a greater prevalence in TGD youth but the basis is unknown requiring further study. It is possible that increased psychological minority stress, like that experienced by TGD youth, may induce autoimmunity in some genetically susceptible individuals. Increased ascertainment of TGD youth may explain the potential link. Providers should be aware of the increased prevalence of autoimmunity in TGD youth.
Session A: Advocacy, Media and Practice Patterns
Moderator: Megan Moreno, MD
7 minutes each, 12 presenters
3:30-5:00
| Time | Presenter | Title |
|---|---|---|
| 3:30-3:37 | Bryan Vonasek, MD | Screening tests for active pulmonary tuberculosis in children: a systematic review |
| 3:37-3:44 | Julia Claire Walters | Providers’ Attitudes to Proposed Changes in the CCHD Screening Algorithm |
| 3:44-3:51 | Lucas Ebert | How the Covid-19 Vaccine is Discussed on Twitter |
| 3:51-3:58 | Reese Hyzer | A Prevention Approach to Bullying News Media: Partnering with Journalist |
| 3:58-4:05 | Alexandra Mechler-Hickson | Early Literacy Intervention for Infants with Congenital Heart Disease: A Pilot Study |
| 4:05-4:12 | Thomas Harris, MD | ECG screening and interpretation patterns among physicians performing preparticipation physical evaluations (PPE) |
| 4:12-4:19 | Lekha Pillarisetti | Exploring the Discussion Of Nexplanon (Etonogestrel Birth Control Implant) On Twitter |
| 4:19-4:26 | Marc Austin Skiles | A Survey of Pediatric Cardiologists and Cardiac Surgeons on the Care of Congenitally Corrected Transposition of the Great Arteries (L-TGA) |
| 4:26-4:33 | Amrutha Garimella | Discussion of Hallucinogens on TikTok |
| 4:33-4:40 | Katie Tobik | Parental Attitudes and Ideas Regarding Newborn Screening for Familial Hypercholesterolemia |
| 4:40-4:47 | Paige Erickson | Pediatric Oncology Providers Opinions on The Addition of Pediatric Cancer Syndromes to Wisconsin Newborn Screening |
| 4:47-4:54 | Marwat Salamin | Telehealth in Genetics: The Genetic Counselor Perspective on the Utility of Telehealth in Response to the COVID-19 Pandemic in Wisconsin |
| 4:54-5:00 | Wrap-Up |
This is an accordion element with a series of buttons that open and close related content panels.
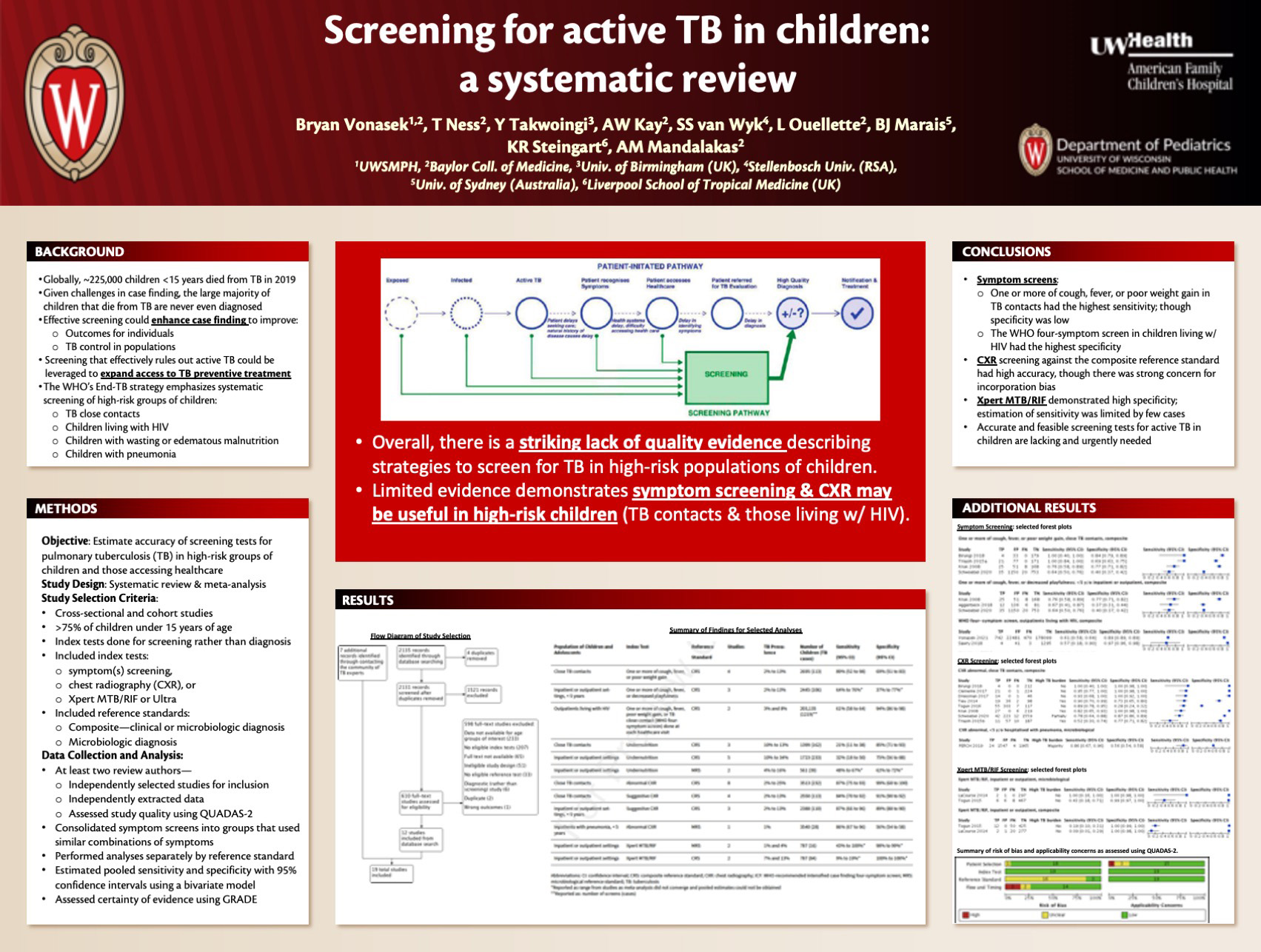
Screening Tests for Active Pulmonary Tuberculosis in Children: a Systematic Review
Click here for .pdf version of poster
Title: Screening Tests for Active Pulmonary Tuberculosis in Children: a Systematic Review
Vonasek B, Ness T, Takwoingi Y, Kay A, Van Wyk S, Ouellette S, Marais B, Steingart K, Mandalakas A
Background: There is urgent need to improve systematic screening for tuberculosis (TB) in high-risk groups of children. The objective of this systematic review was to estimate accuracy of screening tests (symptoms, chest radiography (CXR), and Xpert MTB/RIF) for pulmonary TB in children in high-risk groups.
Design/Methods: We searched six databases, including MEDLINE and Embase, on 14 February 2020. We selected cross-sectional and cohort studies evaluating screening for TB in individuals under 15 years. Reference standards were microbiologic (MRS) and composite reference standard (CRS) incorporating clinical criteria. Two review authors independently extracted data and assessed study quality using QUADAS-2. We used a bivariate model to estimate pooled sensitivity and specificity with 95% confidence intervals (CIs) and performed analyses separately by reference standard. We assessed certainty of evidence using GRADE.
Results: 19 studies assessed the following screens: one symptom – 15 studies (10,097 participants); combinations of symptoms – 12 studies (29,889 participants); CXR – 10 studies (7146 participants); and Xpert MTB/RIF – two studies (787 participants). For 16 studies (84%), risk of bias for the reference standard domain was unclear owing to concern about incorporation bias (symptom and CXR results were included in the CRS). Across other study quality domains, risk of bias was generally low. One or more of cough, fever, or poor weight gain in TB contacts, CRS (4 studies, 2695 participants): pooled sensitivity and specificity (95% CI) were 89% (52% to 98%) and 69% (51% to 83%). One or more of cough, fever, poor weight gain, or tuberculosis close contact, CRS in children living with HIV (CHIV), outpatient (2 studies; 203,135 screens): pooled sensitivity and specificity were 61% (58% to 64%) and 94% (86% to 98%). CXR with any abnormality in tuberculosis contacts, CRS (8 studies, 3513 participants): pooled sensitivity and specificity were 87% (75% to 93%) and 99% (68% to 100%). Xpert MTB/RIF, inpatient or outpatient, MRS (2 studies, 787 participants): sensitivity was 43% and 100% and specificity was 98% and 99%.
Conclusions: Accurate screening tests for pulmonary tuberculosis in children are currently lacking and urgently needed to increase the provision of preventive treatment to high risk children without tuberculosis disease and to increase the timeliness of treatment in those with tuberculosis disease.
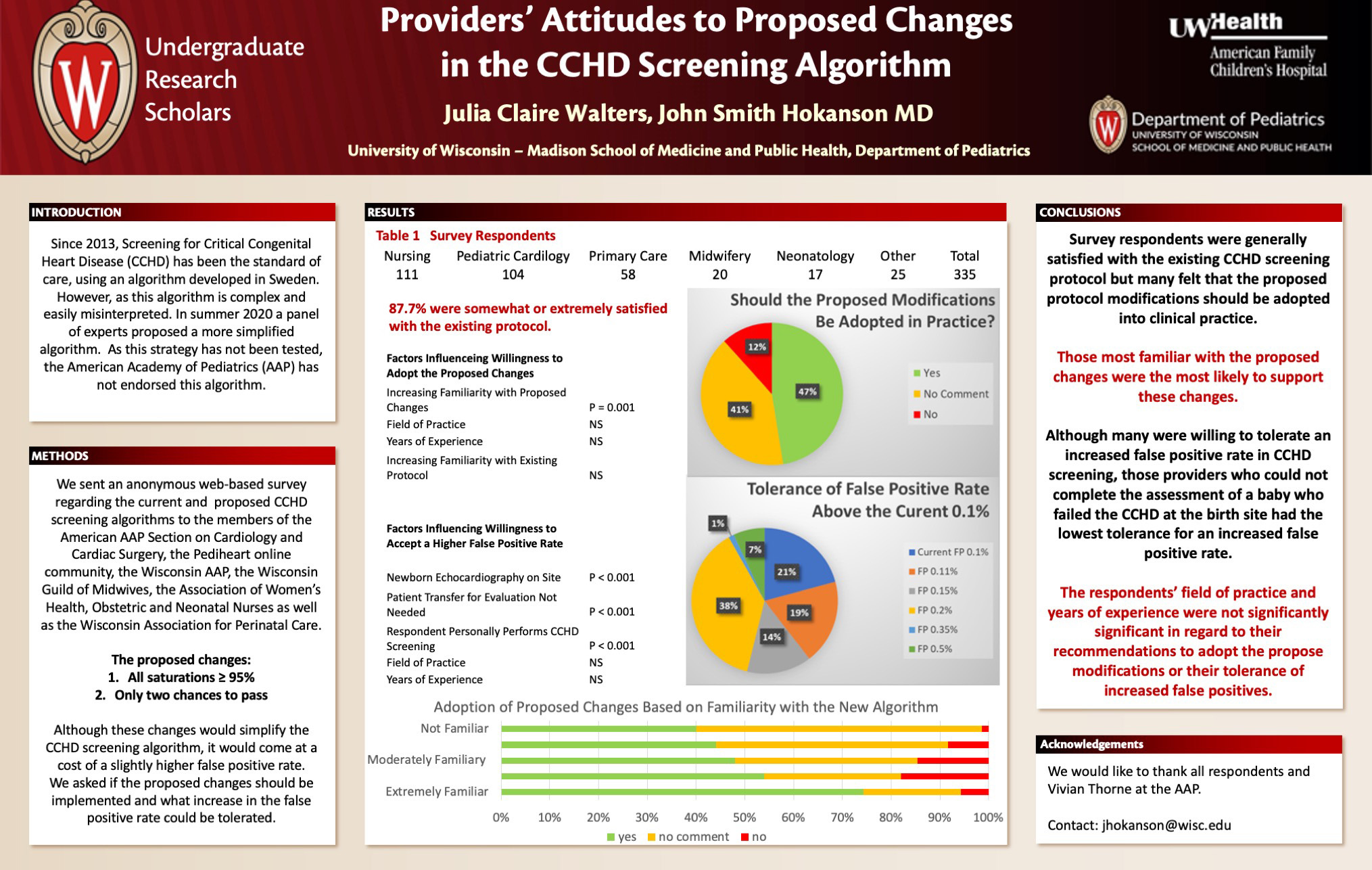
Providers’ Attitudes to Proposed Changes In The CCHD Screening Algorithm
Click here for .pdf version of poster
Title: Providers’ Attitudes to Proposed Changes In The CCHD Screening Algorithm
Walters J, Hokanson J
Background: In 2018, a panel of experts proposed simplifications to the current critical congenital heart disease (CCHD) screening algorithm for newborns. While the American Academy of Pediatrics (AAP) did publish the findings of this meeting in 2020, they did not formally endorse the modifications. Since this proposal has not been endorsed by the AAP, clinicians have been reluctant to change their screening practices.
Design/Methods: An anonymous electronic survey was sent to members of the Wisconsin Association for Perinatal Care, Wisconsin Guild of Midwives, Wisconsin Affiliate of the AAP, the AAP Section on Cardiology and Cardiac Surgery, the Pediheart online cardiology community and the Association of Women’s Health Obstetric and Neonatal Nurses regarding the current and proposed CCHD screening protocols.
Results: We received 335 responses to the survey (Nursing 111, Pediatric Cardiology 104, Primary Care 58, Midwifery 20, Neonatology 17, Administration 4, Other 21). Overall 43.1% of respondents endorsed the proposed changes, 11.2% opposed the changes and 45.6% did not wish to comment. Of responding nurses, 39% endorsed the recommendations, 8.5% opposed the recommendations and 52.1% did not wish to comment. Among pediatric cardiologists, 45.5% endorsed, 16.1% opposed and 38.4% did not wish to comment. Of primary care providers, 46.8% endorsed, 4.8% opposed and 48.4% did not wish to comment. Among midwives, 25% endorsed, 15% opposed and 60% did not wish to comment. Of neonatologists, 61.1% endorsed, 16.7% opposed and 22.2% did not wish to comment. Of respondents self-reporting as extremely familiar with the proposed changes, 74.3% endorsed the recommendations, 5.7% opposed the recommendations and 20% did not wish to comment. Of those self-reporting as not familiar with the proposed changes, 40% endorsed, 1.4% opposed and 58.6% did not wish to comment.
Conclusions: In this survey, those respondents most familiar with the proposed were inclined to endorse the proposed changes in the CCHD screening algorithm. Although the likelihood of endorsing a change in the CCHD protocol varied by profession, more providers recommended the proposed changes than opposed. However, a significant number of survey respondents did not wish to comment on the changing the CCHD screening protocol across all professions and degrees of familiarity with the issue.
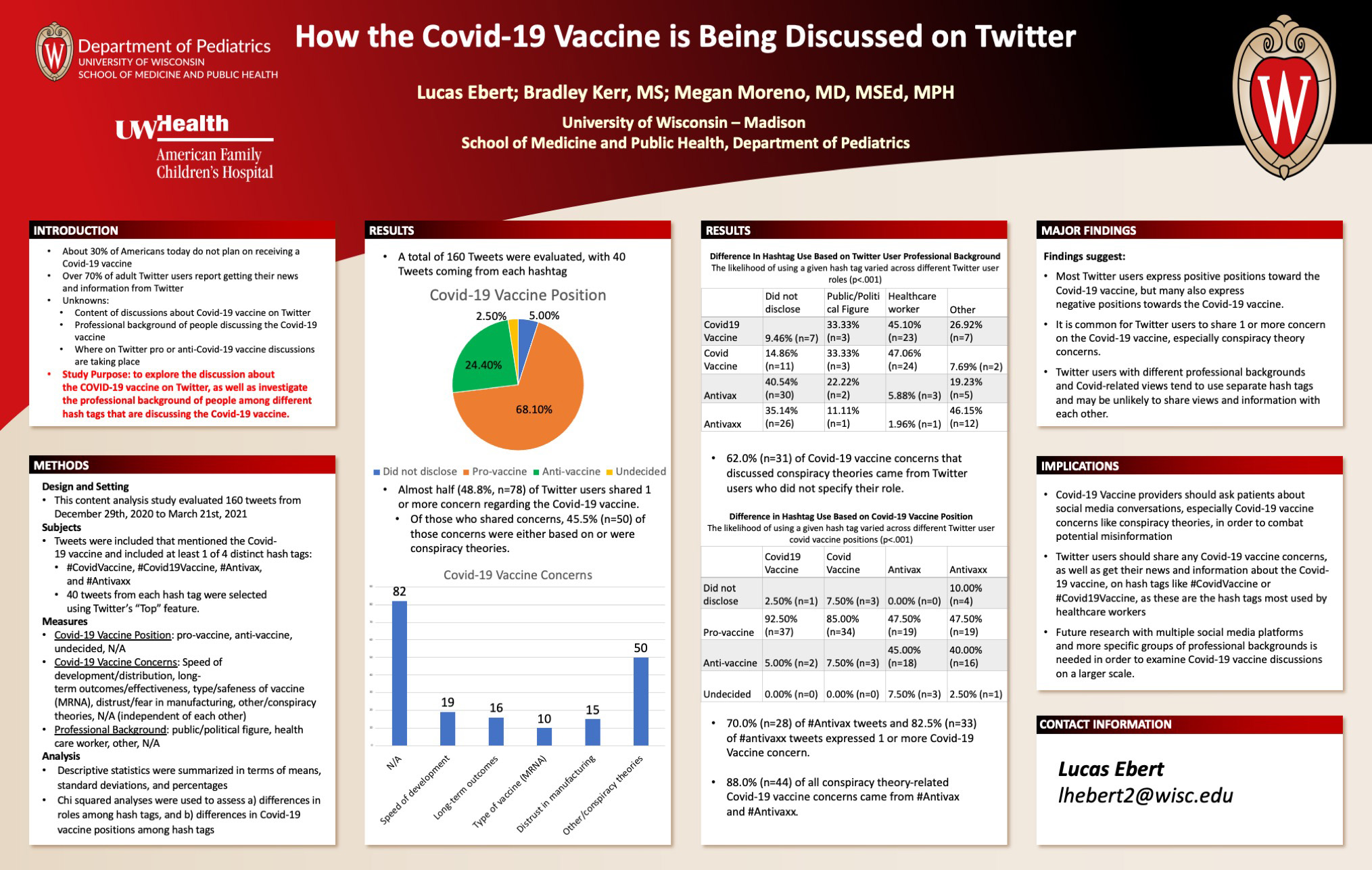
How The Covid-19 Vaccine Is Discussed On Twitter
Click here for .pdf version of poster
Title: How The Covid-19 Vaccine Is Discussed On Twitter
Ebert L, Kerr B, Moreno M
Background: While Covid-19 increasingly affects children, almost a third of American adults report they do not plan on receiving a vaccine. Most adult Twitter users report getting their news from the platform. Twitter discussions about the Covid-19 vaccine remain unknown. The purpose of this study was to explore discussion about the Covid-19 vaccine on Twitter, and to examine differences in professional background and views between different Covid-19 hashtags.
Design/Methods: In this content analysis study, we evaluated 40 tweets from each of four hashtags (#COVIDVaccine, #COVID19Vaccine, #Antivax, and #Antivaxx) dated December 29th, 2020 to March 21st, 2021. Measures included users reported Covid-19 position (pro/anti vaccine), concerns about receiving the Covid-19 vaccine, and professional background (public/political figure, healthcare worker, other, N/A). Descriptive statistics and chi squared tests were used to assess differences in professional background and covid vaccine positions across hashtags.
Results: Out of 160 tweets, 68.1% (n = 109) were categorized as pro-Covid-19 vaccine, while 24.4% (n = 39) were anti-Covid-19 vaccine. About half of tweets (48.8%, n = 78) shared one or more concern regarding the Covid-19 vaccine, with conspiracy theories being the most shared concern (45.5%, n=50). The likelihood of using a given hashtag varied across user professional backgrounds (p < .001). Most healthcare workers (92.2%, n = 47) used #CovidVaccine or # Covid19Vaccine, while 75.7% (n=56) of users who did not disclose their professional background and 65.4% (n = 17) of users with an “other” professional background used #Antivax or #Antivaxx. The likelihood of using a given hashtag also varied across Covid-19 vaccine positions (p<0.001). Most #Covid19Vaccine Tweets (92.5%, n=37) and #CovidVaccine tweets (85.0%, n=34) were categorized as pro-Covid-19 vaccine, while 47.5% (n=19) of #Antivax and #Antivaxx tweets were pro-Covid-19 vaccine.
Conclusions: Tweets frequently expressed concerns about the Covid-19 vaccine. However, healthcare professionals may not reach Twitter users with differing views and professions to provide credible information. Future studies should investigate Covid-19 vaccine discussions on other social media platforms while examining users’ professional backgrounds.
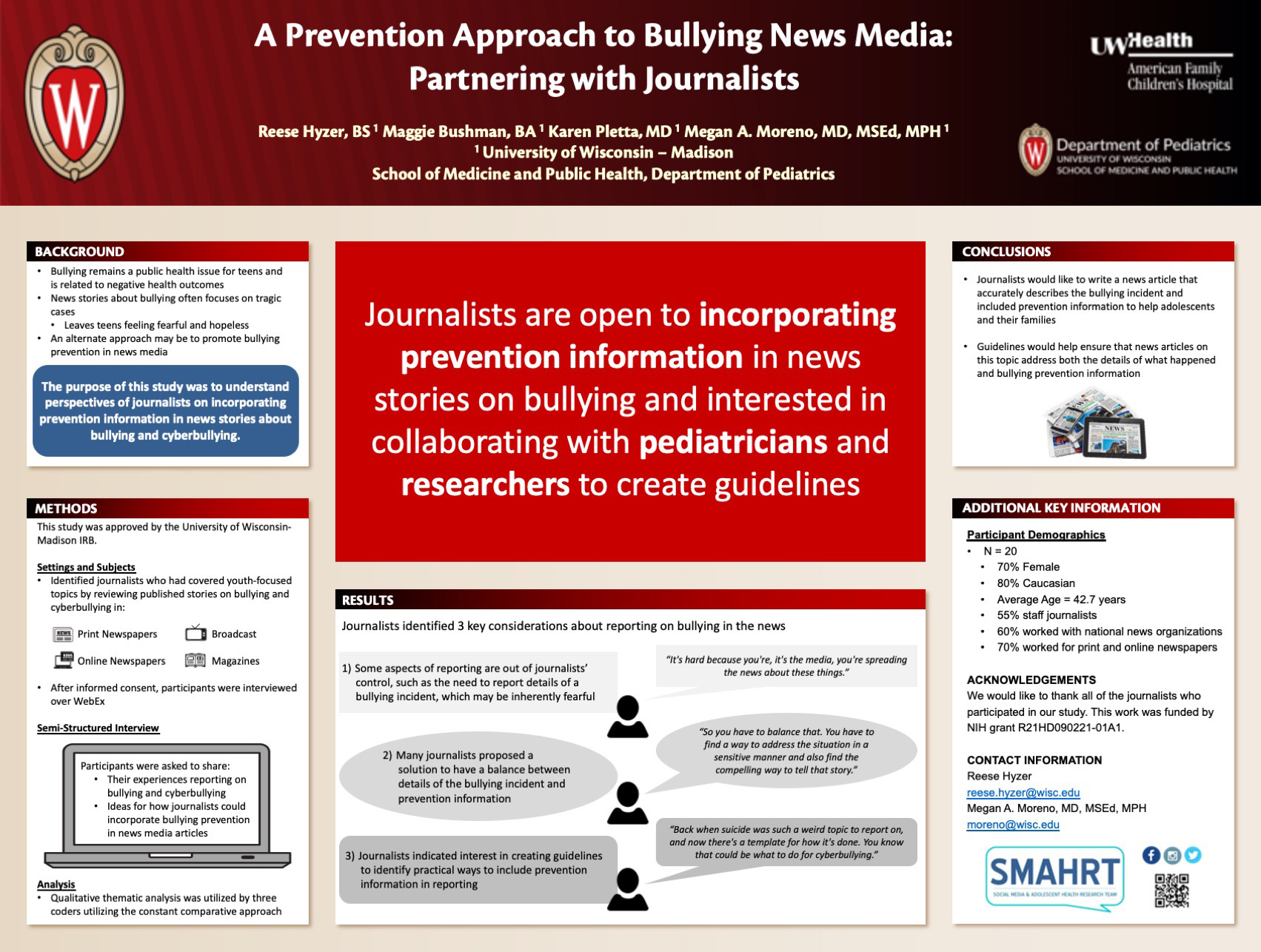
A Prevention Approach to Bullying News Media: Partnering with Journalists
Click here for .pdf version of poster
Title: A Prevention Approach to Bullying News Media: Partnering with Journalists
Hyzer R; Bushman M; Pletta K; Moreno M
Background: Bullying remains a public health issue for teens and is related to negative health outcomes. Bullying news media, which often focuses on tragic cases, can leave teens feeling fearful and hopeless. An alternate approach may be to promote bullying prevention in news stories. The purpose of this study was to understand perspectives of journalists on incorporating prevention information in news stories about bullying and cyberbullying.
Design/Methods: We identified journalists who had covered youth-focused topics by reviewing published news stories on bullying and cyberbullying. Participants were recruited from a variety of sources, including print and online newspapers. Semi-structured interviews explored journalists’ experiences reporting on bullying and how journalists could incorporate bullying prevention in news media articles. Our qualitative analysis included three researchers creating a codebook to evaluate participants’ responses and collapsing codes into themes using the constant comparative method.
Results: A total of 20 journalists were interviewed who were 70% female, 80% Caucasian, with an average age of 42.7 (SD=12.06) years. Three main themes emerged. First, journalists expressed there are some aspects of reporting that are out of their control, such as the need to report details of a bullying incident, which may be inherently fearful. One excerpt stated, “It’s hard because you’re, it’s the media, you’re spreading the news about these things.” Second, many journalists proposed a solution to have a balance between details of the bullying incident and prevention information. A participant commented, “So you have to balance that. You have to find a way to address the situation in a sensitive manner and also find the compelling way to tell that story.” Third, journalists indicated interest in creating guidelines to identify practical ways to include prevention information in reporting. One participant said, “Back when suicide was such a weird topic to report on, and now there’s a template for how it’s done. You know that could be what to do for cyberbullying.”
Conclusions: Findings show that journalists are open to incorporating prevention information in bullying news media and interested in collaborating with researchers to create guidelines. Alongside public health and prevention organizations, researchers and journalists could create and disseminate guidelines that ensure that bullying news media address both details of the incident and prevention information.
Early Literacy Intervention For Infants With Congenital Heart Disease: A Pilot Study
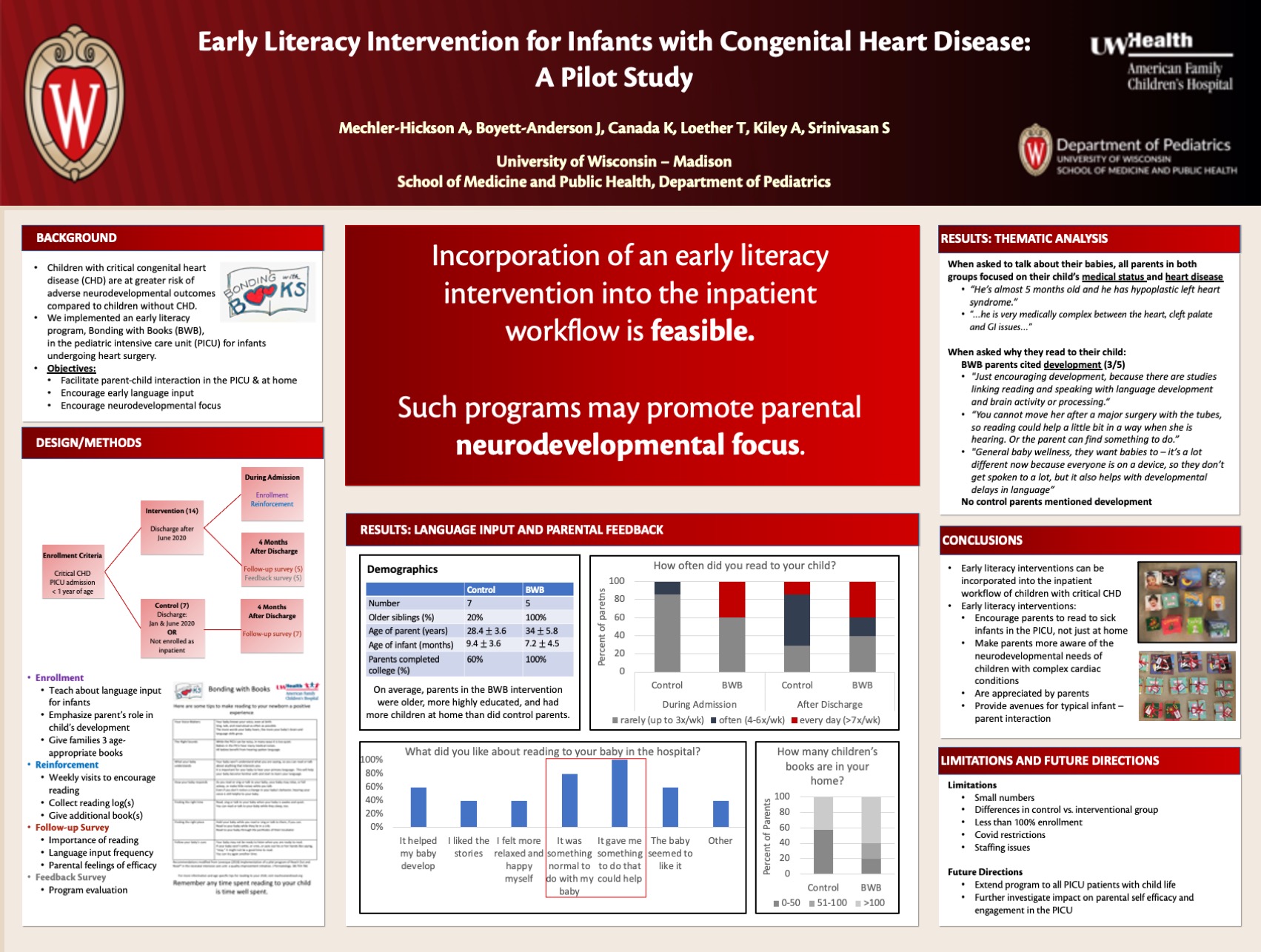
Click here for .pdf version of poster
Title: Early Literacy Intervention For Infants With Congenital Heart Disease: A Pilot Study
Mechler-Hickson A, Boyett-Anderson J, Canada K, Loether T, Kiley A, Srinivasan S
Background: Children with critical congenital heart disease (CHD) have an increased risk of adverse neurodevelopmental outcomes, including language delays, compared to children without heart disease. Parents of these children also often experience high levels of acute stress and feelings of helplessness. We implemented an early literacy intervention (Bonding with Books, BwB) for infants with critical CHD admitted to the pediatric intensive care unit (PICU) to increase early language input and encourage parental self-efficacy.
Design/Methods: Primary caregivers of patients under 1 year admitted to the PICU with critical CHD following June 2020 were eligible for enrollment. Program participants were educated on the benefits of language input on neurodevelopment, given weekly age-appropriate books to read with their child, encouragement and a log to record reading. Patients admitted prior to initiation of the program, and those not enrolled during their surgical hospitalization, were eligible to be enrolled as controls.
All participants were surveyed four months after discharge regarding their child’s hospital experience; their current sense of parental efficacy, stress and bonding; and literacy activities (reading, speaking, singing and rhyming) while hospitalized and after discharge. In the intervention group, data regarding language input and perceived parental efficacy, stress, and bonding were also collected at the time of enrollment.
Results: Thirteen families enrolled in the intervention and five completed follow up surveys. Seven control families completed follow up surveys. Parents who participated in the program reported increased reading frequency during hospitalization but no sustained increase in language input compared with control families post-discharge. Participating families reported being encouraged to read with their child by a healthcare provider more often (100%) than control families (43%) and recalled “development” as a reason to read. Program participants cited increased self-efficacy and normalcy as benefits of participation, and, on average, reported lower rates of helplessness and increased bonding on discharge from the hospital.
Conclusions: Participation in organized early literacy initiatives as a part of critical care of infants with complex CHD is feasible. Such small changes help increase language input and encourage earlier parental neurodevelopmental focus. Larger studies are needed to assess its impact on parental stress and bonding.
ECG Screening and Interpretation Patterns Among Physicians Performing Preparticipation Physical Evaluations (PPE)
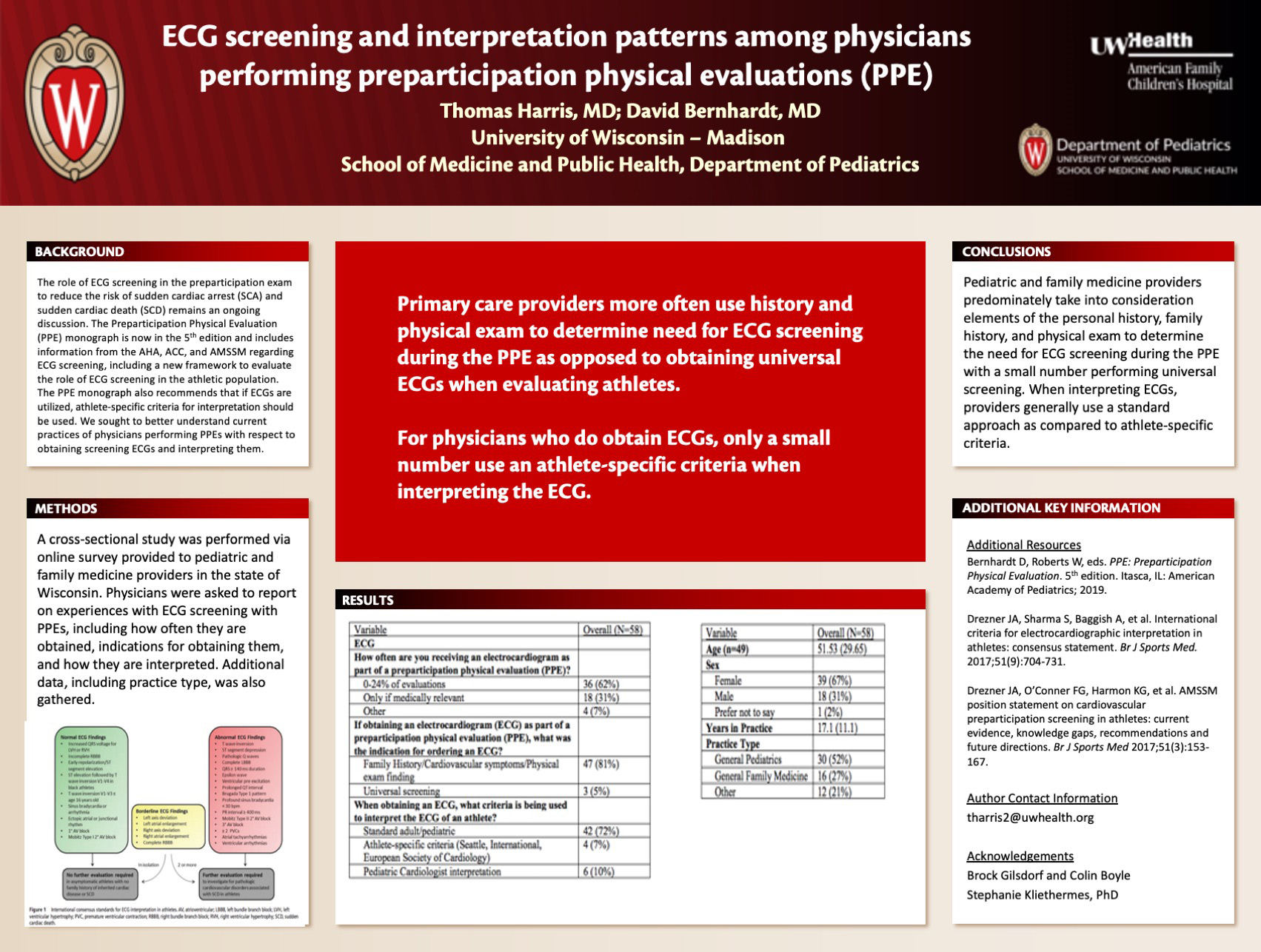
Click here for .pdf version of poster
Title: ECG Screening and Interpretation Patterns Among Physicians Performing Preparticipation Physical Evaluations (PPE)
Harris T, Bernhardt D
Background: The role of ECG screening in the preparticipation exam to reduce the risk of sudden cardiac arrest (SCA) and sudden cardiac death (SCD) remains an ongoing discussion. The Preparticipation Physical Evaluation (PPE) monograph is now in the 5th edition and includes information from the AHA, ACC, and AMSSM regarding ECG screening, including a new framework to evaluate the role of ECG screening in the athletic population. The PPE monograph also recommends that if ECGs are utilized, athlete-specific criteria for interpretation should be used. We sought to better understand current practices of physicians performing PPEs with respect to obtaining screening ECGs and interpreting them.
Design/Methods: A cross-sectional study was performed via online survey provided to pediatric and family medicine providers in the state of Wisconsin. Physicians were asked to report on experiences with ECG screening with PPEs, including how often they are obtained, indications for obtaining them, and how they are interpreted.
Results: Of 58 responses, 81% (n=47) of providers reported obtaining ECGs with a positive physical exam finding, family history, or reported symptoms during the PPE. 62% of respondents (n=36) estimated a frequency of obtaining ECGs with <25% of PPEs and an additional 31% (n=18) reported obtaining ECGs only when medically relevant. 5% (n=3) obtain ECGs universally with athletes. When interpreting EKGs, 72% (n=42) of respondents reported utilizing a standard approach to all EKGs while 7% (n=4) reported using athlete-specific criteria.
Conclusions: Pediatric and family medicine providers predominately take into consideration elements of the personal history, family history, and physical exam to determine need for ECG screening during the PPE with a small number performing universal screening. When interpreting ECGs, providers generally use a standard approach as compared to athlete-specific criteria.
Exploring The Discussion of Nexplanon (Etonogestrel Birth Control Implant) On Twitter
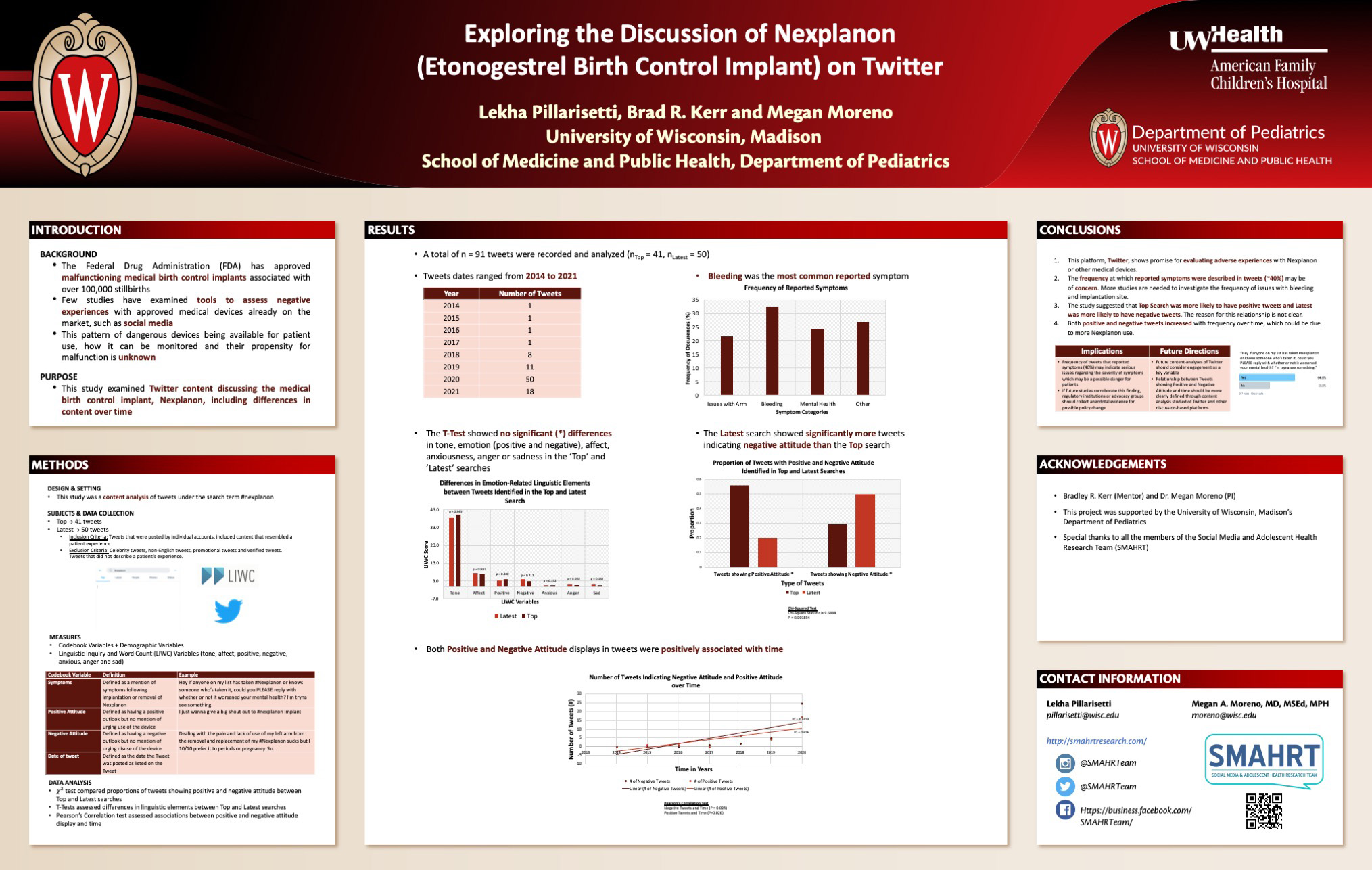
Click here for .pdf version of poster
Title: Exploring The Discussion of Nexplanon (Etonogestrel Birth Control Implant) On Twitter
Pillarisetti L, Kerr B, Moreno M
Background: The Federal Drug Administration (FDA) has approved fraudulent medical birth control implants associated with over 100,000 stillbirths. Few studies have examined tools to assess negative experiences with approved medical devices already on the market, such as social media. This study examined Twitter content discussing the medical birth control implant, Nexplanon, including differences in content over time.
Design/Methods: In this content analysis study, the first 50 public Tweets from the Top search (most popular) and the first 50 from the Latest search (most recent) using the hashtag #Nexplanon were evaluated. Tweets were excluded if they were not personal accounts or recounting a patient experience. Measures included any mention of side effects, positive and negative attitude toward Nexplanon, and date of tweet. The Linguistic Inquiry and Word Count program was used to assess the following linguistic elements: positive, negative, affect, anxiety, anger and sadness. A Chi-squared test compared proportions of Tweets showing positive and negative attitude between Top and Latest searches. T-Tests assessed differences in linguistic elements between Top and Latest categories. Pearson’s Correlation test assessed associations between positive and negative attitude display and time.
Results: A total of 91 Tweets were evaluated. Of the 37 Tweets (40%) that reported side effects associated with Nexplanon, 22% indicated issues with the implantation site (upper arm), 32% reported issues with lengthened/excessive bleeding period and 24% reported mental health problems. Tweets displaying positive attitude were more likely to be shown in the Top search (63%, n = 41) than the Latest search (28%, n = 43, 𝜒2 = 9.6888, p = .002). There were no significant differences in linguistic elements between Tweets in the Top and Latest searches. Tweets from more recent years were associated with increased positive attitude (r2 = 616, p = .03) and negative attitude (r2 = 0.5413, p = .02) references.
Conclusions: Increases in positive and negative attitude displays over time could be reflect increasing Nexplanon use. The finding that 32% of Tweets referenced excessive bleeding periods and 24% referenced mental health problems suggests a possibility of significant health concerns associated with Nexplanon. Future studies should examine the prevalence of these concerns among adolescents and young adults.
A Survey of Pediatric Cardiologists and Cardiac Surgeons on the Care of Congenitally Corrected Transposition of the Great Arteries (L-TGA)
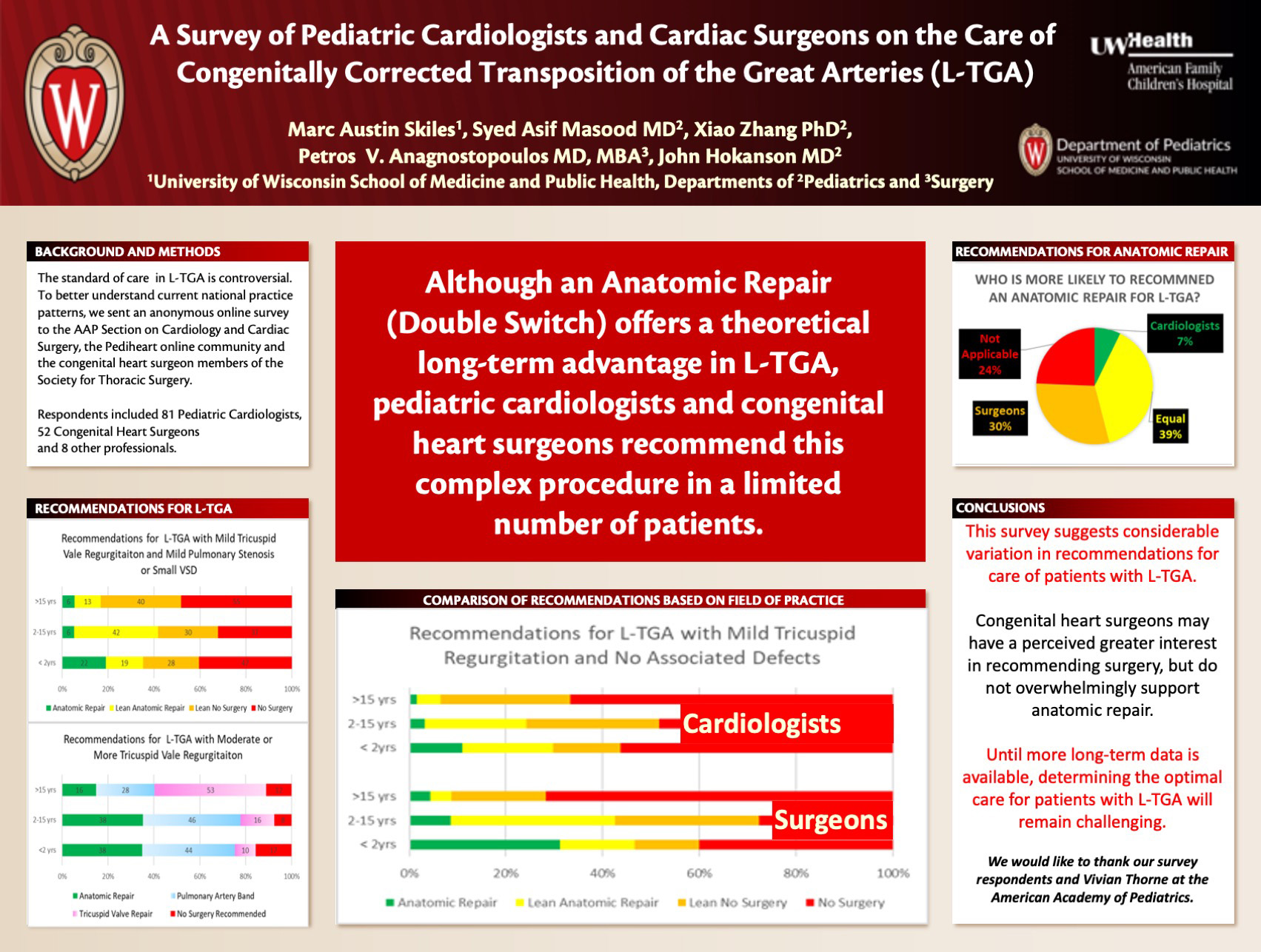
Click here for .pdf version of poster
Title: A Survey of Pediatric Cardiologists and Cardiac Surgeons on the Care of Congenitally Corrected Transposition of the Great Arteries (L-TGA)
Skiles M, Masood S, Anagnostopoulos P, Hokanson J
Background: Congenitally Corrected Transposition (L-TGA) is an uncommon form of congenital heart disease with a wide range of associated cardiac defects and disease severity. Consequently, the best course of treatment for patients with L-TGA remains unclear.
Design/Methods: We sent an anonymous electronic survey to members of the American Academy of Pediatrics Section on Cardiology and Cardiac Surgery and the Pediheart online community as well as the congenital heart surgeon members of the Society for Thoracic Surgery which addressed the management of L-TGA. We asked respondents their opinions regarding their surgical management of progressively complex variations of L-TGA at different ages and their general opinions on management of this disease.
Results: We received responses from 64 pediatric cardiologists and 47 congenital heart surgeons.
In the case of an asymptomatic patient with L-TGA with mild tricuspid insufficiency and no other associated defects, respondents leaned toward or recommended an anatomic repair (double switch operation) in 36.0% of children <2 years, 31.5% of children 2-15 years and 7.2% of patients over 15 years. In all age groups, surgeons were more likely to lean toward or recommend anatomic repair that cardiologists (45/138 (32.6%) of total recommendations v 38/189 (20.1%) of total recommendations).
If the same patient had mild pulmonary stenosis or a small ventricular septal defect, anatomic repair was considered in 34.2% of children <2 years, 40.5% of children 2-15 years and 15.3% of patients over 15 years.
When an asymptomatic patient with L-TGA had moderate or more tricuspid regurgitation but no other cardiac defects, anatomic repair was considered in 34.2% of children <2 years, 34.2% of children 2-15 years and 14.5% of patients over 15 years.
With regard to their clinical care in L-TGA, 7.2% felt cardiologists were more likely to recommend anatomic repair than surgeons, 28.7% felt surgeons were more likely to recommend anatomic repair than cardiologists.
8.1% felt extremely comfortable, 53.2% felt somewhat comfortable, 27.9% were neither comfortable nor uncomfortable, 14.4% were somewhat uncomfortable and 6.3% were extremely uncomfortable with their care recommendations for patients with L-TGA.
Conclusions: There was considerable variation and a certain degree of discomfort to providers regarding their clinical recommendations made by cardiovascular providers for children with L-TGA.
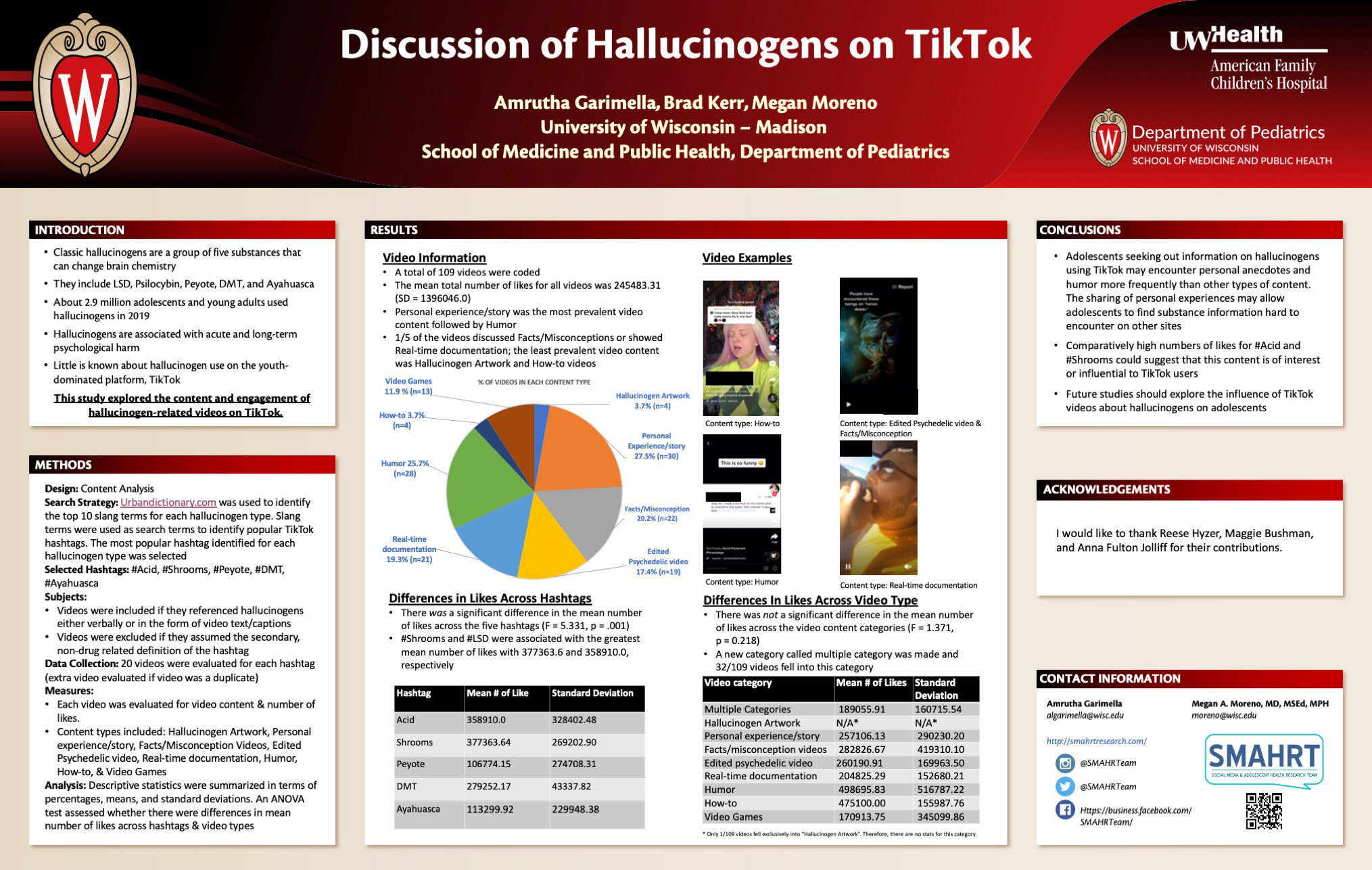
Discussion of Hallucinogens (LSD, Psilocybin, Peyote, DMT, And Ayahuasca) On TikTok
Click here for .pdf version of poster
Title: Discussion of Hallucinogens (LSD, Psilocybin, Peyote, DMT, And Ayahuasca) On TikTok
Garimella A., Kerr B., Moreno M.
Background: About 2.9 million adolescents and young adults used hallucinogens in 2019. Hallucinogens are associated with acute and long-term psychological harm. Little is known about the discussion of hallucinogen use on the youth-dominated platform, TikTok. This study explored the content and engagement of hallucinogen-related videos on TikTok.
Design/Methods: In this content analysis study, the most popular TikTok hashtag associated with LSD (#Acid), Psilocybin (#Shrooms), Peyote (#Peyote), DMT (#DMT), and Ayahuasca (#Ayahuasa) was determined. The first 20 videos located within each hashtag were evaluated. Videos that referenced hallucinogens either explicitly or implicitly were included. Videos were evaluated for the presence of content such as Personal experience/story, Humor, Fact/Misconception, Real-time Documentation, Hallucinogen Artwork and How-to. Additionally, the number of likes for each video was recoded. ANOVA tests compared mean likes between videos from different hashtags and video types.
Results: A total of 109 TikTok videos were coded. Personal experience/story was the most prevalent video content (n = 30, 27.5%) followed by Humor (n = 28, 25.7%). About a fifth of the videos discussed Facts/Misconceptions (n=22, 20.2%) or showed Real-time Documentation (n=21, 19.3%). The least prevalent video content was Hallucinogen Artwork (n=4, 3.7%) and How-to videos (n=4, 3.7%). Mean likes across all videos was 245483.31 (SD = 282869.572). There was a significant difference in the mean number of likes across the five hashtags (F = 5.331, p = .001). #Shrooms and #LSD were associated with the greatest mean number of likes with 377363.6 (SD= 269202.9) and 358910.0 (SD= 328402.5), respectively. However, there was not a significant difference in the mean number of likes across the video content categories (F = 1.371, p = 0.218).
Conclusions: Adolescents seeking out information on hallucinogens using TikTok may encounter personal anecdotes and humor more frequently than other types of content. Future studies should explore the influence of TikTok videos about hallucinogens on adolescents.
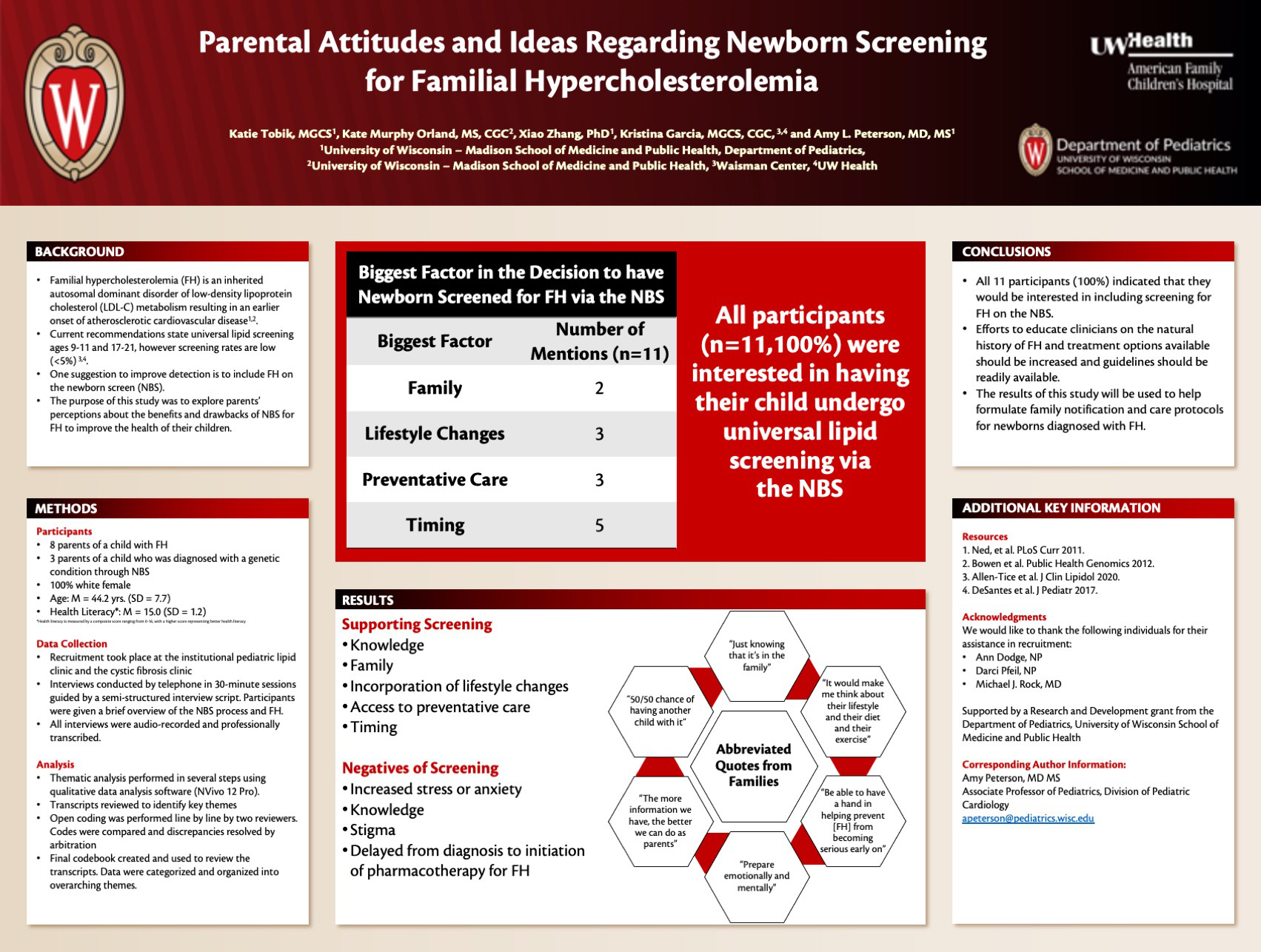
Parental Attitudes and Ideas Regarding Newborn Screening for Familial Hypercholesterolemia
Click here for .pdf version of poster
Title: Parental Attitudes and Ideas Regarding Newborn Screening for Familial Hypercholesterolemia
Tobik K, Orland K, Zhang X, Garcia K, and Peterson AL
Background: Familial hypercholesterolemia (FH) is an inherited disorder of low-density lipoprotein cholesterol (LDL-C) metabolism that affects approximately 1 in 200-300 people. Current screening rates for FH in childhood are very low, despite recommendations for universal cholesterol screening in childhood. One suggestion to improve screening rates is to add cholesterol screening to the newborn screening (NBS) process as part of a multifaceted approach to screening for FH. Previous research has shown that parents are in favor of screening for FH during childhood. However, very little is known regarding parent opinions on screening for FH during the newborn period. This study aims to identify themes involving possible benefits, harms, and ethical concerns that could arise from adding screening for Familial Hypercholesterolemia (FH) to the newborn screen (NBS) and assess acceptability of NBS for FH.
Design/Methods: Personal interviews were conducted to identify perspectives regarding NBS for FH from two groups: 1) parents of children diagnosed with FH, and 2) parents who have gone through a screen-positive NBS experience. Stratified purposive sampling was used to ensure adequate representation. The interviews were conducted via telephone in 30-minute sessions guided by a semi-structured interview script. At the beginning of the interview, participants were educated on the NBS process and FH.
Results: Of the 11 participants interviewed, 11 (100%) indicated that they would be interested in having their child undergo universal cholesterol screening via NBS. Reasons supporting screening during the newborn period included knowledge, family, incorporation of lifestyle changes, access to preventative care, and timing. Negatives surrounding screening during the newborn period included various emotions, increased stress or anxiety, knowledge, stigma, and the delay before pharmacotherapy is started to treat FH.
Conclusions: While these interviewees were in favor of NBS for universal lipid screening, further education of parents and clinicians is needed to ensure proper implementation. The results of this study may be useful to formulate family notification and care protocols for newborns diagnosed with FH and other diseases.
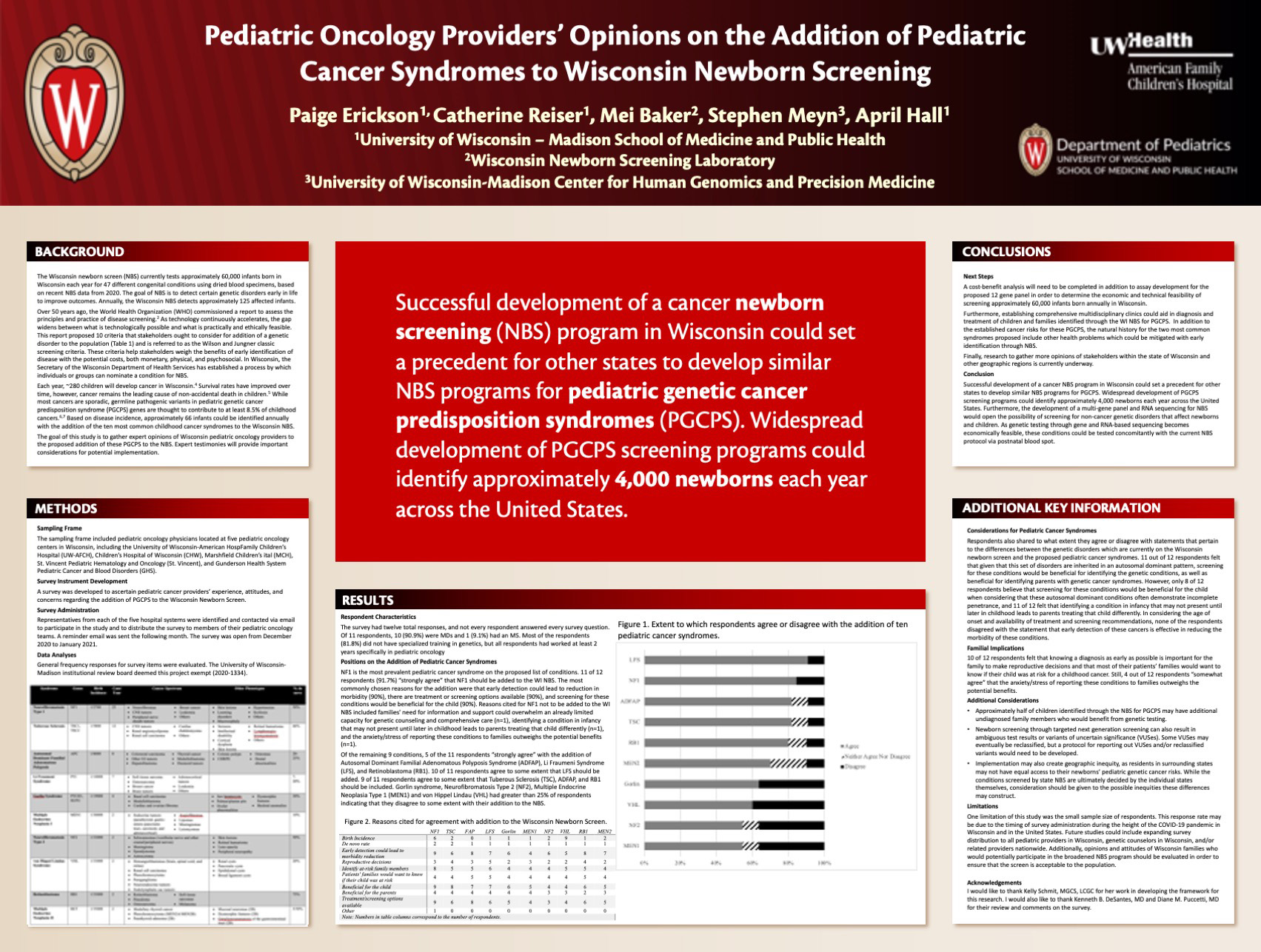
Pediatric Oncology Providers Opinions on the Addition of Pediatric Cancer Syndromes to Wisconsin Newborn Screening
Click here for .pdf version of poster
Title: Pediatric Oncology Providers Opinions on the Addition of Pediatric Cancer Syndromes to Wisconsin Newborn Screening
Erickson P, Reiser C, Baker M, Meyn S, Hall A
Background: Wisconsin’s Newborn Screening Program (NBS) currently tests 65,000 infants born in Wisconsin each year for 44 different disorders and detects ~120 affected infants.1 The goal of NBS is to detect certain genetic disorders early in life in order to direct management and improve outcomes. As technology continuously accelerates, the gap widens between what is technologically possible and what is practically and ethically feasible. Based on disease incidence, it is estimated that 66 more infants could be identified annually with the addition of the ten most common childhood cancer syndromes to the Wisconsin NBS.
Design/Methods: We surveyed healthcare professionals working in the field of pediatric oncology at five centers in Wisconsin. The survey included questions collecting demographic information and experience/knowledge with genetics and pediatric cancer syndromes as well as Likert scales addressing the four areas where the proposed pediatric cancer syndromes are different from the genetic disorders which are currently on the Wisconsin newborn screen (inheritance, penetrance, disease onset and family implications).
Results: 12 providers responded to the survey. 91% of providers agree that early detection of these cancer conditions is effective in reducing the morbidity of these conditions, and for each condition, most providers agreed with the addition of the pediatric cancer syndrome to the Wisconsin NBS.
Conclusions: Successful development of a cancer NBS program in Wisconsin could identify an estimated 66 infants with pediatric cancer syndromes each year. Expert testimonies will provide important considerations for inclusion of pediatric cancer conditions on the WI NBS.
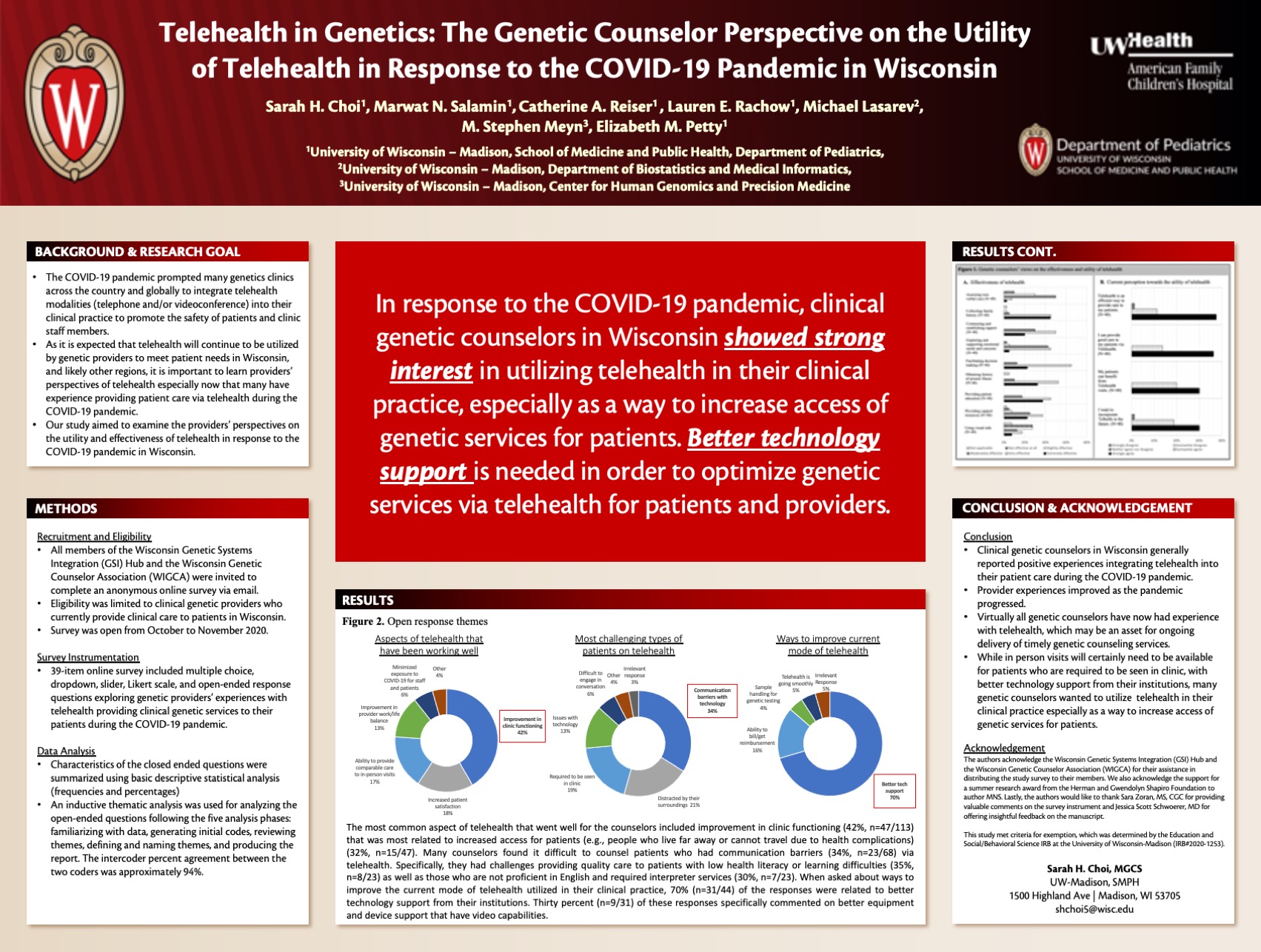
Telehealth in Genetics: The Genetic Counselor Perspective on the Utility of Telehealth in Response to the Covid-19 Pandemic in Wisconsin
Click here for .pdf version of poster
Title: Telehealth in Genetics: The Genetic Counselor Perspective on the Utility of Telehealth in Response to the Covid-19 Pandemic in Wisconsin
Choi S, Salamin M, Reiser C, Rachow L, Lasarev M, Meyn M, Petty E
Background: Due to the COVID-19 pandemic, many genetics clinics across the country were prompted to integrate telehealth delivery modalities into their clinical practice either by telephone, videoconferencing, or a combination of both to promote the safety of patients and clinic staff members. Our study aimed to examine the providers’ perspectives on the utility of telehealth clinic visits in response to the COVID-19 pandemic in Wisconsin.
Design/Methods: An anonymous Qualtrics survey was distributed via email to all members of the Wisconsin Genetic Systems Integration Hub and the Wisconsin Genetic Counselor Association. Current clinical genetic providers were eligible to participate in the survey. The survey assessed the providers’ experiences as well as perceptions towards utilizing telehealth in delivering clinical genetic services to their patients during the pandemic.
Results: A total of 47 currently practicing clinical genetic counselors in Wisconsin responded to the survey. Almost all of them somewhat (23%) or strongly (75%) agreed to wanting to incorporate telehealth in the future. The most common aspect of telehealth that went well for the counselors included improvement in clinic functioning. The most common types of patients that they found most challenging were patients who had communication barriers. Better technology support was noted to be the most common response when asked about ways to improve the current mode of telehealth modalities utilized in their clinical practice.
Conclusions: Clinical genetic counselors in Wisconsin generally had a positive experience utilizing telehealth during the COVID-19 pandemic. With better technology support from their institutions, many seemed to be interested in utilizing telehealth in their clinical practice especially as a way to increase access of genetic services for patients.
Session B: Bench & Translational
| Time | Presenter | Title |
|---|---|---|
| 3:30-3:39 | Alisha Ching, MD | Hepatic Adenoma is Associated with Turner Syndrome |
| 3:39-3:48 | Vishwanatha Chandrahas | Relationship between magnitude maternal antibody response to ZIKV infection and plasma viremia duration |
| 3:48-3:57 | Fernanda Szewc | Alpha-tocopheryloxyacetic acid induces apoptosis of murine rhabdomyosarcoma in vitro while modulating innate and adaptive immune responses in vivo |
| 3:57-4:06 | Margaret Hackett | Assessing Fear and Anxiety Response in Mice Following Neonatal Hypoxic Ischemic Encephalopathy |
| 4:06-4:15 | Nida Karahan Keles | Role of Nuclear Estrogen Receptor Alpha in TRKB Signaling Following Neonatal Hypoxic Ischemic Encephalopathy |
| 4:15-4:24 | Katie Beverley | Side-Chain Polarity of Amino Acids within the Kir7.1 Channel Pore Lining Determine Permeability and Function |
| 4:24-4:33 | Matthew Forsberg | Human monocytes educated with exosomes from TLR4 primed mesenchymal stem cells treat acute radiation syndrome by promoting hematopoietic recovery |
| 4:33-4:42 | Lauren Hlubek | Structural Brain Imaging in Infant Macaques Exposed to Zika Virus Prenatally |
| 4:42-4:51 | Nicholas Mohrdieck | An immune co-stimulatory vaccine, with adoptive transfer of natural killer cells and immune inhibition blockade, after allogeneic bone marrow transplant, delays and reduces neuroblastoma tumor growth |
| 4:51-5:00 | Meha Kabra | CRISPR base editing as a potential therapeutic approach for Kir7.1 channelopathy |
| 5:00 | Wrap-Up |
This is an accordion element with a series of buttons that open and close related content panels.
Hepatic Adenoma is Associated with Turner Syndrome
Click here for .pdf version of poster
Title: Hepatic Adenoma is Associated with Turner Syndrome
Ching A, Zhang X, Furuya K, Bartlett H
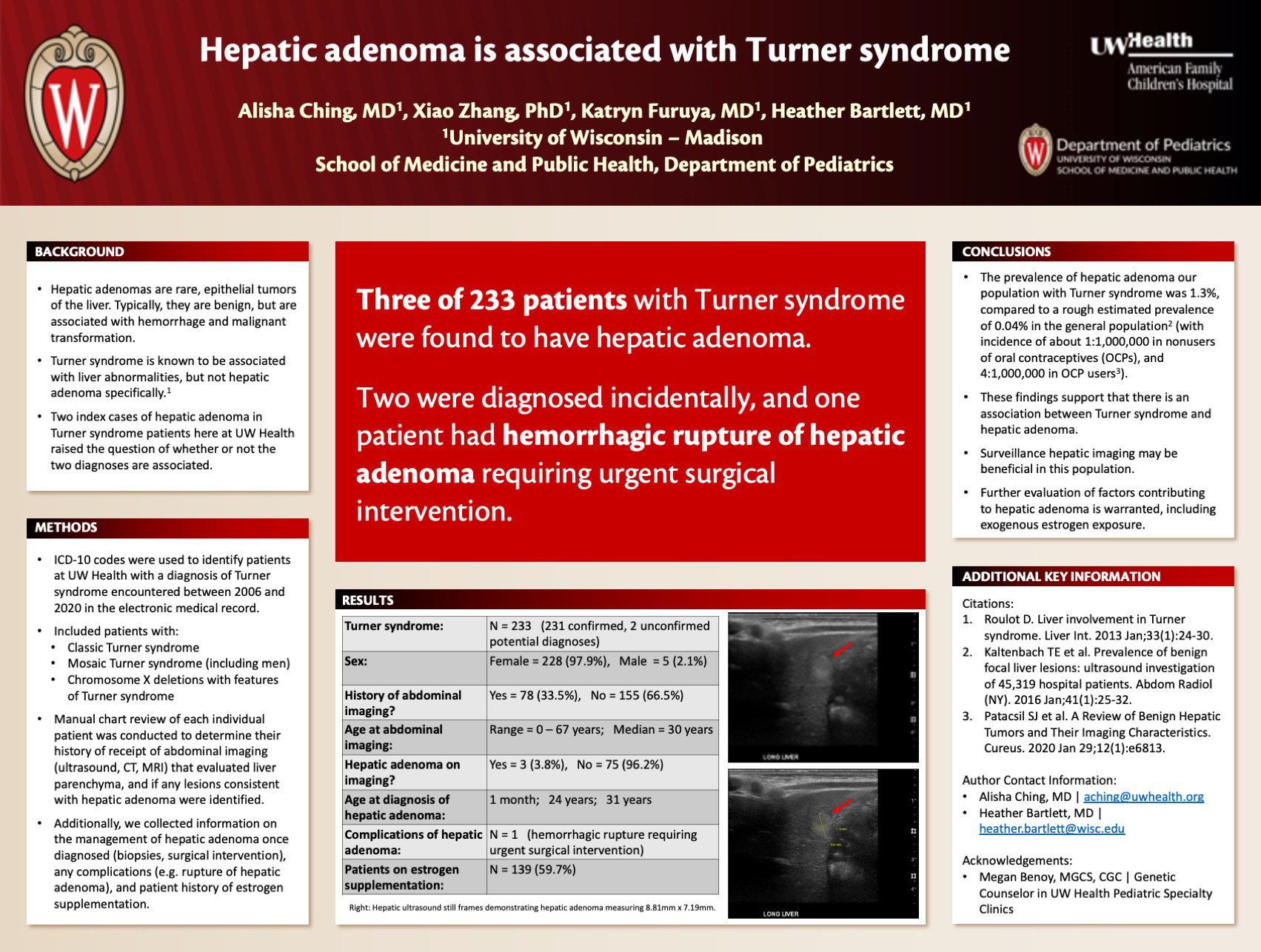
Background: Hepatic adenomas are rare, epithelial tumors of the liver. Although benign, they are associated with hemorrhage and malignant transformation. Two index cases of hepatic adenoma in patients with Turner syndrome raised the question of whether or not the diagnoses are associated. We hypothesized that Turner syndrome is associated with an increased incidence of hepatic adenoma.
Design/Methods: ICD–10 codes were used to identify all UW Health patients with a diagnosis of Turner syndrome encountered between 2006 and 2020 in the electronic medical record. Patients with mosaic Turner syndrome and partial X chromosome deletions with Turner syndrome features were included in our study. Manual chart review of each individual patient was conducted to identify if they had ever received abdominal imaging (CT, MRI, ultrasound) which included evaluation of their liver. We examined the imaging reports to determine if the radiologist had identified lesions in the liver consistent with hepatic adenoma. We also noted if and when the patients had received estrogen supplementation.
Results: A search of UW Health’s electronic medical record database identified 231 patients with a diagnosis of Turner syndrome. Of these patients, 78 have had abdominal imaging, and three of them were noted to have hepatic adenomas. Of the three patients with hepatic adenomas, two were found incidentally on abdominal imaging, and one patient was identified as having a hepatic adenoma after it ruptured and caused severe hemorrhage. Two of these three patients had been on estrogen supplementation prior to diagnosis of hepatic adenoma.
Conclusions: The incidence of hepatic adenoma in our Turner syndrome patients is about 1.3% over 14 years, acknowledging that only about a third of the patients have received abdominal imaging, so this may be an underestimate. This is much higher than the incidence of hepatic adenoma in the general population, including oral contraceptive users (0.056%). These data suggest an association between Turner syndrome and hepatic adenoma.
Relationship Between Magnitude Maternal Antibody Response to ZIKV Infection and Plasma Viremia Duration
Click here for .pdf version of poster
Title: Relationship Between Magnitude Maternal Antibody Response to ZIKV Infection and Plasma Viremia Duration
Chandrahas V, Mohr E
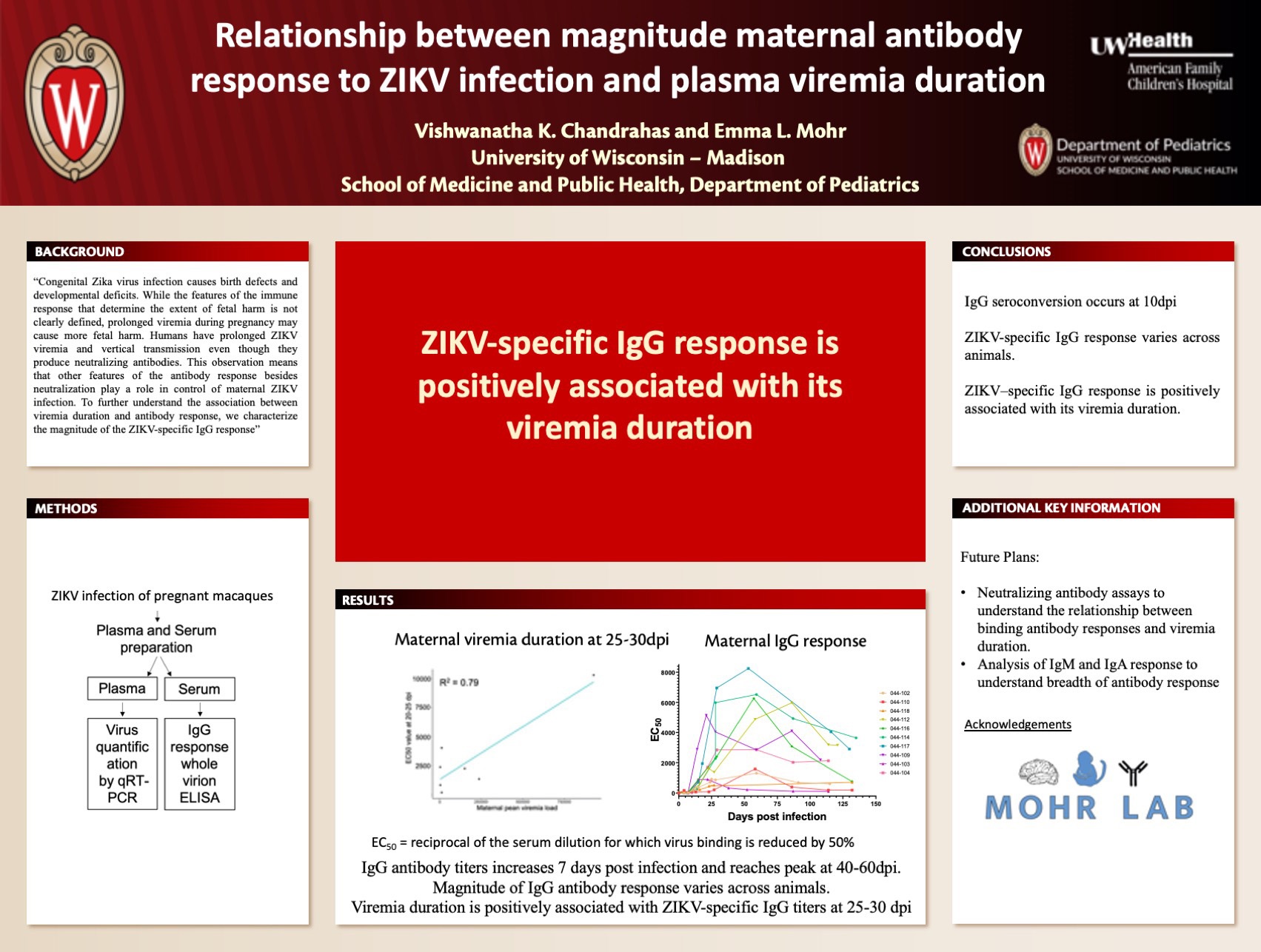
Background: Congenital Zika virus infection causes birth defects and developmental deficits. While the features of the immune response that determine the extent of fetal harm is not clearly defined, prolonged viremia during pregnancy may cause more fetal harm. Humans have prolonged ZIKV viremia and vertical transmission even though they produce neutralizing antibodies. This observation means that other features of the antibody response besides neutralization play a role in control of maternal ZIKV infection. To further understand the association between viremia duration and antibody response, we characterize the magnitude of the ZIKV-specific IgG response.
Design/Methods: Blood samples were collected from pregnant macaques at several time points before and after ZIKV infection until the day of delivery. We quantified the magnitude of ZIKV-specific IgG antibodies by measuring binding to whole ZIKV virions in an ELISA. We calculated the inhibitory concentration 50 (EC50), which is defined as reciprocal of the serum dilution for which virus binding is reduced by 50%, for each timepoint. Maternal viremia was assessed by qRT-PCR, and viremia duration was defined as the last day of positive viral load.
Results: Our study showed that the IgG antibody response is near background level until 7 days post infection (dpi). After 7dpi, EC50 values increased and reached peak magnitude at 40-60dpi indicating that highest amount of IgG antibodies are produced between 40 and 60 dpi. Magnitude of IgG antibody response was also found to be highly variable across animals. Viremia duration was positively associated with ZIKV-specific IgG titers at 25-30 dpi (R2 = 0.95).
Conclusions: In conclusion, we found that IgG seroconversion occurs at 10dpi and that there is significant variability in an animal’s ZIKV-specific IgG response. The finding that animal’s ZIKV–specific IgG response is positively associated with its viremia duration is interesting and neutralizing antibody assays are planned to further understand the relationship between binding antibody responses and viremia duration.
Alpha-Tocopheryloxyacetic Acid Induces Apoptosis of Murine Rhabdomyosarcoma in Vitro while Modulating Innate and Adaptive Immune Responses in Vivo
Click here for .pdf version of poster
Title: Alpha-Tocopheryloxyacetic Acid Induces Apoptosis of Murine Rhabdomyosarcoma in Vitro while Modulating Innate and Adaptive Immune Responses in Vivo
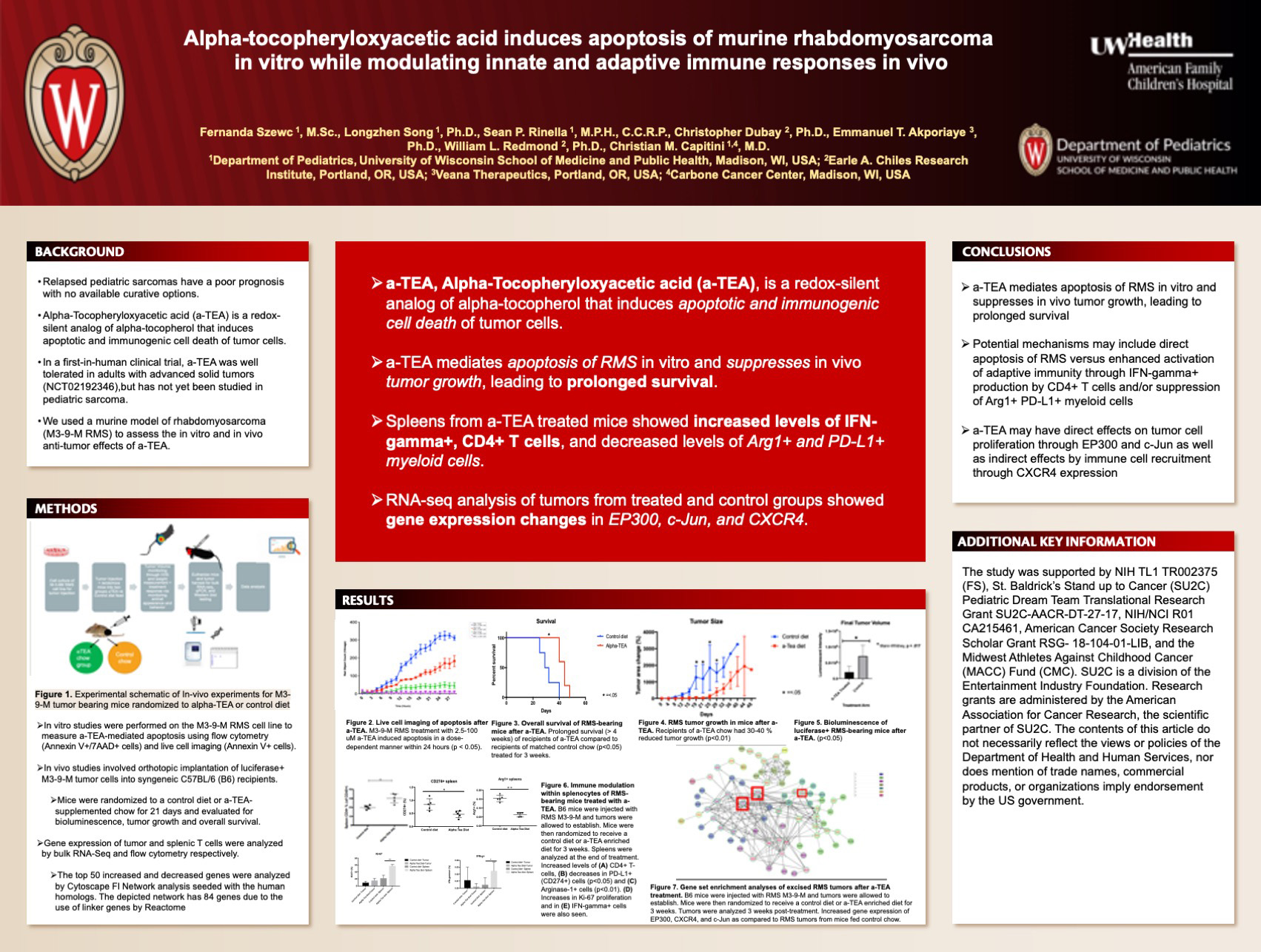
Szewc F, Song L, Rinella S, Dubay C, Akporiaye E, Redmond W, Capitini C
Background: Relapsed pediatric sarcomas have a poor prognosis with no available curative options. Alpha-Tocopheryloxyacetic acid (a-TEA) is a redox-silent analog of alpha-tocopherol that induces apoptotic and immunogenic cell death of tumor cells at doses that are not harmful to healthy normal cells. In a first-in-human clinical trial, a-TEA was well tolerated in adults with advanced solid tumors (NCT02192346), but has not yet been studied in pediatric sarcoma. We used a murine model of rhabdomyosarcoma (M3-9-M RMS) to assess the in vitro and in vivo anti-tumor effects of a-TEA.
Design/Methods: In vitro studies were performed on the M3-9-M RMS cell line to measure a-TEA-mediated apoptosis using flow cytometry (Annexin V+/7AAD+ cells) and live cell imaging (Annexin V+ cells). In vivo studies involved orthotopic implantation of luciferase+ M3-9-M tumor cells into syngeneic C57BL/6 recipients. Once tumors were palpable, mice were randomized to a control diet or a-TEA supplemented chow for 21 days and evaluated for bioluminescence, tumor growth and overall survival. Gene expression of tumor infiltrating and splenic T cells were analyzed by bulk RNA-Seq and flow cytometry respectively.
Results: M3-9-M RMS treatment with 2.5-100 uM a-TEA induced apoptosis in a dose-dependent manner within 24 hours (p < 0.05) as measured by flow cytometry and live cell imaging. In-vivo studies with the M3-9-M RMS mouse model showed that recipients of a-TEA chow had 30-40 % reduced tumor growth (p<0.01) and bioluminescence (p<0.05), leading to prolonged survival (> 4 weeks) compared to recipients of matched control chow (p<0.05). Spleen cells isolated from a-TEA-fed tumor-bearing mice demonstrated increased levels of IFN??+ cells, CD4+ T-cells, Ki-67 proliferation, and decrease in splenic CD11b+ arginase-1+ (p<0.01) and PD-L1+ cells (p<0.05) compared to their counterparts on the control diet. Gene set enrichment analyses of excised RMS tumors after a-TEA treatment revealed increased gene expression of CD24, EP300, CXCR4, and c-Jun as compared to tumors from mice fed control chow.
Conclusions: These data indicate that a-TEA mediates apoptosis of RMS in vitro and suppresses in vivo tumor growth, leading to prolonged survival likely via enhanced activation of adaptive immunity through CD4+ T cells and suppression of innate immunity through regulation of myeloid cell subsets. Furthermore, a-TEA may have direct effects on tumor cell proliferation through EP300 and c-Jun as well as indirect effects on tumor growth by regulation of immune cell recruitment through CD24 and CXCR4 gene expression. Administration of a-TEA as a potential salvage treatment for RMS is warranted.
Assessing Fear and Anxiety Response in Mice Following Neonatal Hypoxic Ischemic Encephalopathy
Click here for .pdf version of poster
Title: Assessing Fear and Anxiety Response in Mice Following Neonatal Hypoxic Ischemic Encephalopathy
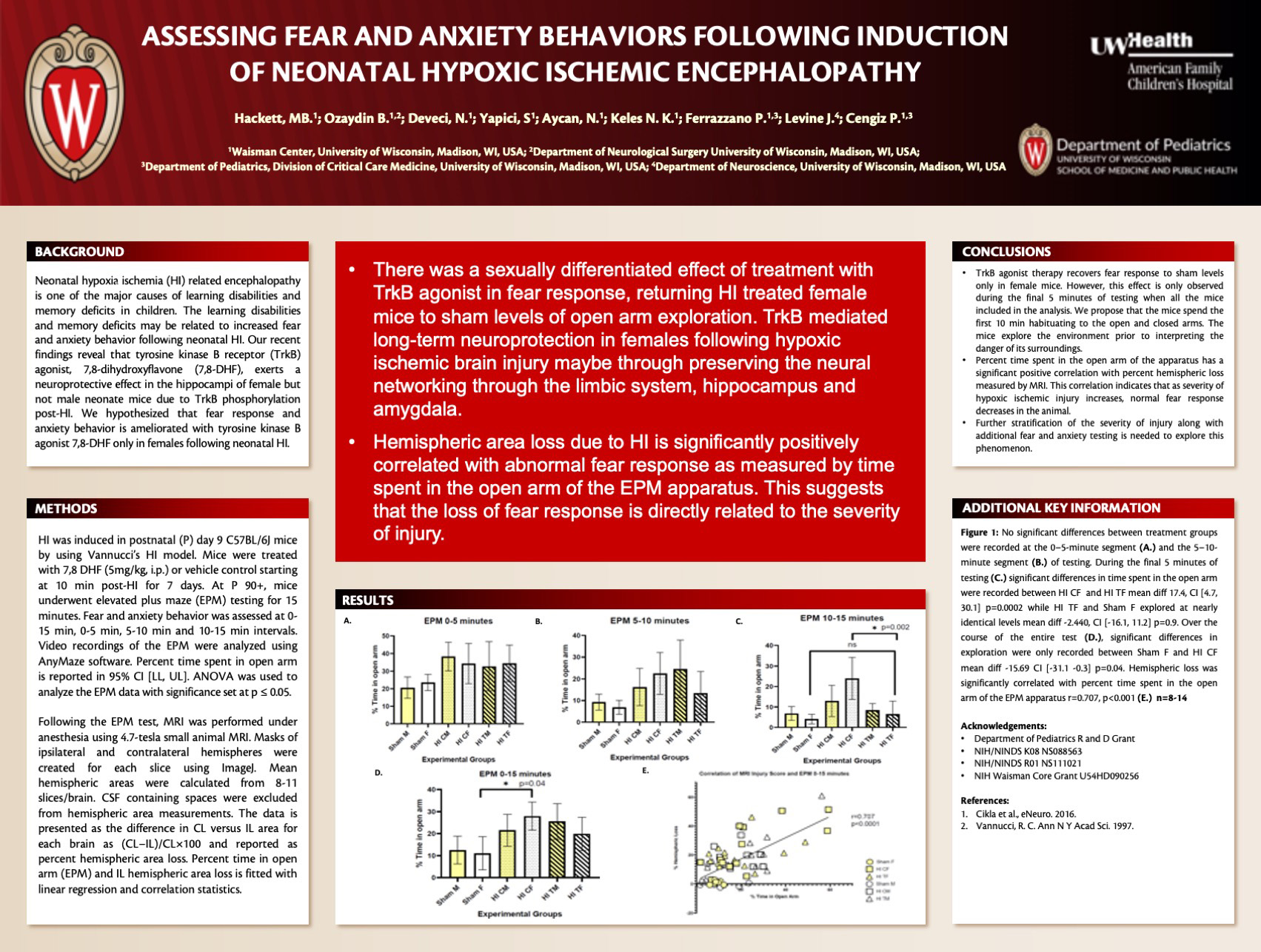
Hackett M, Ozaydin B, Deveci N, Yapici S, Aycan N, Karahan Keles N, Lagoa Miguel C, Corcoran K, Ferrazzano P, Levine J, Cengiz P
Background: Neonatal hypoxia ischemia (HI) related encephalopathy is one of the major causes of learning disabilities and memory deficits in children. The learning disabilities and memory deficits maybe related to the increased fear and anxiety behavior following neonatal HI. We hypothesized that fear response and anxiety behavior is ameliorated with tyrosine kinase B agonist 7,8-dihydroxyflavone (7,8-DHF) following neonatal HI.
Design/Methods: HI was induced in postnatal (P) day 9 C57BL/6J mice by using Vannucci’s HI model. Mice were treated with 7,8 DHF (5mg/kg, i.p.) or vehicle control starting at 10 min post-HI for 7 days. At P 90+, mice underwent elevated plus maze (EPM) testing for 15 minutes. Video recordings of the EPM were analyzed using AnyMaze software. Percent time spent in open arm is reported in mean ± SEM. ANOVA was used to analyze the EPM data. MRI was performed under anesthesia following EPM testing using 4.7-tesla small animal MRI. Masks of ipsilateral and contralateral hemispheres were created for each slice using ImageJ. Hemispheric areas were calculated from 8-11 slices/brain and averaged. CSF is excluded from hemispheric area measurements. The data is presented as the difference in CL area versus IL area for each brain as (CL−IL)/CL×100 and reported as IL hemispheric area loss. Percent time in open arm (EPM) and IL hemispheric area loss is fitted with linear regression.
Results: Significant differences in percent time spent in open arm of the EPM test indicate differing fear response between treatment groups (p= 0.013). HI mice exhibited abnormal fear response and TrkB agonist treatment rescued abnormal fear response only in female mice (19±1) versus the male mice (25±3) (p=0.034). Hemispheric area loss correlated with percent time spent in open arm.
Conclusions: HI mice preferred the open arms of the testing apparatus indicating a lack of fear response in compared to sham mice. 7,8 DHF recovered the fear response in female mice to the sham levels but not in male mice 90 days post-HI. This data suggests that TrkB agonist therapy restores the normal fear response and decreases anxiety in female mice exposed to perinatal HI and tested in early adulthood.
Role of Nuclear Estrogen Receptor Alpha in TrkB Signaling Following Neonatal Hypoxic Ischemic Encephalopathy
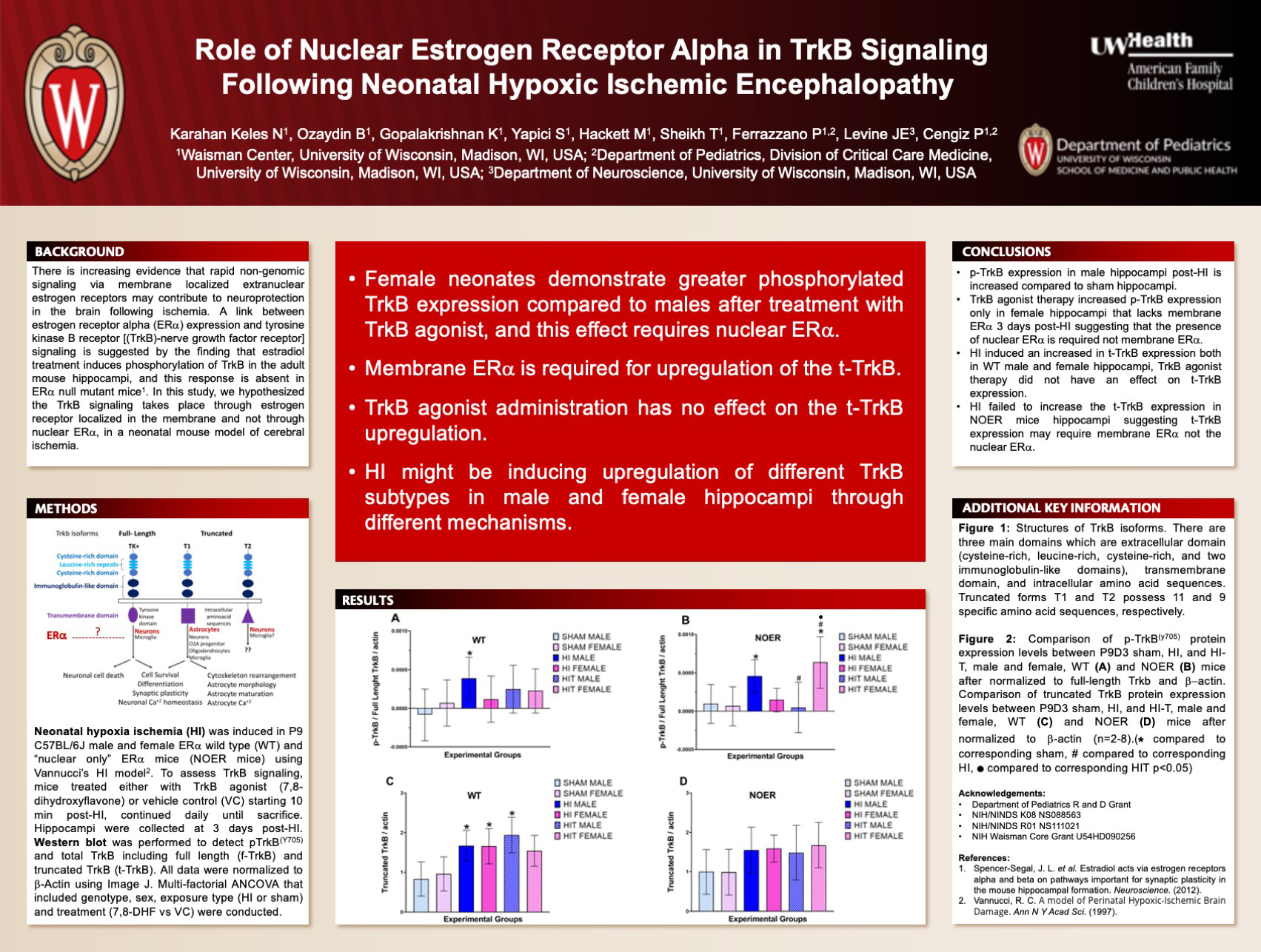
Click here for .pdf version of poster
Title: Role of Nuclear Estrogen Receptor Alpha in TrkB Signaling Following Neonatal Hypoxic Ischemic Encephalopathy
Karahan Keles N, Ozaydin B, Gopalakrishnan K, Yapici S, Hackett M, Sheikh T, Ferrazzano P, Levine JE, Cengiz P
Background: There is increasing evidence that rapid nongenomic signaling via membrane localized extranuclear estrogen receptors may contribute to neuroprotection in the brain. A link between estrogen receptor (ER) alpha expression and tyrosine kinase B receptor (TrkB-nerve growth factor receptor) signaling is suggested by the finding that estradiol treatment induces phosphorylation of TrkB in the adult mouse hippocampi, and this response is absent in ER alpha null mutant mice. In this study, we hypothesized the TrkB signaling takes place through estrogen receptor localized in the membrane and lacks in the mice that express estrogen receptor only in the nucleus in a neonatal mouse model of cerebral ischemia.
Design/Methods: Cerebral ischemia was induced in P9 C57BL/6J male and female ER alpha wild type (WT) and ER alpha knock-in mice that express mutant ER alpha that are incapable of membrane-initiated signaling, but maintain the capacity to regulate target gene expression in the nucleus: the “nuclear only” ER alpha mice (NOER mice) using Vannucci’s hypoxia ischemia (HI) model. Mice were either treated with TrkB agonist (7,8-dihydroxyflavone) or vehicle control starting from 10 min post-HI then daily for 2 days until sacrifice. The hippocampi were collected at 3 days post-HI. pTrkB (Y705), total TrkB including full length and truncated TrkB were quantified after being normalized to -Actin using western blotting. Multi-factorial ANOVA that included genotype, sex, exposure type (HI or sham) and treatment (VC vs. 7,8-DHF) were conducted.
Results: Our preliminary results suggest that HI induced robust truncated TrkB (t-TrkB) protein expression in both WT male and female hippocampi 3 days post-HI compared to sham mice. There was a tendency for ischemic WT female hippocampi to have higher t-TrkB expression compared to male hippocampi. Treatment with TrkB agonist decreased the t-TrkB expression in WT female but not in WT male hippocampi. t-TrkB expression post-HI was attenuated in NOER mice hippocampi and TrkB agonist increased t-TrkB expression in ischemic NOER female hippocampi.
Conclusions: t-TrkB regulates the function of reactive astrocytes following cerebral ischemia. Our results suggest that TrkB agonist therapy maybe regulating the t-TrkB in a sexually differential manner post-HI. Lacking membrane ER alpha reverses this response. The role of truncated TrkB and membrane-initiated ER alpha signaling in astrogliosis and neuroinflammation need to be further studied in developing brains following cerebral ischemia.
Identification And Function Of A CD4+/CD8αβ+ T Cell Population That is Predictive of GVHD Development in a Xenogeneic Transplant Model
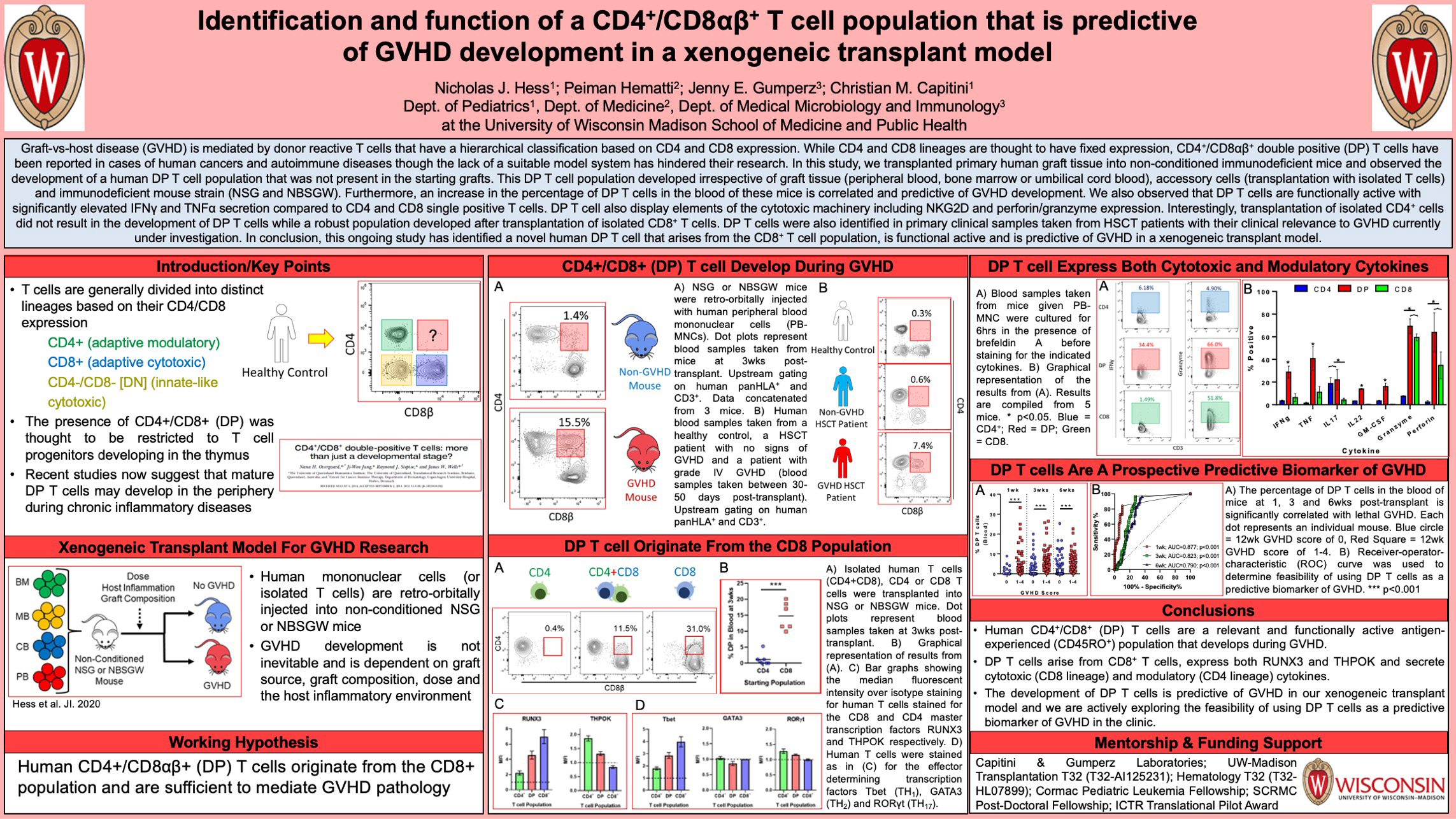
Click here for .pdf version of poster
Title: Identification And Function Of A CD4+/CD8αβ+ T Cell Population That is Predictive of GVHD Development in a Xenogeneic Transplant Model
Hess, NJ, Hematti, P, Gumperz, JE, Capitini, CM
Background: Graft-vs-host disease (GVHD) is mediated by donor reactive T cells that have a hierarchical classification based on CD4 and CD8 expression. While CD4 and CD8 lineages are thought to have fixed expression, CD4+/CD8αβ+ double positive (DP) T cells have been reported in cases of human cancers and autoimmune diseases though the lack of a suitable model system has hindered their research.
Design/Methods: Primary human graft tissue was transplanted into non-conditioned NSG or NBSGW immunodeficient mice. Mice were bled at regular intervals to monitor T cell activity. Graft sources include healthy peripheral blood, bone marrow, G-CSF mobilized peripheral blood and umbilical cord blood.
Results: We observed the development of a human DP T cell population that was not present in the starting grafts. This DP T cell population developed irrespective of graft tissue (peripheral blood, bone marrow or umbilical cord blood), accessory cells (transplantation with isolated T cells) and immunodeficient mouse strain (NSG and NBSGW). Furthermore, an increase in the percentage of DP T cells in the blood of these mice is correlated and predictive of GVHD development. We also observed that DP T cells are functionally active with significantly elevated IFNγ, TNFα, IL-17 and IL-22 secretion compared to CD4 and CD8 single positive T cells. DP T cell also display elements of the cytotoxic machinery including NKG2D and perforin/granzyme expression. Interestingly, transplantation of isolated CD4+ cells did not result in the development of DP T cells while a robust population developed after transplantation of isolated CD8+ T cells. Transcription factor staining confirmed that DP T cells express both the CD4 and CD8 master transcription factors THPOK and RUNX3 respectively. DP T cells were also identified in primary clinical samples taken from HSCT patients with their clinical relevance to GVHD currently under investigation.
Conclusions: This ongoing study has identified a novel human DP T cell that arises from the CD8+ T cell population and develops during GVHD. These cells are functionally active and display both modulatory and cytotoxic cytokine expression. Finally the development of DP is predictive of GVHD in a xenogeneic transplant model and is currently being validated in primary human HSCT samples.
Side-Chain Polarity of Amino Acids Within the Kir7.1 Channel Pore Lining Determine Permeability and Function
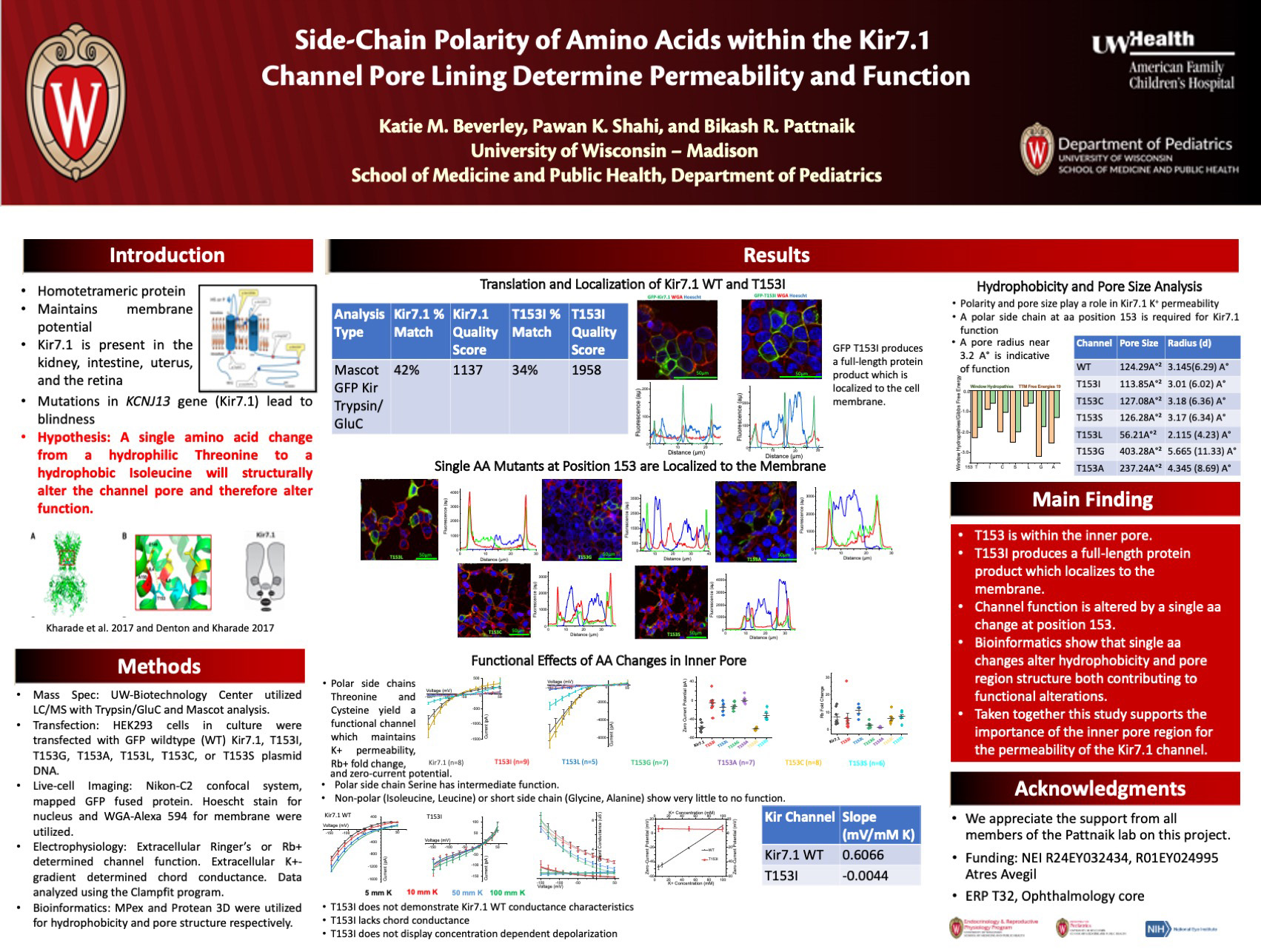
Click her for .pdf version of poster
Title: Side-Chain Polarity of Amino Acids Within the Kir7.1 Channel Pore Lining Determine Permeability and Function
Beverley K, Shahi P, Pattnaik B
Background: Inwardly rectifying potassium (K+) channels (Kir) maintain membrane potential and K+ homeostasis across many tissues. Mutations in the KCNJ13 gene encoding for Kir7.1 protein, in the retinal pigmented epithelium (RPE), cause pediatric blindness. One point mutation in the KCNJ13 gene c.458C>T Threonine (T) to Isoleucine (I) at amino acid position 153 lines the inner pore of the tetrameric protein. We sought to elucidate the impact of pore region amino-acid hydrophobicity and side-chain length on the channel function.
Design/Methods: Amino acid side-chain polarity and length at position T153 are important determinants of Kir7.1 channel structure/function. HEK293 cells in culture were transfected with GFP tagged wildtype (WT) Kir7.1, T153I, T153G, T153A, T153L, T153C, or T153S plasmid DNA. Live-cell imaging, using the Nikon-C2 confocal system, mapped the expression of GFP fused protein. Hoescht and WGA-Alexa 594 labeled the nucleus and plasma membrane, respectively. Off-line image analysis was performed with Nikon NIS Elements. Whole-cell patch-clamp electrophysiology with either extracellular Ringer’s or Rb+ determined channel function. Extracellular K+-gradient was used to determine chord conductance.
Results: Live-cell imaging indicated that Kir7.1 WT and all mutants studied are trafficked to the membrane. The IV plot for the Kir7.1 WT showed inward current measured at -150 mV with a mean amplitude of -863.67 ± 142.44 pA (n = 8) compared to Ile -68.54 ± 10.49 pA (n = 9, P = 2.79×10-5). Extracellular K+ dependent chord conductance further confirmed that T153I is nonfunctional. The current amplitude rank order for the mutant channel K+ permeability was Cys > WT > Ser > Gly > Ile > Ala> Leu. The membrane potential, measured as zero-current potential, was -57.75 ± 3.23 mV (n = 8) for the WT compared to -5.46 ± 6.01 mV (n = 9, P = 2.27×10-6) for the disease mutant with a rank order of Cys > WT > Ser > Leu > Gly > Ile > Ala. Rb+ ion, selectively permeates through Kir7.1 channel with a Rb+-current fold-change of 7.28 ± 1.63 (n = 8) for WT versus 6.48 ± 2.78 (n = 9, P=0.81) for the disease mutant. The rank order of Rb+-current fold-change was Leu > Ser > WT > Ile > Cys > Gly > Ala.
Conclusions: Even though all the mutant channels traffick normally to the membrane, T153I was non-functional as determined by K+ ion permeability. Upon testing, Rb+, it was deemed that T153I is actually dysfunctional. Based on the rank order, a substitution of polar amino acid at position 153 is required for Kir7.1 channel function. Permeability of all the mutant channels except T153A to Rb+ indicates that channel function is dependent on size of the cation. Since aa position T153 is within the inner pore-lining of the channel, a hydrophobic aa might alter protein-lipid interaction to affect channel function. Additionally, short-chain amino acids may further alter protein-protein interactions within the channel.
Human Monocytes Educated with Exosomes from TLR4 Primed Mesenchymal Stem Cells Treat Acute Radiation Syndrome by Promoting Hematopoietic Recovery
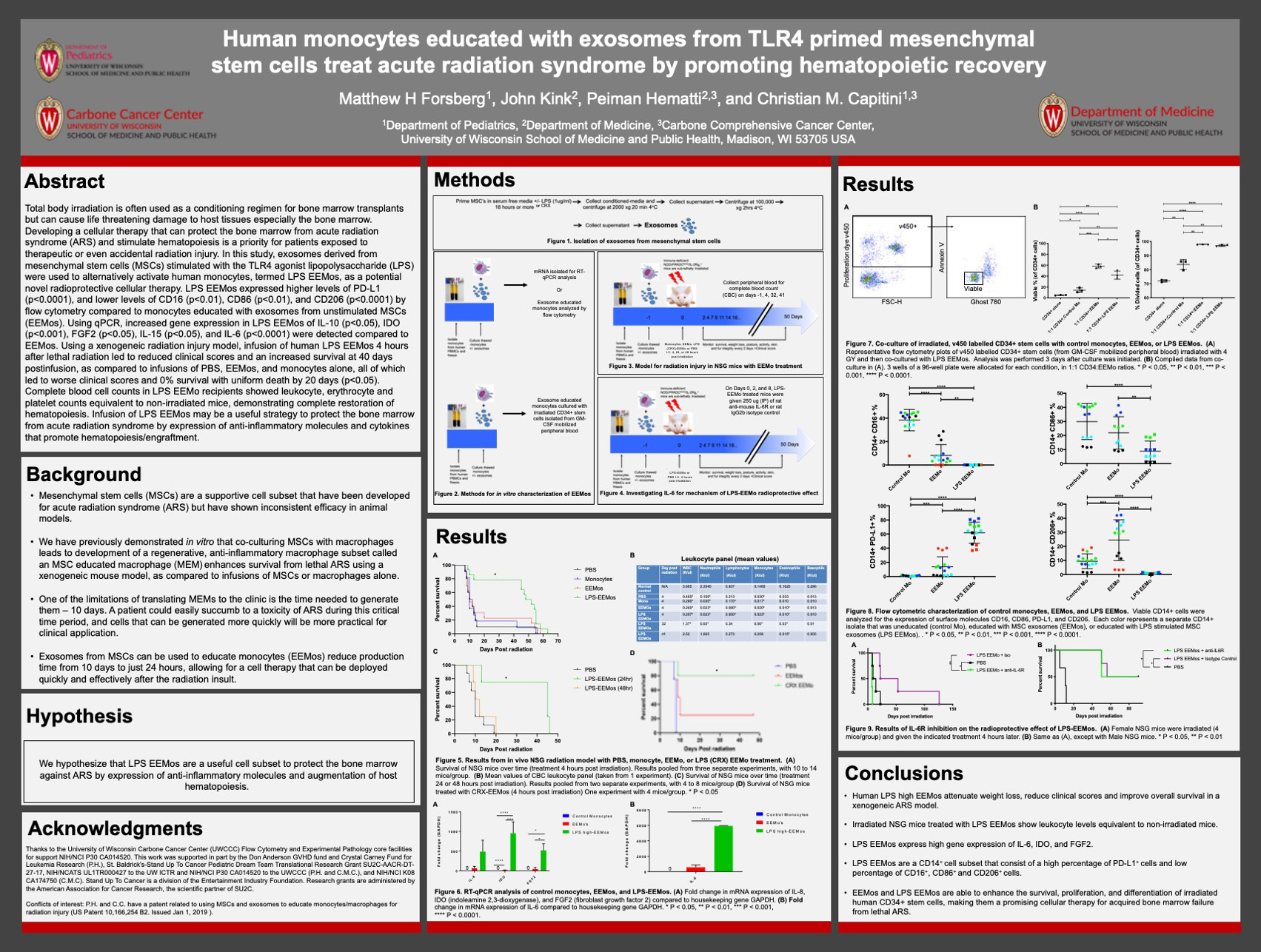
Click here for .pdf version of poster
Title: Human Monocytes Educated with Exosomes from TLR4 Primed Mesenchymal Stem Cells Treat Acute Radiation Syndrome by Promoting Hematopoietic Recovery
Forsberg M, Kink J, Hematti P, Capitini C
Background: Developing a cellular therapy that can protect the bone marrow from acute radiation syndrome and stimulate hematopoiesis is a priority for patients exposed to therapeutic or even accidental radiation injury. In this study, exosomes derived from MSCs stimulated with the TLR4 agonist lipopolysaccharide (LPS), or the less toxic LPS alternative CRX, were used to alternatively activate human monocytes, termed LPS EEMos, as a potential novel radioprotective cellular therapy.
Design/Methods: Exosomes were isolated from MSCs that were either unstimulated or stimulated with 1ug LPS (or CRX) for 18 hours. These exosomes were then cocultured overnight with monocytes. These educated monocytes were then characterized via qPCR and flow cytometry. Alternatively, these educated monocytes were given to NSG mice 4, 24, or 48 hours after being given a dose of 4 GY radiation to generate a xenogenic mouse model of ARS. Mice were then tracked for survival, with complete blood counts being taken periodically. To investigate the role of IL-6 in the radioprotective effect of LPS-EEMos, IL-6 receptor blocking monoclonal antibodies were given to mice on days 0, 2, and 8 post irradiations. LPS EEMos and EEMos were also cocultured with irradiated human CD34+ HSCs isolated from GMCSF mobilized peripheral blood. Survival and proliferation of the CD34+ cells was assessed after 3 days of culture by flow cytometry.
Results: Infusion of human LPS EEMos in to NSG mice 4 hours after lethal radiation led to an increased survival at 40 days post-infusion, as compared to infusions of PBS, EEMos, and monocytes alone, all of which led 0% survival with uniform death by 20 days (p<0.05). Complete blood cell counts in LPS EEMo recipients showed leukocyte, erythrocyte and platelet counts similar to non-irradiated mice. In vitro co-culture experiments showed that LPS EEMos were also able to improve the survival of Irradiated human CD34+ haemopoietic stem cells. Results from experiments using CRX instead of LPS showed that the CRX-EEMos provided mice with the same radioprotective effect as LPS-EEMos. Increased IL-6 production from LPS-EEMos may have a radioprotective effect.
Conclusions: Infusion of LPS or CRX EEMos may be a useful strategy to protect the bone marrow from acute radiation syndrome by expression of anti-inflammatory molecules and cytokines that promote hematopoiesis/engraftment.
Structural Brain Imaging in Infant Macaques Exposed to Zika Virus Prenatally
Click here for .pdf version of poster
Title: Structural Brain Imaging in Infant Macaques Exposed to Zika Virus Prenatally
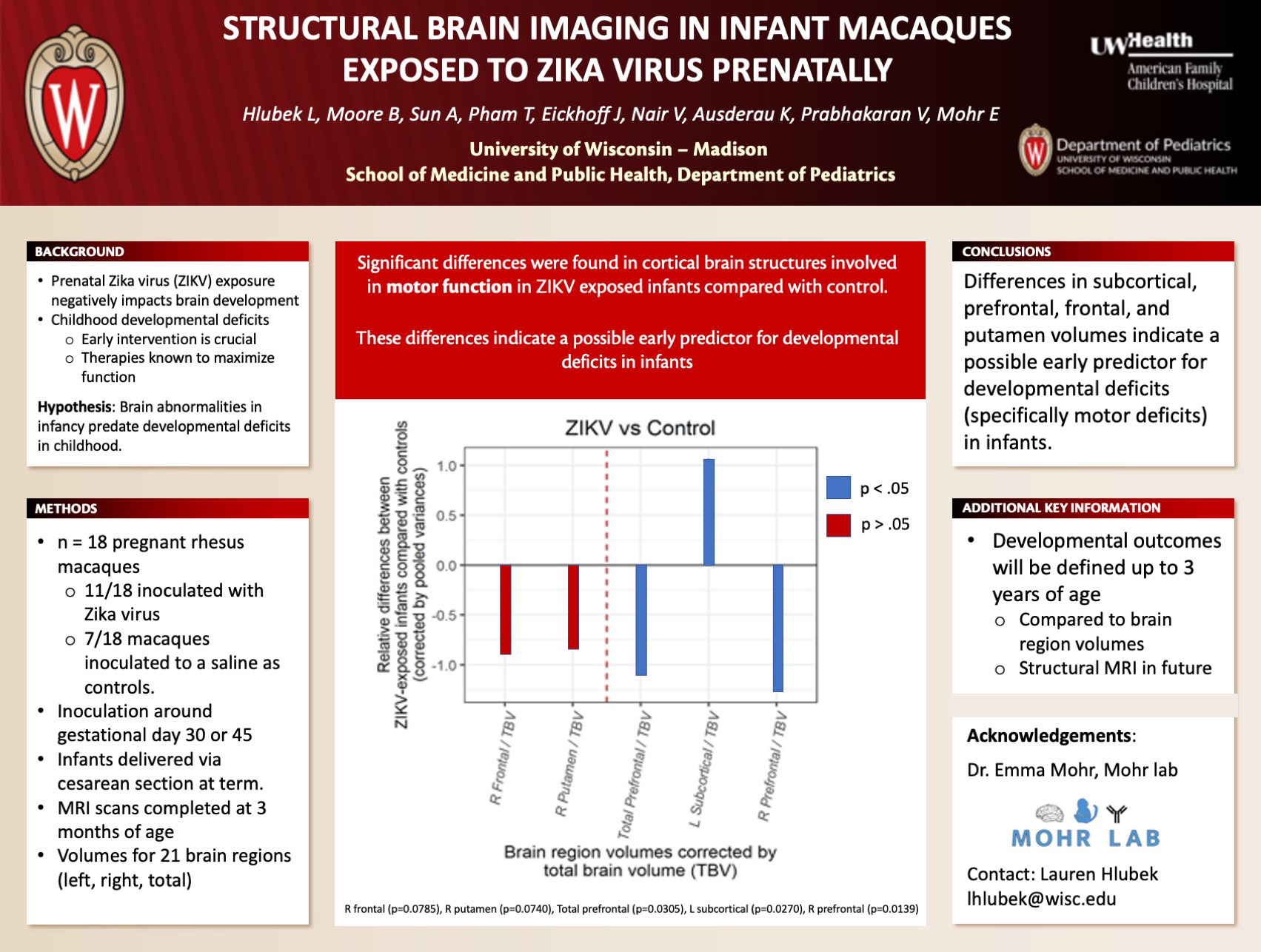
Hlubek L, Moore B, Sun A, Pham T, Eickhoff J, Nair V, Ausderau K, Prabhakaran V, Mohr E
Background: Prenatal Zika virus (ZIKV) exposure negatively impacts brain development in the fetus leading to developmental outcomes ranging from normal development to developmental deficits and birth defects. We do not currently know why some children develop normally and others develop deficits in early childhood. Because early intervention with therapies is the only effective therapy, early identification of children at high risk of developmental deficits is crucial. We hypothesize that brain abnormalities in infancy predate developmental deficits in childhood. We performed the first steps towards this goal by defining volumetric brain changes in ZIKV-exposed infant macaques in this study.
Design/Methods: 18 pregnant rhesus macaques were inoculated with a 1 x 10^4 PFU strain of Zika virus isolated from Puerto Rico (PRVABC59) . 7/18 macaques were inoculated to a saline at the same gestational ages as controls. Infants were delivered via cesarean section at term. Structural magnetic resonance imaging (MRI) scans were completed at 3 months of age. Volumes were measured for 21 brain regions.
Results: There were no significant differences in total brain volume, grey matter, white matter or ventricles between ZIKV-exposed infants and controls. We identified differences in cortical brain structures involved in motor function, including a bigger/smaller putamen (p=0.0740), bigger/smaller subcortical region (p=0.0270), bigger/smaller prefrontal lobe (p=0.0305), and frontal lobe (p=0.0785) in ZIKV-exposed infants compared with controls.
Conclusions: These differences in regions of the brain involved in motor function in ZIKV-exposed and control infant macaques indicate a possible early predictor for developmental deficits (specifically motor deficits) in infants. The developmental outcomes of these infants will be defined up to 3 years of age, and compared with these brain volumes to determine how early brain region volumes may predict later developmental outcomes.
An immune co-stimulatory vaccine, with adoptive transfer of natural killer cells and immune checkpoint blockade, after allogeneic bone marrow transplant, delays and reduces neuroblastoma tumor growth
Click here for .pdf version of poster
Title: An immune co-stimulatory vaccine, with adoptive transfer of natural killer cells and immune checkpoint blockade, after allogeneic bone marrow transplant, delays and reduces neuroblastoma tumor growth
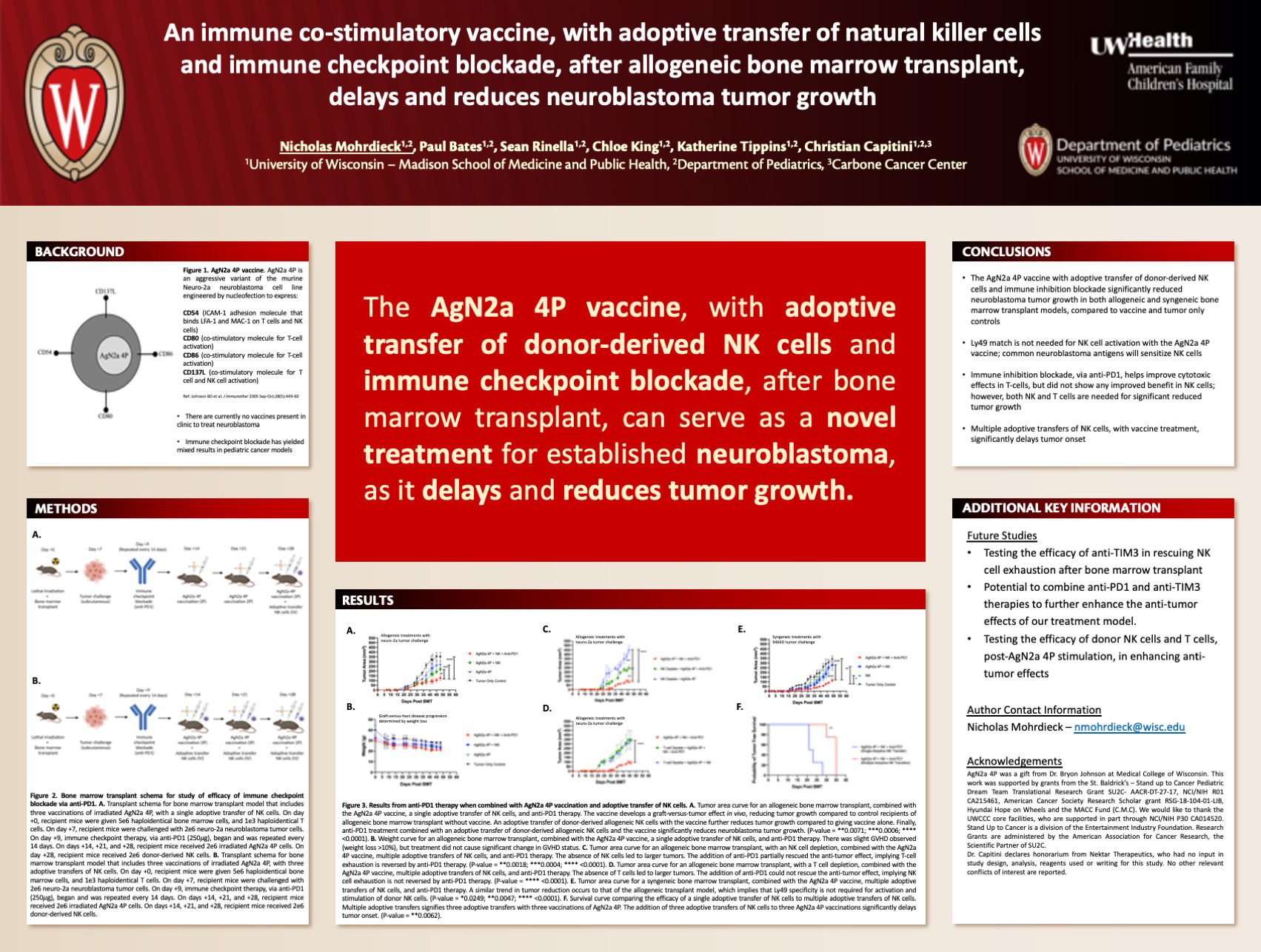
Mohrdieck NR, Bates PD, Rinella SP, King CA, Capitini CM
Background: High risk neuroblastoma remains a challenge to cure despite multi-modality treatment, with only 50% survival. “Tumor specific” therapies are needed to improve survival. Natural killer (NK) cells have cytotoxic effects against tumor cells and can also stimulate a T-cell mediated response against tumors. The immune co-stimulatory vaccine, AgN2a 4P, is an irradiated aggressive variant of the murine neuroblastoma cell line Neuro-2a, that is engineered to express four co-stimulatory markers – CD54, CD80, CD86, and CD137L1 – which can activate both NK and T-cells. In vitro, T-cells and NK cells stimulated by AgN2a 4P have greater cytotoxic effects against neuroblastoma, than T-cells and NK cells alone2. In vivo, giving AgN2a 4P after allogeneic bone marrow transplant (BMT), with adoptive transfer of donor-derived NK cells, induces a stronger anti-tumor response than giving AgN2a 4P alone2. However, this model was not curative. A limitation in activating both NK and T-cells is that they can become exhausted, abrogating their function. Inhibition of immune checkpoints that regulate exhaustion may keep NK and T-cells activated.
Design/Methods: Following an allogeneic BMT, B6AJ mice were challenged with neuro-2a murine neuroblastoma on day +7. Immune inhibition blockade, via anti-PD1, started on day +9 and was repeated every 14 days. Starting on day +14, vaccination of irradiated AgN2a 4P was given with or without adoptive transfer of donor-derived NK cells and was repeated every 7 days until endpoint was reached. Tumor growth and cytokine production were measured for efficacy of treatment.
Results: Combining immune inhibition blockade, via anti-PD1, with our combination therapy significantly delayed tumor onset and significantly reduced tumor growth compared to tumor only controls and the combination therapy absent of anti-PD1. Performing separate NK and T-cell depletions in our model signified that T-cells have a more robust response to anti-PD1 therapy than NK cells; however, both are needed for significant tumor reduction.
Conclusions: The AgN2a 4P vaccine, with adoptive transfer of NK cells and immune inhibition blockade, after allogeneic bone marrow transplant, serves as a novel approach to reducing neuroblastoma tumor growth, as previous studies have not been successful at curing pediatric malignancies with anti-PD1 or the use of allogeneic BMT.
CRISPR Base Editing as a Potential Therapeutic Approach for Kir7.1 Channelopathy
Click here for .pdf version of poster
Title: CRISPR Base Editing as a Potential Therapeutic Approach for Kir7.1 Channelopathy
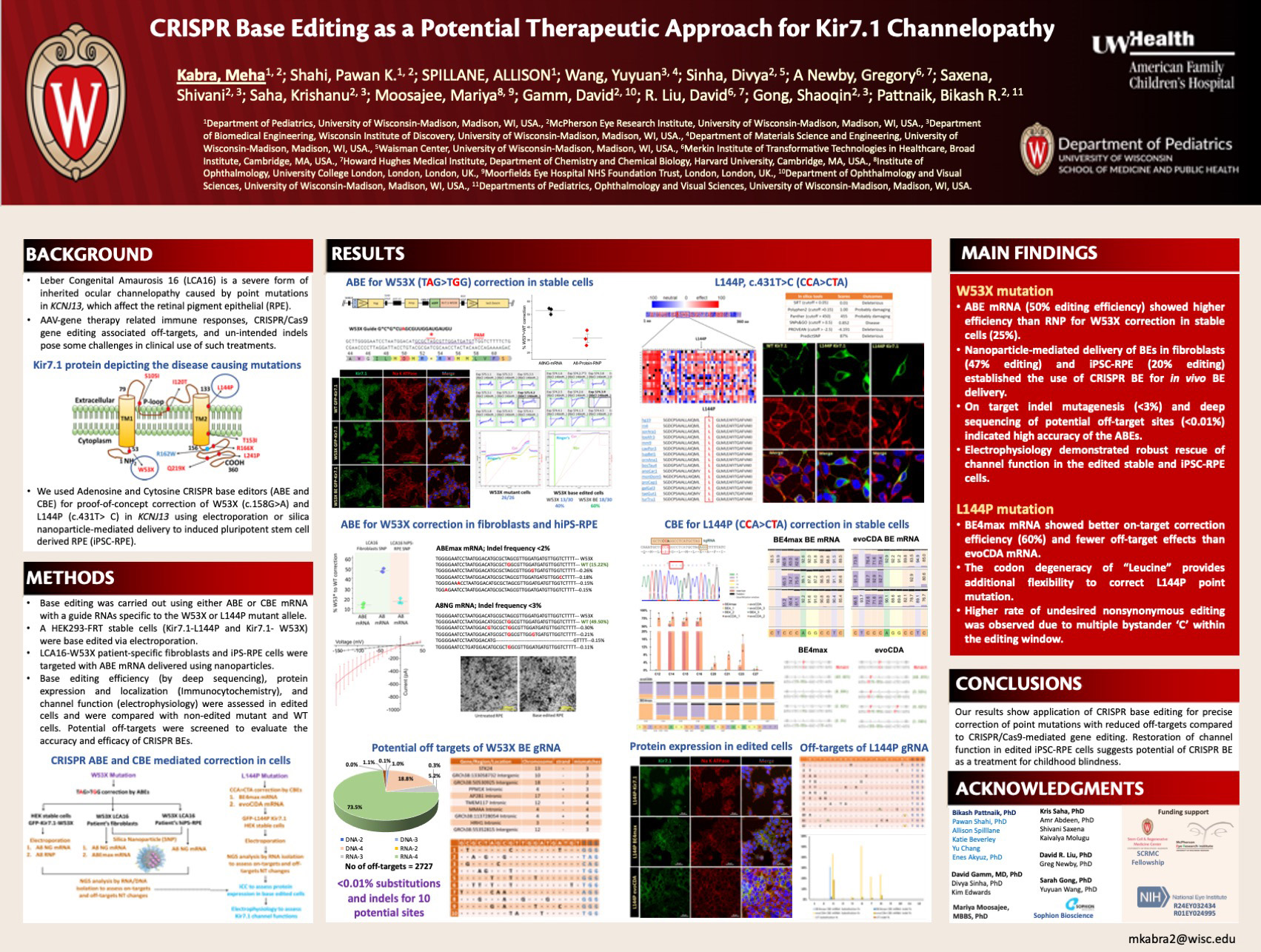
Kabra M, Shahi P, Spillane A, Wang Y, Sinha D, Newby G, Saxena S, Saha K, Moosajee M, Gamm D, Liu D, Gong S, Pattnaik B
Background: Leber Congenital Amaurosis 16 (LCA16) is a severe form of inherited ocular channelopathy caused by point mutations in KCNJ13, which affect the retinal pigment epithelial (RPE). AAV-gene therapy related immune responses, CRISPR/Cas9 gene editing associated off-targets, and unintended indels pose some challenges in clinical use of such treatments. We used Adenosine and Cytosine CRISPR base editors (ABE and CBE) for proof-of-concept correction of KCNJ13 point mutations (c.158G>A [p.W53X] and c.431T> C [p.L144P]) using nanoparticle-mediated delivery to induced pluripotent stem cell-derived RPE (iPSC-RPE).
Design/Methods: Base editing was carried out using either ABE or CBE mRNA with a guide RNAs specific to the W53X or L144P mutant allele. A HEK293-FRT stable cell line expressing Kir7.1-L144P and Kir7.1- W53X were base edited via electroporation using CBE and ABE mRNA respectively. LCA16-W53X patient-specific fibroblasts and iPS-RPE cells were also targeted with ABE mRNA delivered using nanoparticles. Base editing efficiency, protein expression, localization, and channel function were assessed in edited cells and were compared with non-edited mutant and WT cells. Potential off-targets were screened to evaluate the accuracy and efficacy of CRISPR BEs.
Results: CBE mRNA for L144P correction in HEK cells resulted in 66% editing. The degenerate nature of codons for provides additional flexibility to correct L144P point mutation. Higher rate (~24%) of off-targets were observed in treated L144P-cells due to multiple bystander cytosines at the targeted locus. ABE mRNA for W53X (TaG>TgG) correction in HEK stable cells showed 50% editing efficiency than RNP approaches (25% efficiency). Nanoparticle-mediated delivery of ABE-mRNA and sgRNA in fibroblasts (47% editing) and iPSC-RPE (20% editing) established its use for in vivo BE delivery. Control fibroblast cells lacking the mutant allele showed about 1% indels. On target indel mutagenesis (<3%) and deep sequencing of potential off-target sites (<1%) indicated high accuracy of the ABEs. Electrophysiology assays demonstrated robust rescue of channel function in the edited iPSC-RPE cells.
Conclusions: Our results show application of CRISPR base editing for precise correction of point mutations with reduced off-targets compared to CRISPR/Cas9-mediated gene editing. Restoration of channel function in edited iPSC-RPE cells suggests potential of CRISPR BE as a treatment for childhood blindness.
Session C: Care Innovation
| Time | Presenter | Title |
|---|---|---|
| 3:30-3:36 | Joseph McBride, MD | The utility of “lollipop” oral swabs in the diagnosis of COVID-19 |
| 3:36-3:42 | Ellen Sutter | Disrupted access to therapies and impact on well-being during the COVID-19 pandemic for children with motor impairment and their caregivers |
| 3:42-3:48 | Preet Matharu, MD | Modifying 17-hydroxyprogesterone screening cutoffs for improved detection of 21-hydroxylase deficiency |
| 3:48-3:54 | Lindsey McGowan, MD | Umbilical Cord Blood Cultures in Chorioamnionitis |
| 3:54-4:00 | Susan Xia | Contact-free neonatal heart rate and respiratory rate monitor |
| 4:06-4:12 | Narmin Mukhtarova | Serum Ferritin Threshold to Diagnose Iron Deficiency in Children 9 to 13 Months Age |
| 4:12-4:18 | Lauren Gadek | Correlation of renal tissue oxygenation to venous, arterial, and capillary blood gas oxygen saturation in preterm neonates |
| 4:18-4:24 | Santhi Logel, MD | Continuous Glucose Monitoring Facilitates Diazoxide Use in the Management of Glut1 Deficiency Syndrome |
| 4:24-4:30 | Emma Simpson | Feasibility of remote transcranial direct current stimulation for pediatric cerebral palsy during the COVID-19 pandemic |
| 4:36-4:42 | Diane Brown, MD | Improvements in post-operative cardiac surgery arrhythmia identification using the Atriamp signals |
| 4:42-4:48 | Megan Peters, MD | Performing Minor Urologic Procedures in a Pediatric Sedation Center May Be Safe and Cost-Effective: A Pilot Study |
| 4:48-4:54 | Jonathan Mietchen, MD | Utility of Neuropsychological Screening in a Multidisciplinary Neurocutaneous Clinic |
| 4:54-5:00 | Colin Korlesky | Portable Electroretinography (ERG) Goggles for use in The Pediatric Surgical Suite |
| 5:000 | Wrap-Up |
This is an accordion element with a series of buttons that open and close related content panels.
The Utility of “Lollipop” Oral Swabs in the Diagnosis of COVID-19
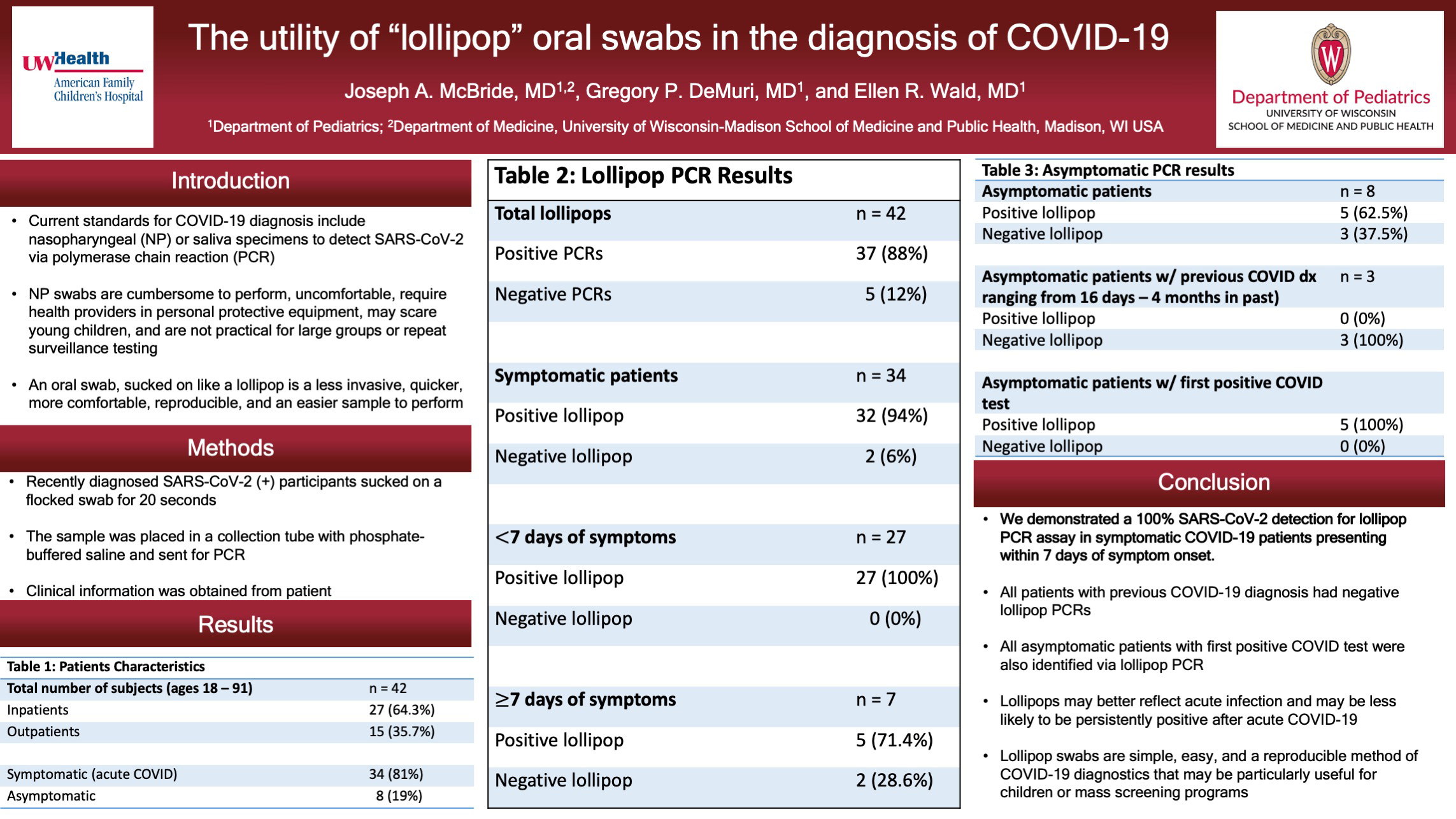
Click here for .pdf version of poster
Title: The Utility of “Lollipop” Oral Swabs in the Diagnosis of COVID-19
McBride J, DeMuri G, Wald, E
Background: Rapid and accurate diagnosis is essential for control of the COVID-19 pandemic. Current standards for diagnosis include nasopharyngeal (NP) or saliva specimens to detect SARS-CoV-2 via polymerase chain reaction (PCR). Alternatively, nasal swabs via lateral flow immunoassay for rapid qualitative antigen detection are available. NP swabs are cumbersome to perform, uncomfortable for the patient, demand assistance from health care providers, require personal protective equipment due to aerosolization of the virus, and are not practical for large groups that may require repeat testing for surveillance. NPs are especially challenging in young children secondary to fear and invasiveness of testing. Saliva specimens are an alternative diagnostic test with comparable results to NP specimens. An oral swab, sucked on like a lollipop is a less invasive, quicker more comfortable, more reproducible, and easier sample to perform. The lollipop swab may be obtained by the individual, parent, or non-medical guardian without the need for a medical provider or PPE.
Design/Methods: Adult inpatients and outpatients with positive SARS-CoV-2 PCRs were enrolled in the study. Participants were approached within 24 hours from their diagnostic NP or saliva PCR. Participants sucked on a flocked swab for 20 seconds. The sample was placed in a collection tube with phosphate-buffered saline and sent for PCR. Information on participants’ age, gender, race, time between diagnostic and lollipop testing, day of illness, degree of respiratory support, presence/absence of dry mouth, and symptoms were obtained.
Results: 40 patients aged 18 through 91 participated. 32 patients were symptomatic (80%) and 8 patients were asymptomatic (20%). Of the 40 lollipop PCRs obtained 35 (87.5%) detected SARS-CoV-2. Of the 32 symptomatic patients 30 (93.75%) were positive. Symptomatic patients presenting within 7 days of symptom onset were positive in 25 out of 25 cases (100%). Asymptomatic patients were divided into 2 groups – 1) those with a previous diagnosis of COVID-19 (n=3) and 2) those diagnosed with COVID for the first time (n = 5). None of the lollipop PCRs in asymptomatic patients with a previous COVID diagnosis were positive (0/3). All asymptomatic patients w/ first positive COVID test had positive lollipops as well (5/5).
Conclusions: We demonstrated a 100% SARS-CoV-2 detection for lollipop PCR assay in symptomatic COVID-19 patients presenting within 7 days of symptom onset. All patients with previous COVID-19 diagnosis had negative lollipop PCRs. All asymptomatic patients with first positive COVID test were also identified via lollipop PCR. Lollipops may better reflect acute infection and may be less likely to be persistently positive than NP swabs after acute COVID-19. Lollipop swabs are simple, easy, and a reproducible method of COVDI-19 diagnostics that may be particularly useful for children or mass screening programs.
Disrupted Access to Therapies and Impact on Well-Being During the COVID-19 Pandemic for Children with Motor Impairment and Their Caregivers
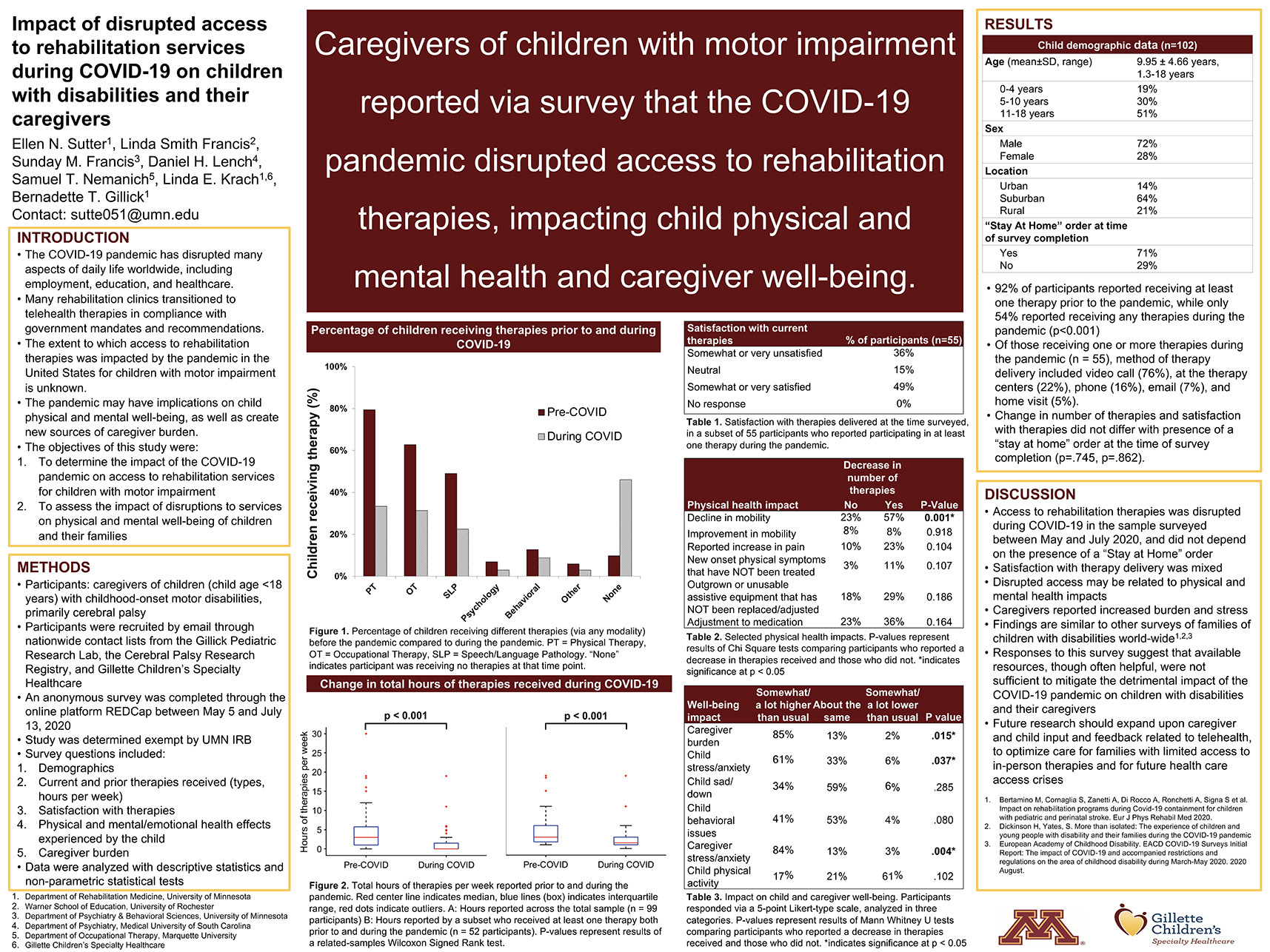
Click here for .pdf version of poster
Title: Disrupted Access to Therapies and Impact on Well-Being During the COVID-19 Pandemic for Children with Motor Impairment and Their Caregivers
Sutter E, Francis L, Francis S, Lench D, Nemanich S, Krach L, Gillick B
Background: This study aimed to determine the impact of the COVID-19 pandemic on access to rehabilitation services, as well as the impact of disrupted access to services on the mental and physical well-being of children with motor impairment and their families.
Design/Methods: Caregivers of children (child age <18 years) with childhood-onset motor impairment, primarily cerebral palsy, were included. Participants were recruited by email from established nationwide contact lists through the Gillick Pediatric Research Lab, the Cerebral Palsy Research Registry, and Gillette Children’s Specialty Healthcare. Participants completed an anonymous survey through the online platform REDCap between May 5, 2020 and July 13, 2020 during the COVID-19 pandemic. Questions included demographics, current and prior therapies received, physical and mental health effects experienced by the child, and caregiver burden. Data were analyzed with descriptive statistics and non-parametric statistical tests.
Results: The survey was completed by 102 caregiver participants. Prior to the pandemic, 92 of 102 children (90%) received one or more therapies; at the time surveyed, 55 children (54%) received any therapies (p<.001). Among those who received any therapies at the time surveyed, video consultations were the most common form of therapy delivery (76%), and the median total hours of therapies decreased from 3 hours to 1.5 hours per week (p<.001). Reported child health impacts during the pandemic in >40% of the sample included increased stress, decreased physical activity, and decline in mobility/movement. Participants who reported a decrease in number of therapies at the time surveyed more frequently reported lower satisfaction with treatment delivery (p<.001), decline in child’s mobility (p =.001), and increased caregiver stress (p=.004). Change in number of therapies and satisfaction with therapies did not differ with presence of a “stay at home” order at the time of survey completion (p=.745, p=.862).
Conclusions: Access to pediatric rehabilitation therapies was disrupted during COVID-19 in the sample surveyed, and disrupted access may be related to physical and mental health impacts. With the expansion of telehealth, caregiver and child feedback should be incorporated to optimize benefit.
Modifying 17-Hydroxyprogesterone Screening Cutoffs for Improved Detection of 21-Hydroxylase Deficiency
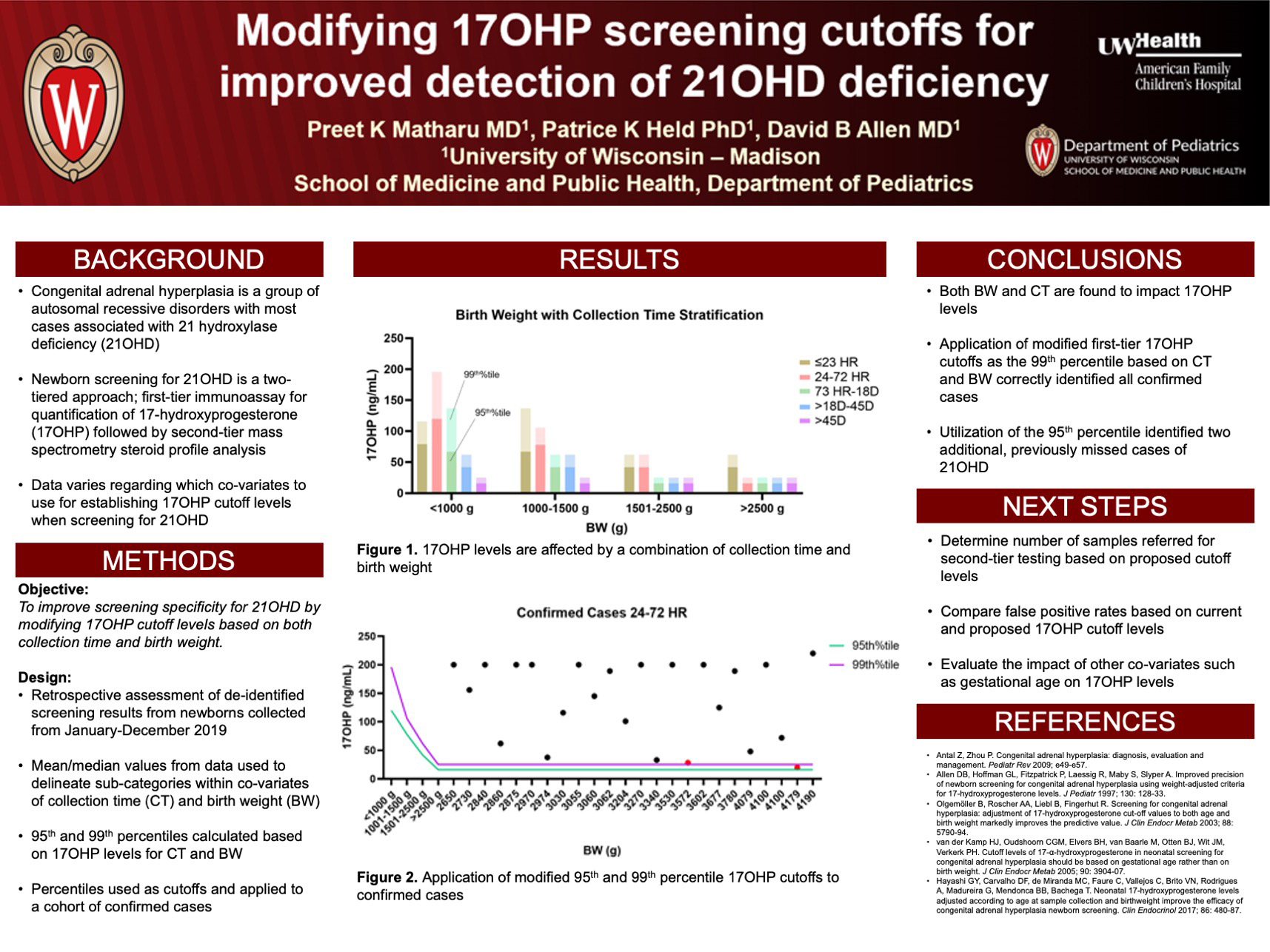
Click here for .pdf version of poster
Title: Modifying 17-Hydroxyprogesterone Screening Cutoffs for Improved Detection of 21-Hydroxylase Deficiency
Matharu P, Held P, Allen D
Background: Congenital adrenal hyperplasia (CAH) is a group of autosomal recessive disorders defined by impaired cortisol synthesis. The most common form, 21-hydroxylase deficiency (21OHD), is identified by elevated 17-hydroxyprogesterone (17OHP) levels on newborn screens. While current testing using an immunoassay can detect cases of 21OHD, this screening process has a high false positive rate. There is also a lack of consensus regarding which covariates to use such as gestational age (GA), birth weight (BW), or collection time (CT) when determining 17OHP screening cutoffs to improve specificity. There is also potential for false negative cases due to late rising 17OHP concentrations. Wisconsin has a two-tiered screening algorithm for 21OHD involving a first-tier immunoassay followed by a more sensitive second-tier steroid profile. The objective of our study is to improve screening specificity for 21OHD by modifying 17OHP cutoff levels based on both CT and BW to optimize the number of specimens undergoing second-tier testing and minimize the risk of false negative cases.
Design/Methods: This was a retrospective assessment of de-identified 17OHP screening results from the Wisconsin registry of presumed normal newborn screening specimens collected from January to December 2019. Data were grouped based on CT of the specimen and BW. Mean and median 17OHP levels were calculated from the screening data and used to delineate sub-categories of CT and BW. Within these subcategories, the 95th and 99th percentiles were calculated based on the 17OHP levels. These percentiles were then applied to a cohort of confirmed cases of 21OHD to assess screening accuracy of new proposed thresholds.
Results: Results of the study demonstrated that both CT and BW are factors impacting 17OHP concentrations. The newly proposed 95th and 99th percentile cutoffs were applied to 17OHP levels collected from 27 confirmed cases of 21OHD. In addition to correctly identifying 21OHD in 25 confirmed cases, this approach identified 2 additional cases that would have otherwise been missed with current screening strategies.
Conclusions: This study demonstrates that application of modified first-tier 17OHP cutoffs based on CT and BW accurately identified all confirmed cases of 21OHD. The proposed cutoffs also identified 2 cases of 21OHD that were previously missed. These 17OHP cutoffs will be implemented into routine newborn screening.
Umbilical Cord Blood Cultures in Chorioamnionitis
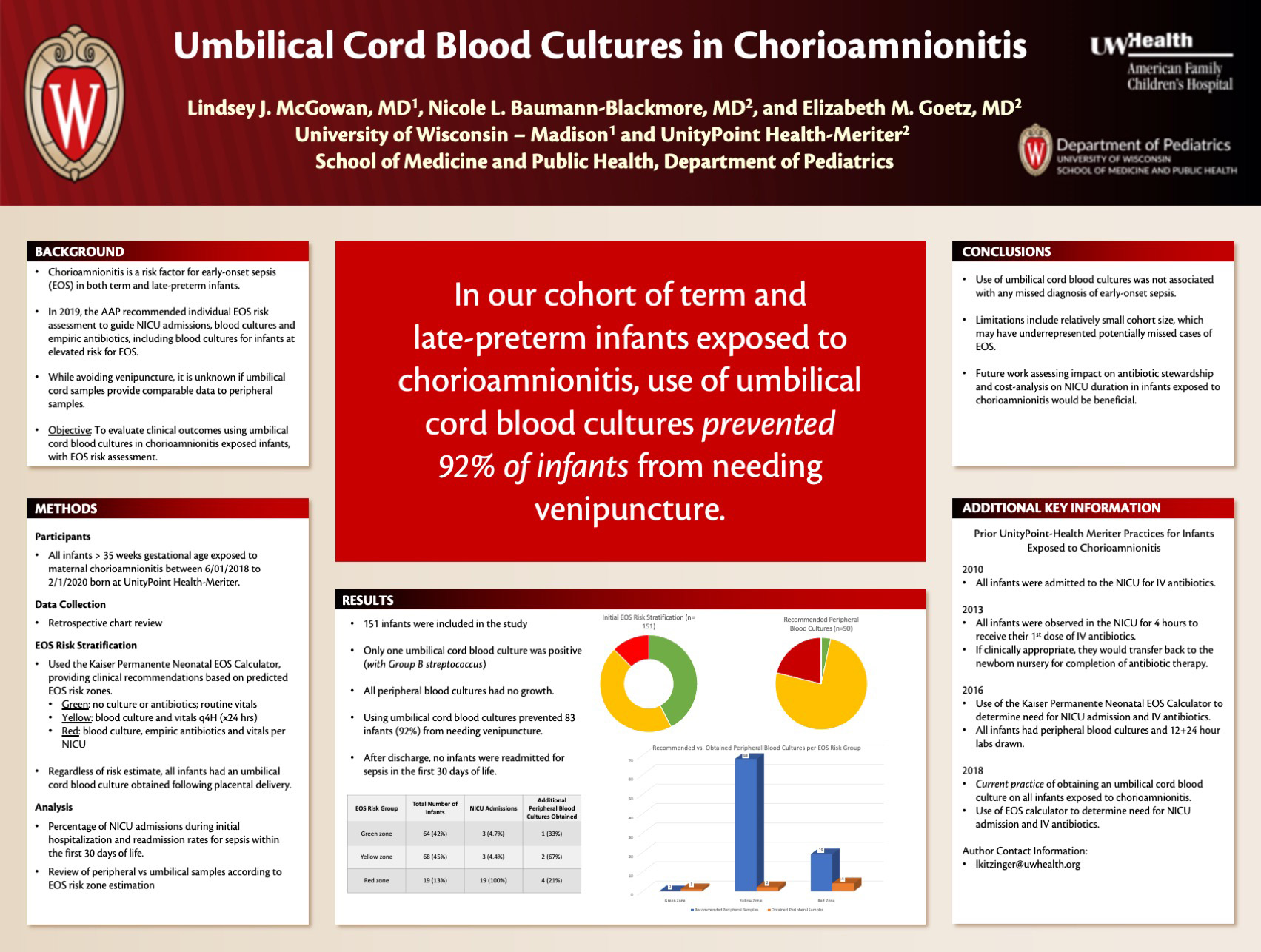
Click here for .pdf version of poster
Title: Umbilical Cord Blood Cultures in Chorioamnionitis
McGowan L, Goetz E, Baumann-Blackmore N
Background: Chorioamnionitis is a risk factor for early-onset sepsis (EOS) in term and late-preterm infants. In 2019, the AAP recommended individual EOS risk assessment to guide neonatal intensive care unit (NICU) admissions, blood cultures and empiric antibiotics, including blood cultures for infants at elevated risk for EOS. Obtaining cultures from the umbilical cord avoids venipuncture after birth, however, it is unknown if cord blood cultures provide comparable data to peripheral samples. This study evaluated clinical outcomes using umbilical cord blood cultures in chorioamnionitis exposed infants, with EOS risk assessment.
Design/Methods: A retrospective data review was performed from 2018-2019 at UnityPoint Health-Meriter. All chorioamnionitis exposed infants born > 35 weeks gestation were included and risk stratified using the Kaiser Permanente Neonatal EOS Calculator. This tool provided clinical recommendations based on predicted green, yellow or red EOS risk zones. An umbilical cord blood culture was drawn following placental delivery, despite risk estimate. Analysis included percentage of NICU admissions during initial hospitalization and readmission rates within the first 30 days of life.
Results: 151 infants were included with risk stratification placing 64 infants in the green zone, 68 in the yellow zone, and 19 in the red zone. The red zone was admitted to the NICU for empiric antibiotics; 4 of these infants also had peripheral blood cultures drawn, which were negative. 136 infants were admitted to the Newborn Nursery, with 6 of these infants being transferred to the NICU for sepsis rule-out, including a green-zone infant with the only positive cord blood culture. 3 of these infants also had peripheral blood cultures drawn, which had no growth. After discharge, no infants were readmitted for sepsis in the first 30 days of life. In this sample, 87 infants (58%) were stratified to an elevated risk (yellow or red) zone, where a blood culture is recommended, with 3 additional green zone infants requiring peripheral blood cultures per AAP guidelines. Rather, by drawing cord blood cultures, 91 (60%) of infants were prevented from needing venipuncture.
Conclusions: In our review, the use of cord blood cultures was not associated with any missed diagnoses of EOS. These findings suggest that using cord blood in chorioamnionitis provides a painless, yet effective way to obtain data. Future work assessing antibiotic use and cost-analysis of this method on NICU duration in chorioamnionitis would be beneficial.
Contact-Free Neonatal Heart Rate and Respiratory Rate Monitor
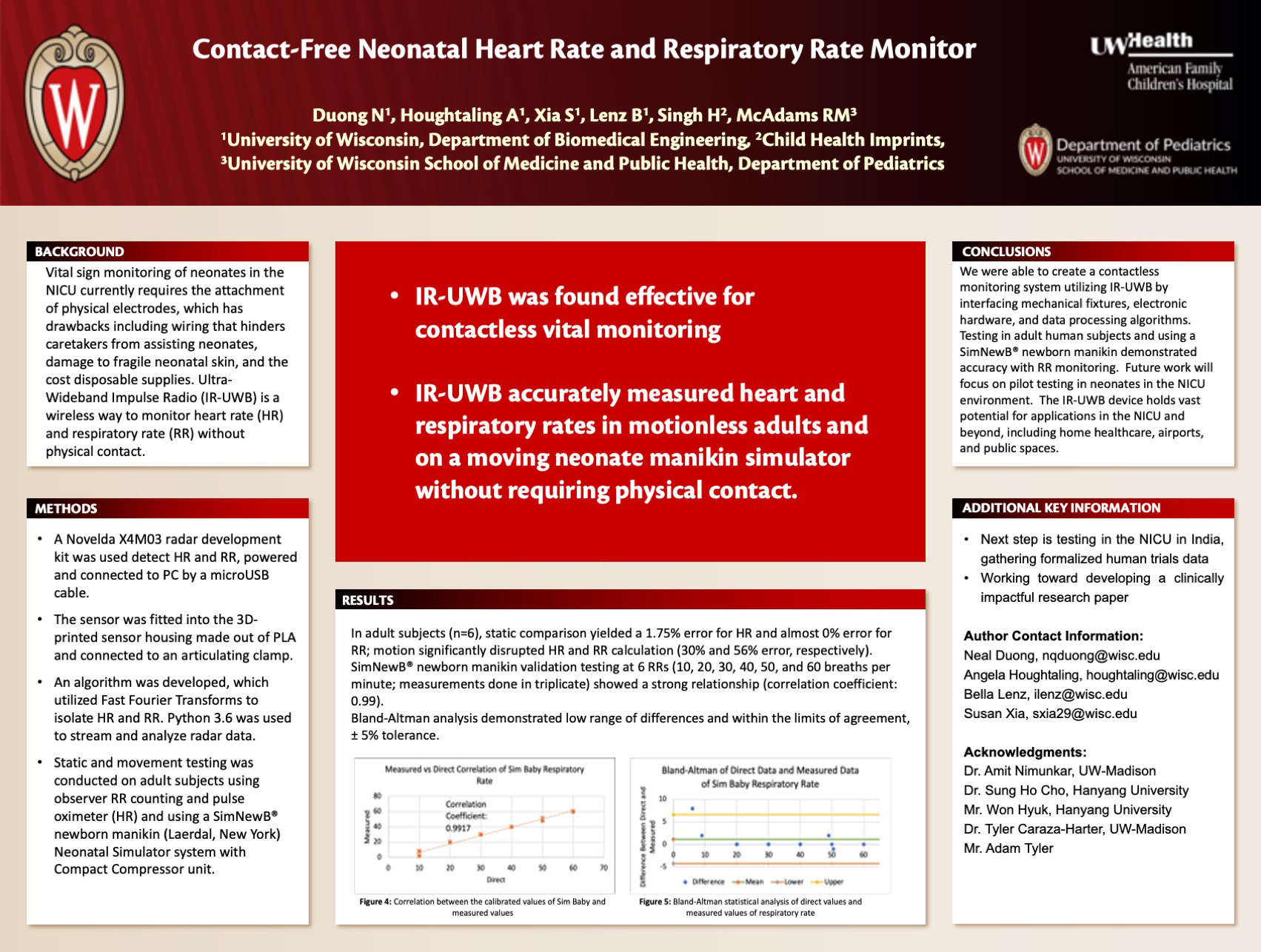
Click here for .pdf version of poster
Title: Contact-Free Neonatal Heart Rate and Respiratory Rate Monitor
Duong N, Houghtaling A, Xia S, Lenz B, Singh H, McAdams RM
Background: Vital sign monitoring of neonates in the NICU currently requires the attachment of physical electrodes, which has drawbacks including wiring that hinders caretakers from assisting neonates, damage to fragile neonatal skin, and the added cost due to disposable supplies. Ultra-Wideband Impulse Radio (IR-UWB) is a wireless way to potentially monitor heart rate (HR) and respiratory rate (RR) without physical contact.
Design/Methods: A Novelda X4M03 radar development kit was used detect HR and RR, powered and connected to PC by a microUSB cable. The sensor was fitted into the 3D-printed sensor housing made out of PLA and connected to an articulating clamp. An algorithm was developed, which utilized Fast Fourier Transforms to isolate HR and RR. Python 3.6 was used to stream and analyze radar data. Static and movement testing was conducted on adult subjects using observer RR counting and pulse oximeter (HR) and using a SimNewB® newborn manikin (Laerdal, New York) Neonatal Simulator system with Compact Compressor unit.
Results: In adult subjects (n=6), static comparison yielded a 1.75% error for HR and almost 0% error for RR; motion significantly disrupted HR and RR calculation (30% and 56% error, respectively). SimNewB® newborn manikin validation testing at 6 RRs (10, 20, 30, 40, 50, and 60 breaths per minute; measurements done in triplecate) showed a strong relationship (correlation coefficient: 0.99) Bland-Altman analysis demonstrated low range of differences and within the limits of agreement, ± 5% tolerance.
Conclusions: We were able to create a contactless monitoring system utilizing IR-UWB by interfacing mechanical fixtures, electronic hardware, and data processing algorithms. Testing in adult human subjects and using a SimNewB® newborn manikin demonstrated accuracy with RR monitoring. Future work will focus on pilot testing in neonates in the NICU environment. The IR-UWB device holds vast potential for applications in the NICU and beyond, including home healthcare, airports, and public spaces.
Serum Ferritin Threshold to Diagnose Iron Deficiency in Children 9 to 13 Months Age
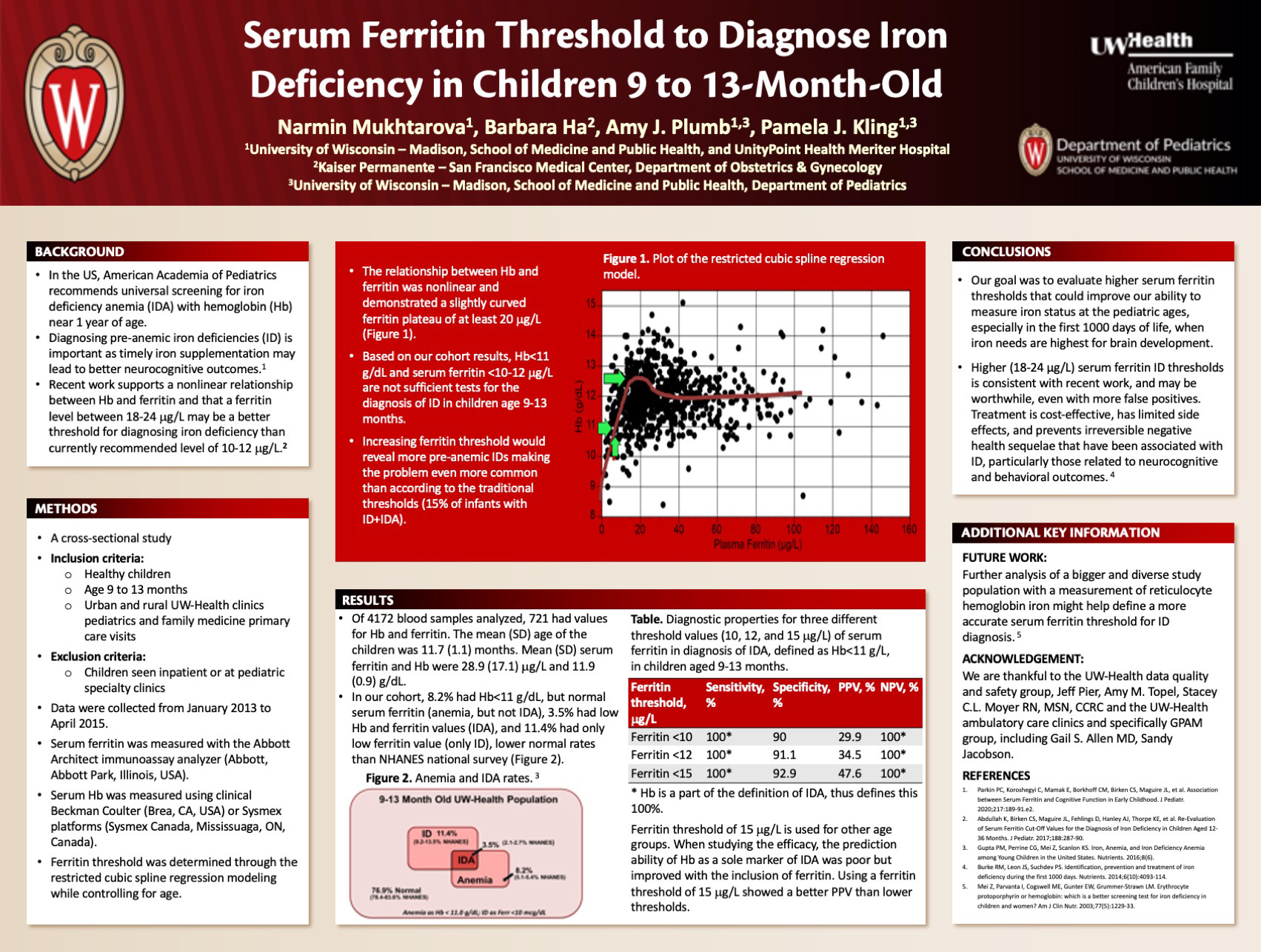
Click here for .pdf version of poster
Title: Serum Ferritin Threshold to Diagnose Iron Deficiency in Children 9 to 13 Months Age
Mukhtarova N, Ha B, Pumb A, Kling P
Background: The American Academy of Pediatrics (AAP) recommends universal screening with hemoglobin for iron deficiency (ID) and ID anemia (IDA) near one year of age to coincide with a well child visit. Hemoglobin (anemia screening) was recommended because of its universal availability and ease in using smaller volume capillary samples. Recent work supports the importance of diagnosing ID before anemia develops using iron indices, such as ferritin, as timely iron supplementation may lead to better neurocognitive outcomes. Recent work also supports a nonlinear relationship between hemoglobin and ferritin and that a ferritin between 18-24 mcg/L may be a better threshold than ferritin of 10 mcg/L. We sought to validate these findings in our own university-based ambulatory clinic in a population of 9 to 13-month-old children.
Design/Methods: For a quality initiative, a cross-sectional study of healthy children aged 9 to 13 months seen in both urban and rural UW-Health clinics was undertaken in primary care visits. Data were collected from January 2013 to April 2015. According the AAP, hemoglobin<110 g/L was considered as anemia and ferritin <10 mcg/L was considered as ID. We examined the relationship between hemoglobin and ferritin through the restricted cubic spline regression modeling to determine ferritin threshold.
Results: Of 4172 screens performed, 719 screens had a simultaneous hemoglobin and ferritin obtained. Of these, 8.2% had Hb below 11, but normal ferritin values (anemia, but not IDA), 3.5% had low hemoglobin and ferritin values (IDA), and 11.4% had only ferritin below the threshold (only ID). The relationships between Hb and ferritin was nonlinear, requiring cubic spline regression modeling with 4 and 5 knots, and supported a slightly curved ferritin plateau of at least 20 mcg/L.
Conclusions: Using traditional thresholds, nearly 15% of infants had either ID or IDA, making this a common problem in our practice. Our data support others in that the relationship between hemoglobin and ferritin is nonlinear and a ferritin value of at least 20 mcg/L may be a better threshold. If so, substantially more infants would be diagnosed with ID or IDA, making the problem even more common in our practice.
Correlation of Renal Tissue Oxygenation to Venous, Arterial, and Capillary Blood Gas Oxygen Saturation in Preterm Neonates
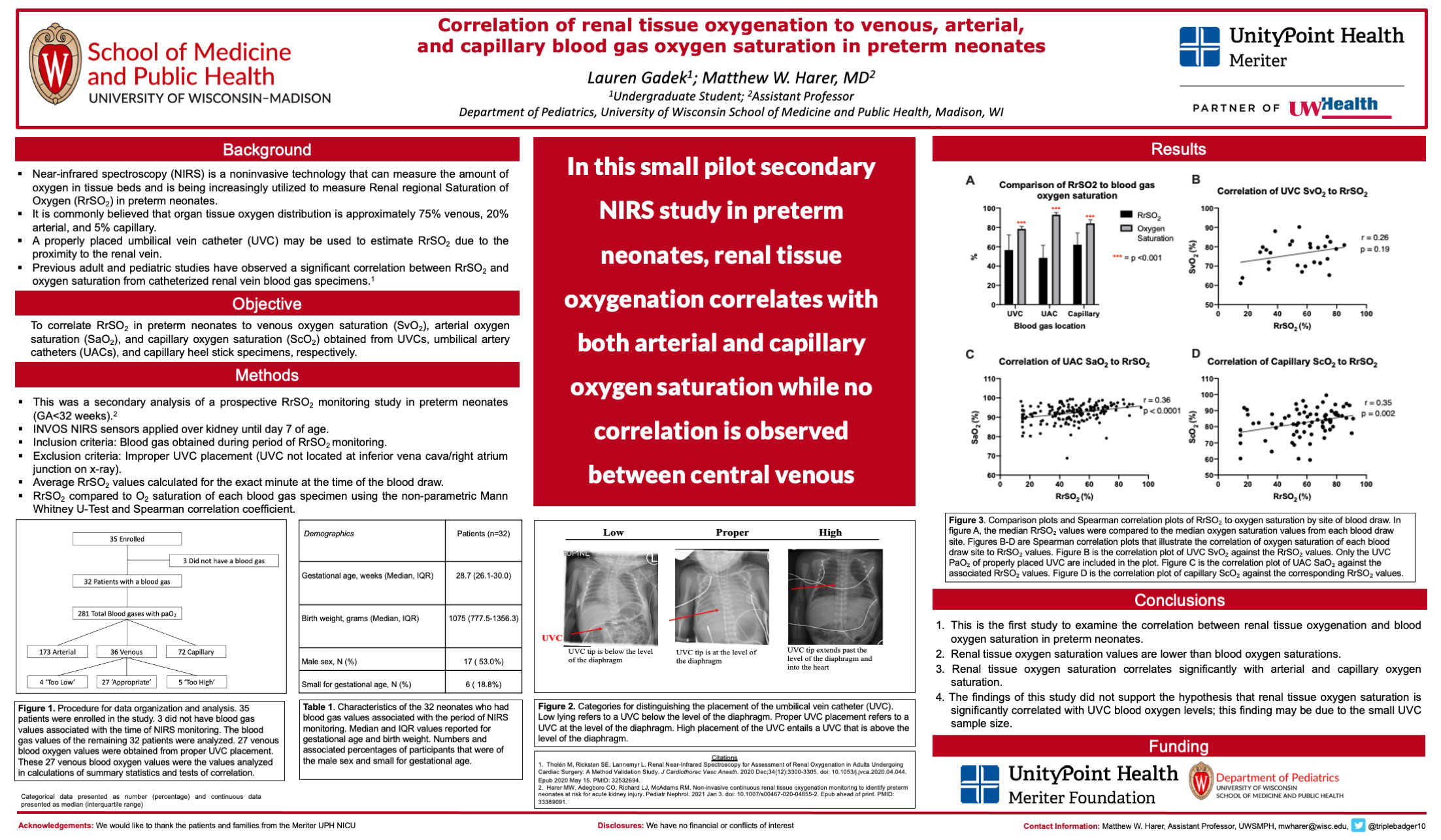
Click here for .pdf version of poster
Title: Correlation of Renal Tissue Oxygenation to Venous, Arterial, and Capillary Blood Gas Oxygen Saturation in Preterm Neonates
Gadek, L; Harer, M
Background: Near infrared spectroscopy (NIRS) measures tissue oxygenation and is being increasingly utilized in preterm neonates to monitor Renal regional Saturation of Oxygen (RrSO2). Theoretically, the contribution to tissue oxygenation is 75% venous, 20% arterial, and 5% capillary. Adult and pediatric studies have shown excellent correlation between RrSO2 and oxygen saturation from catheterized renal vein blood gas specimens. Although preterm neonates are too small to place a renal vein catheter, a properly placed umbilical vein catheter (UVC) may estimate RrSO2 given the proximity to the renal vein. Our objective was to correlate RrSO2 in preterm neonates to venous oxygen saturation (SvO2), arterial oxygen saturation (SaO2) and capillary oxygen saturation (ScO2) obtained from UVCs, umbilical arterial catheters (UACs) and heel stick specimens, respectively.
Design/Methods: This is a secondary analysis of a prospective RrSO2 monitoring study in preterm neonates (gestational age (GA) < 32 weeks). Neonates with any blood gas obtained during RrSO2 monitoring were included, except when the UVC was not located at the IVC/RA junction on x-ray. RrSO2 was compared to simultaneous O2 saturation on each blood gas specimen using the non-parametric Mann Whitney U-test and Spearman correlation coefficient.
Results: Data included 27 UVC specimens (4 patients, median GA 26.6 weeks), 172 UAC specimens (19 patients, median GA 28.1 weeks), and 73 heel stick capillary specimens (24 patients, median GA 28.7 weeks). RrSO2 was lower than the median SvO2 (56.6 vs. 78.4, p<0.0001), SaO2 (48.4 vs. 93, p<0.0001), and ScO2 (62.1 vs. 78.4, p<0.001) (Figure A). RrSO2 values were significantly correlated to both SaO2 and ScO2, but not to SvO2 (Figures B-D).
Conclusions: In this small pilot secondary analysis in preterm neonates, RrSO2 values are consistently lower than blood gas O2 saturations and correlate with both SaO2 and ScO2. Although we hypothesized that SvO2 values would be strongly correlated to RrSO2 given the proximity of the UVC to the renal veins, we did not confirm this hypothesis. Lack of a correlation could be due to the low UVC sample size and lack of statistical power or hindered by improper placement of either the UVC or renal NIRS sensors that could be improved with ultrasound evaluation and placement. Prospective studies will be critical to determine if renal NIRS monitoring truly detects primarily RrSO2 in preterm neonates.
Continuous Glucose Monitoring Facilitates Diazoxide Use in The Management of Glut1 Deficiency Syndrome
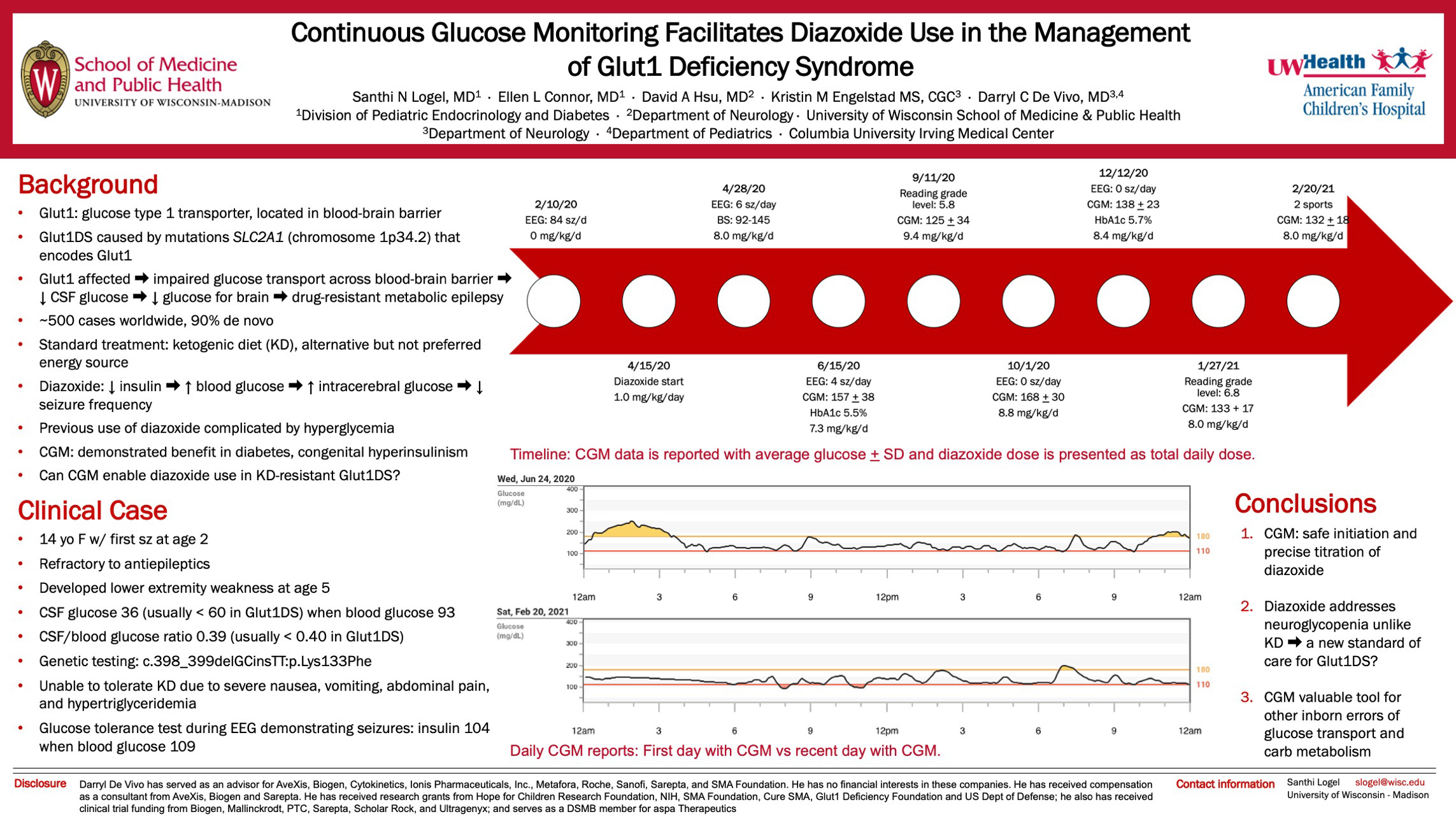
Click here for .pdf version of poster
Title: Continuous Glucose Monitoring Facilitates Diazoxide Use in The Management of Glut1 Deficiency Syndrome
Logel S, Connor E, Hsu D, Engelstad K, De Vivo D
Background: Glut1 deficiency syndrome (Glut1DS) is caused by mutations in SLC2A1 on chromosome 1p34.2, which impairs transmembrane glucose transport across the blood brain barrier resulting in hypoglycorrhachia and decreased glucose availability for brain metabolism. This causes a drug-resistant, metabolic epilepsy due to energy deficiency. Standard treatment for Glut1DS is the ketogenic diet (KD) but treatment options are limited if patients fail the KD. Diazoxide, which inhibits insulin release, was used sparingly in the past for a few Glut1DS patients to increase blood glucose levels and thus intracerebral glucose levels. Unfortunately, their treatment was complicated by unacceptable persistent hyperglycemia with blood glucoses in the 300s to 500s. We investigated the use of a continuous glucose monitor (CGM) to enable titration of diazoxide therapy in a patient with KD-resistant Glut1DS.
Design/Methods: A 14-year-old girl with Glut1DS (c.398_399delGCinsTT:p.Lys133Phe) failed the KD due to severe nausea, vomiting, abdominal pain, and hypertriglyceridemia. Laboratory tests revealed CSF glucose of 36 mg/dL when blood glucose was 93 mg/dL. Over the course of 3 hospitalizations, blood glucose levels in the range of 120-180 mg/dL were targeted with diazoxide.
Results: EEG seizure activity decreased from 3 to 0 absence seizures per hour. CGM placement during the third hospitalization showed an average interstitial glucose of 157 mg/dL with glucose variability of 20.8% on diazoxide dose of 7.3 mg/kg/day. After discharge, CGM was used to adjust diazoxide doses 2-4 times a week to achieve target interstitial glucoses of 140-180 mg/dL. Repeat laboratory tests revealed CSF glucose of 55 mg/dL when interstitial glucose was 158 mg/dL. Current diazoxide dose is 7.9 mg/kg/day and most recent hemoglobin A1c was 5.4%.
Conclusions: This is the first report demonstrating CGM as a tool facilitating the safe initiation and real-time titration of diazoxide in Glut1DS patients who have failed the KD. Diazoxide addresses neuroglycopenia more physiologically by raising blood glucose levels and subsequently intracerebral glucose levels. CGM allows for more accurate titration of blood glucose with diazoxide while avoiding complications of hyperglycemia and thus introduces the possibility of diazoxide becoming a standard of care for Glut1DS. More broadly, CGM provides a valuable tool for the management of other disorders of glucose transport and carbohydrate metabolism.
Feasibility of Remote Transcranial Direct Current Stimulation for Pediatric Cerebral Palsy During the Covid-19 Pandemic
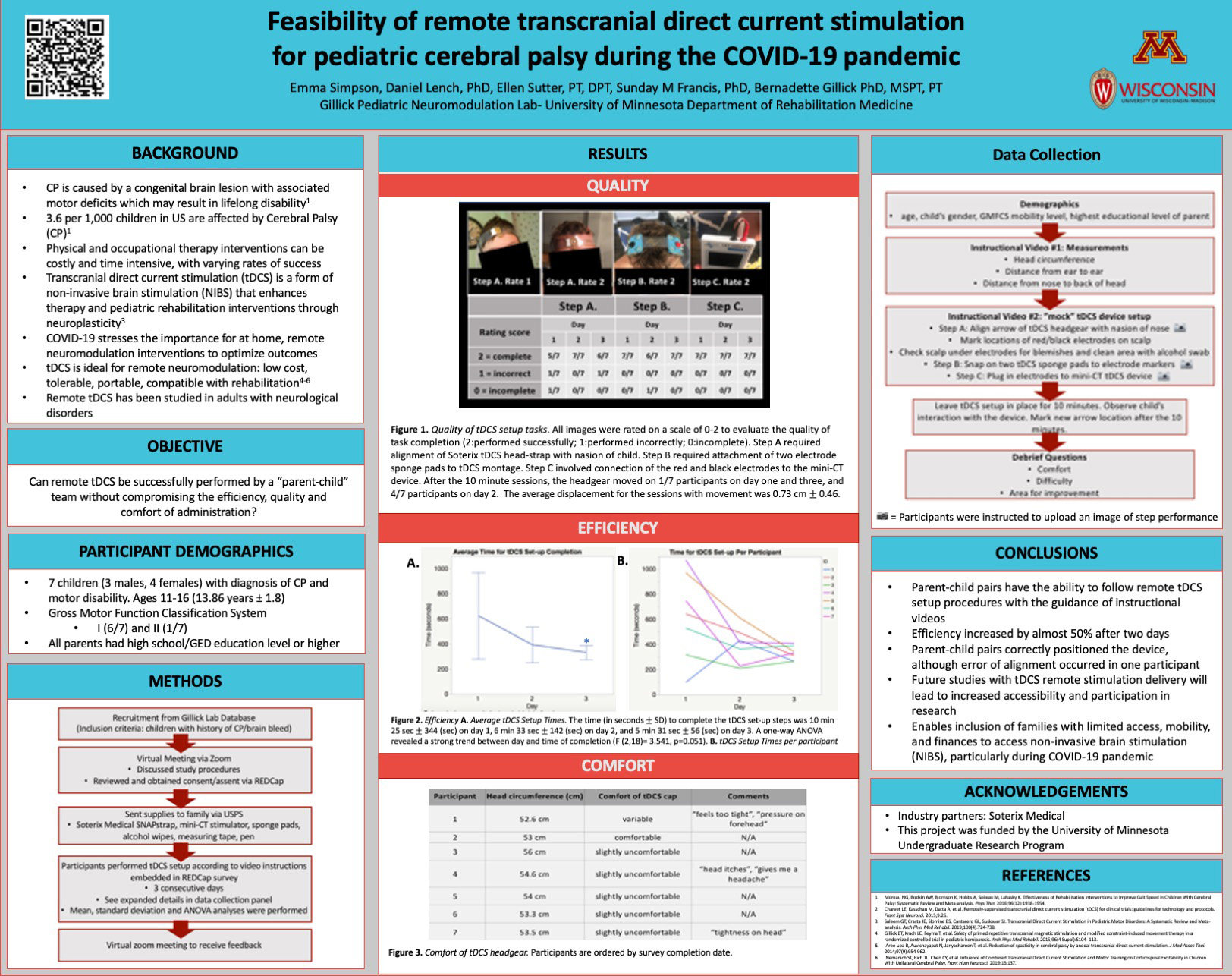
Click here for .pdf version of poster
Title: Feasibility of Remote Transcranial Direct Current Stimulation for Pediatric Cerebral Palsy During the Covid-19 Pandemic
Simpson E, Lench D, Sutter E, Gillick B
Background: Cerebral palsy is caused by a congenital brain lesion that occurs early in life with associated motor deficits which may result in lifelong disability. The brain has high neuroplastic potential early in life, stressing the importance for rehabilitation. Non-invasive brain stimulation (NIBS) including transcranial direct current stimulation (tDCS) may enhance pediatric rehabilitation interventions through neuroplasticity. The Gillick laboratory has previously demonstrated that tDCS is safe, feasible, and successful at modifying motor performance in children with CP in the research setting. Although researched in adults, teleneuromodulation studies of home-based remote stimulation sessions has not occurred in children. We studied the reliability of remote tDCS in a pediatric population due to the increasing need to enhance rehabilitation research for children with limited access to in-person therapies, especially during the COVID-19 pandemic.
Design/Methods: The efficiency, quality, and comfort of unstimulated tDCS administration performed by a “parent-child team” was evaluated. Participants used the Soterix Medical tDCS SNAPstrap and inactive mini-CT device to perform steps including headgear setup, application of sponge electrodes, and connection of the mini-CT device over three consecutive days with the guidance of instructional videos.
Results: The efficiency of the tDCS workflow improved by nearly 50% after the first two days; it was performed 294 seconds faster on day three than on day one. The quality analysis revealed parent-child teams correctly positioned the device on the scalp across multiple days. The headgear was slightly uncomfortable for 5/7 participants.
Conclusions: Parent-child teams have the ability to perform the steps required for remote tDCS. Future studies with monitored remote tDCS stimulation will increase accessibility to NIBS during and after the COVID19 pandemic.
Improvements in Post-Operative Cardiac Surgery Arrhythmia Identification Using the AtriAmp Signals
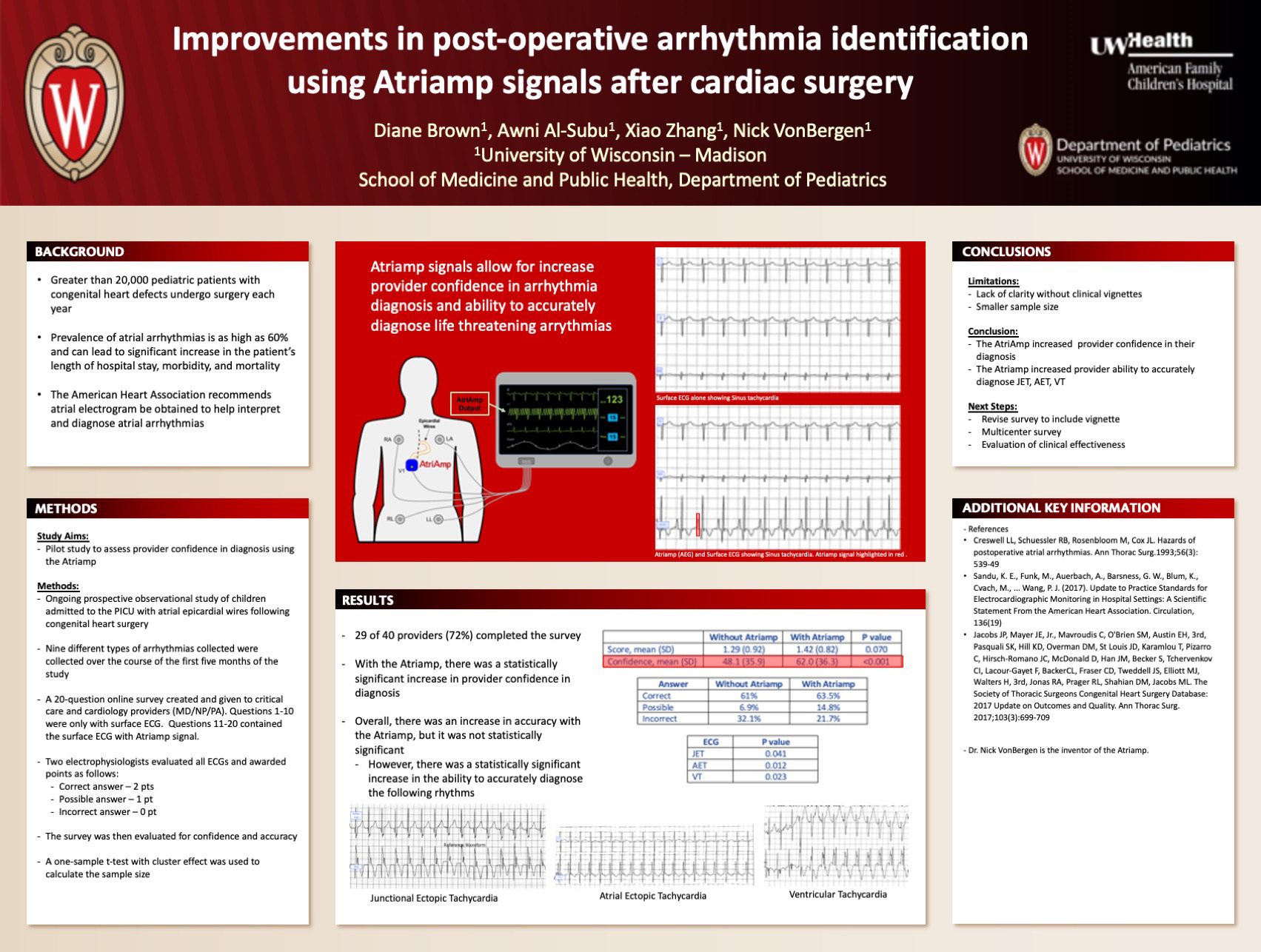
Click here for .pdf version of poster
Title: Improvements in Post-Operative Cardiac Surgery Arrhythmia Identification Using the AtriAmp Signals
Brown D, Zhang X, Al-Subu A, Vonbergen N
Background: Following cardiac surgery, as many as 60% of patients will experience an arrhythmia. These arrhythmias are associated with increased morbidity and occasional mortality. Therefore, rapid and accurate identification is paramount to the improvement of patient outcome. Unfortunately, until now monitoring was limited by lack of timeliness or clarity. Here we evaluate the confidence and accuracy of rhythm diagnosis using the AtriAmp, a UW device that allows continuous arrhythmia monitoring.
Design/Methods: An ongoing IRB approved prospective observational study of children less than or equal to 18 years of age admitted to the PICU with atrial pacing wires following congenital heart surgery. The AtriAmp was connected to atrial pacing wires and e AEG was displayed along with a surface ECG on GE monitors. Nine different types of arrhythmias were collected over the course of the first five months of the study. A 20-question online survey was given to critical care and cardiology providers. Ten questions displayed signals from only the surface leads, while the other ten showed the same arrhythmias with an AEG from the AtriAmp also displayed. Answers were then evaluated for confidence and accuracy.
Results: 40 providers including MDs and NPs were given the survey with 72% (29 providers) completing at the time of this abstract submission. Paired t-tests and mixed effects modeling were used to assess the data. The overall accuracy of diagnosis increased when using the Atriamp signals along with the surface ECG, but it was not statistically significant (p=0.07). Improvements in accuracy were most notable with AET, VT and JET. Provider confidence in diagnosis increased significantly when using the Atriamp signals (48%) compared to using only the surface ECG (62%) to diagnose arrhythmias (p<0.001).
Conclusions: Use of the AtriAmp increased provider confidence in the diagnosis of post-operative arrhythmias when compared to the same arrhythmias seen on surface electrograms. Future research among a larger sample of providers is needed to further evaluate the use of AtriAmp in arrythmia diagnosis.
Performing Minor Urologic Procedures in a Pediatric Sedation Center may be Safe and Cost-Effective: a Pilot Study
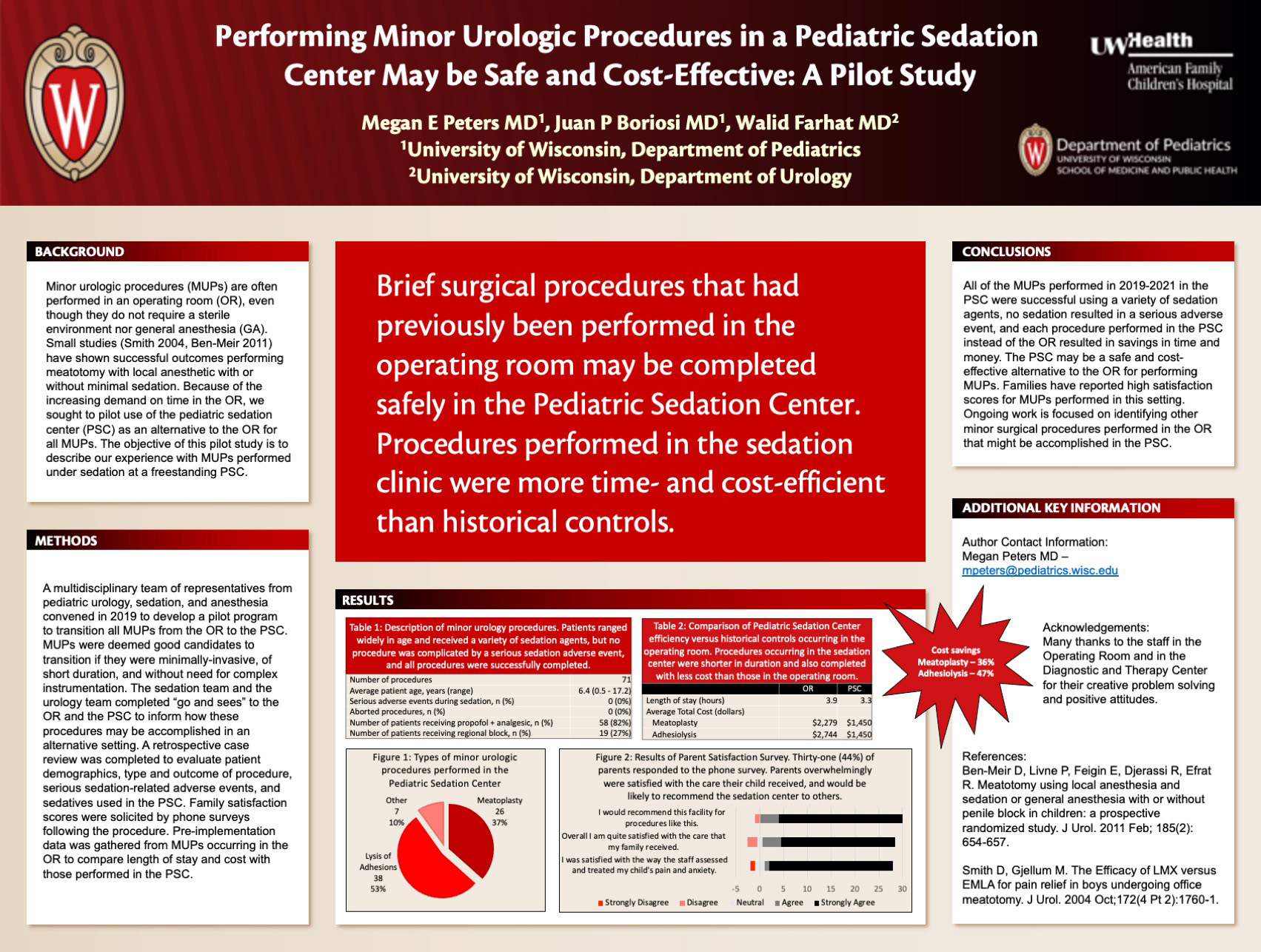
Click here for .pdf version of poster
Title: Performing Minor Urologic Procedures in a Pediatric Sedation Center may be Safe and Cost-Effective: a Pilot Study
Peters M, Boriosi J, Farhat W
Background: Minor urologic procedures (MUPs) are often performed in an operating room (OR), even though they do not require a sterile environment nor general anesthesia (GA). Because of the increasing demand on time in the OR, and because of the importance of providing a high-value experience for patients and their families, we sought to pilot use of the pediatric sedation center (PSC) as an alternative to the OR for all MUPs. The objective of this pilot study is to describe our experience with MUPs performed under sedation at a freestanding PSC.
Design/Methods: A multidisciplinary team of representatives from pediatric urology, sedation, and anesthesia convened in 2019 to develop a pilot program to transition all MUPs from the OR to the PSC. MUPs were deemed good candidates to transition if they were minimally-invasive, of short duration, and without need for complex instrumentation. The sedation team and the urology team completed “go and sees” to the OR and the PSC to inform how these procedures may be accomplished in an alternative setting. A retrospective case review was completed to evaluate patient demographics, type and outcome of procedure, serious adverse events, and sedatives used in the PSC. Family satisfaction scores were solicited by phone surveys following the procedure. Pre-implementation data was gathered from MUPs occurring in the OR to compare length of stay and cost with those performed in the PSC.
Results: Between September 2019 and February 2021 there were 71 MUPs performed in the PSC for children mean age 6 years (6 months to 17 years old): 26 meatoplasty, 38 lysis of penile adhesions, and 7 “other” MUPs. All procedures were successfully completed. There were no serious sedation adverse events. 73% of the procedures were accomplished with a combination of fentanyl and propofol. 26% of patients were given regional anesthetic. Of the 31 (41%) parents who responded to the survey, 83% “strongly agreed” that they were satisfied with their child’s care. Median length of stay in the PSC was 3.3 hours compared with 3.9 hours in the OR. Cost reduction varied by procedure performed, but each procedure performed in the PSC resulted in at least a 36% cost reduction compared with costs in the OR.
Conclusions: The PSC may be a safe and cost-effective alternative to the OR for performing MUPs. Families have reported high satisfaction scores for MUPs performed in this setting. Ongoing work is focused on identifying other minor surgical procedures performed in the OR that might be accomplished in the PSC.
Utility of Neuropsychological Screening in a Multidisciplinary Neurocutaneous Clinic
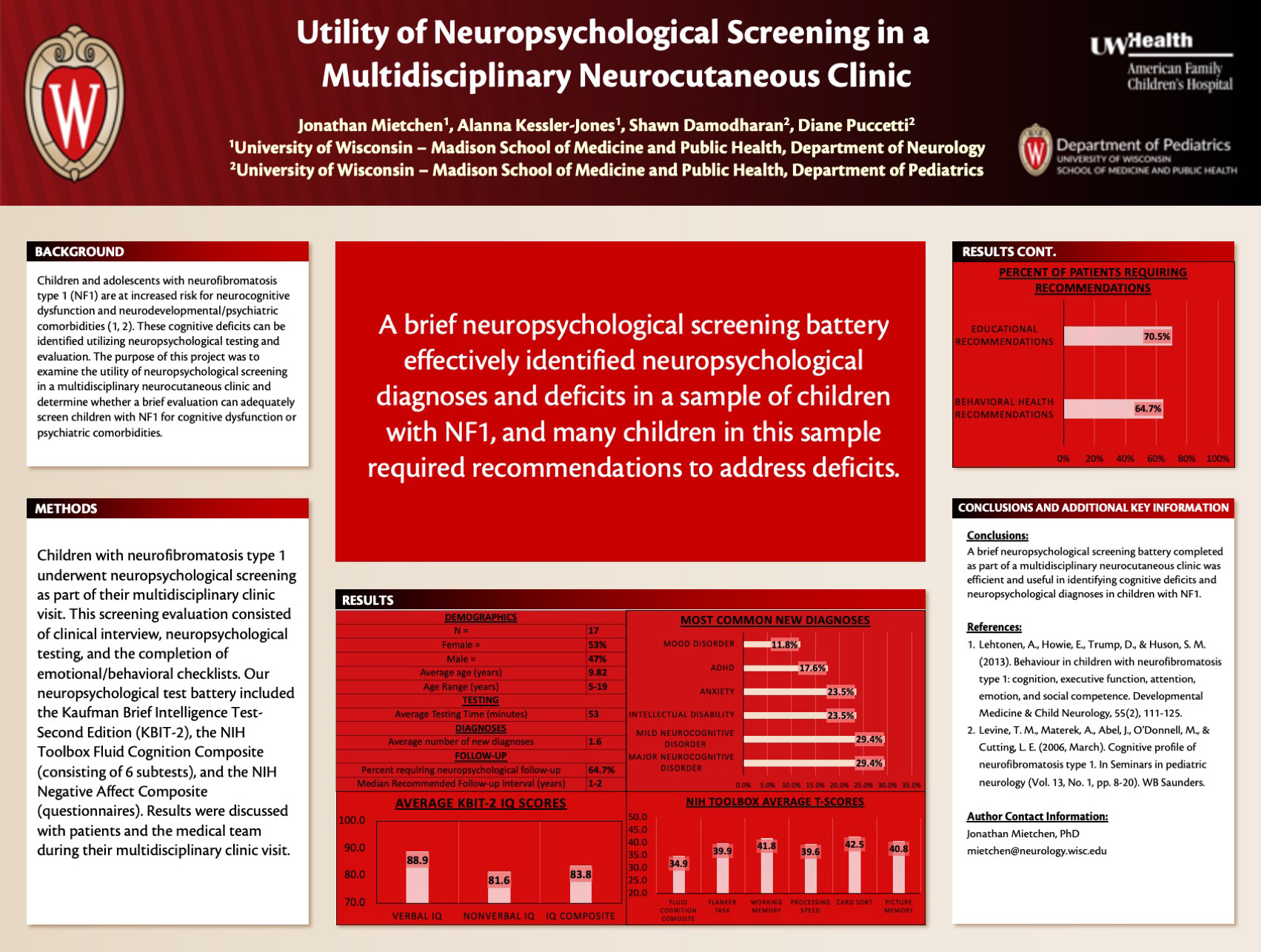
Click here for .pdf version of poster
Title: Utility of Neuropsychological Screening in a Multidisciplinary Neurocutaneous Clinic
Mietchen J, Kessler-Jones A, Puccetti D, Damodharan S
Background: Children with neurofibromatosis type 1 (NF1) are at increased risk for cognitive dysfunction and psychiatric comorbidities. These cognitive deficits can be identified using neuropsychological evaluation. The purpose of this project was to examine the utility of neuropsychological screening in a multidisciplinary neurocutaneous clinic and determine whether a brief evaluation can adequately screen children with NF1 for cognitive dysfunction and psychiatric comorbidities.
Design/Methods: Children underwent neuropsychological screening as part of their multidisciplinary clinic visit. This screening consisted of clinical interview, neuropsychological testing, and the completion of emotional/behavioral checklists. Our neuropsychological test battery included the Kaufman Brief Intelligence Test-Second Edition (KBIT-2) and the NIH Toolbox Fluid Cognition Composite (consisting of 6 subtests).
Results: Over a six-month period 17 children and adolescents with NF1 were seen in our neuropsychology screening clinic. Females made up 53% of the sample. The average age was 9.82 years (range = 5 years–19 years). The average time to complete neuropsychological testing was 53 minutes. Professional units billed by the neuropsychologist included an average of 2.7 hours (median = 3, mode = 3). On average, children in this sample met criteria for 2.1 neuropsychological diagnoses with an average of 1.6 new diagnoses that had not been given prior to their neuropsychological screening. The most common new diagnoses were major or mild neurocognitive disorder (major=29.4%, mild=29.4%), intellectual disability (23.5%), anxiety (23.5%), ADHD (17.6%), and mood disorder (11.8%). On average, children with NF1 performed lower on neurocognitive tests, including intellectual functioning (KBIT-2 Verbal IQ=88.9; KBIT-2 Nonverbal IQ=81.6; KBIT-2 Total IQ=83.75), attention (NIH Flanker T-Score=39.9), working memory (NIH Working Memory T-Score=41.8), processing speed (NIH Processing Speed T-Score=39.6), cognitive flexibility (NIH Card Sort T-Score=42.5), memory (NIH Picture Memory T-Score=40.8), and fluid cognition (NIH Fluid Cognition Composite T-Score=34.36). Behavioral health recommendations were needed for 64.7% of this sample. Educational recommendations were needed for 70.5%.
Conclusions: Neuropsychological screening completed as part of a multidisciplinary neurocutaneous clinic was efficient and useful in identifying cognitive deficits and neuropsychological diagnoses in children with NF1.
Portable Electroretinography (ERG) Goggles for Use in the Pediatric Surgical Suite
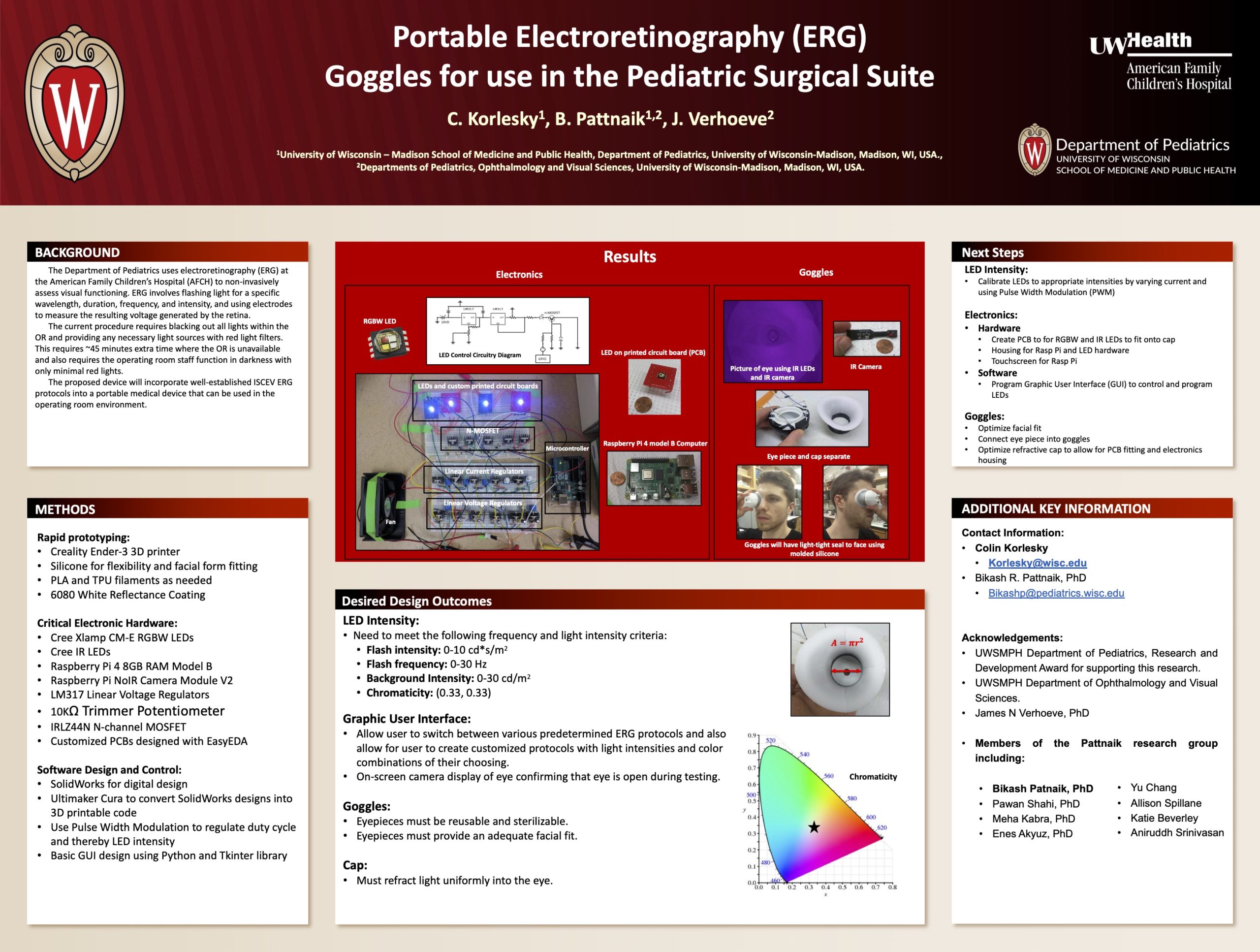
Click here for .pdf version of poster
Title: Portable Electroretinography (ERG) Goggles for Use in the Pediatric Surgical Suite
Korlesky C, Pattnaik B, Verhoeve JN
Background: The Department of Pediatrics currently uses electroretinography (ERG) at the American Family Children’s Hospital (AFCH) surgical rooms as a means of non-invasive objective assessment of visual functioning. The current testing procedure requires exceptional flexibility from operating room staff, is time consuming, cost ineffective, and cannot guarantee the blackout conditions necessary for rod/cone repolarization that is a necessary part of ERG testing. We are currently developing wearable, light-tight goggles that will flash pre-determined light intensities and durations according to established protocols. If design criteria are met, there is further potential in evaluating optic nerve functionality such as seen in optic neuritis (eg multiple sclerosis), ischemia (eg stroke), and compression (eg abscess, adjacent tumor, or optic gliomas). The proposed device will incorporate well-established ERG principals into a portable, wearable medical device that will allow for binocular and monocular light-isolation in the traditional operating room setting.
Design/Methods: For initial rapid prototyping, SolidWorks and 3D printing with PLA is being used. RGBW and IR LEDs controlled with a Graphic User Interphase (GUI) programmed with python. Internal circuitry will ultimately be surface mounted on a custom printed circuit board (PCB) and will include the appropriate electrical components to control the various voltage and current requirements.
Results: The resulting device will allow for monocular and binocular ERG testing without requiring blackout conditions in the surgical suite. A primary prototype is in the process of being developed.
Conclusions: We are in the initial stages of development and cannot yet speak to specific conclusions.
Session D: Education & QI
| Time | Presenter | Title |
|---|---|---|
| 3:30-3:37 | Carolyn Stone, PharmD | An Outpatient Antimicrobial Stewardship Initiative in Pediatric Clinics |
| 3:37-3:44 | Adam Bauer, MD | The Impact of a Scholarly Concentration Program on Medical Student Research in Pediatrics |
| 3:44-3:51 | Aurora Babe Arce, Belinda Islami | A Survey of Cholesterol Disease Management in Pediatric Cardiology |
| 3:51-3:58 | Karen Pletta, MD | Asthma Action Plan Rates: Barriers for Pediatricians and Ideas for Improvement |
| 3:58-4:05 | Asiya Ahmed | Tobacco Use and Nicotine Addiction in Pediatric Cardiology Practices |
| 4:05-4:12 | Stephanie Syu, MD | Lessons Learned from Evaluation of PICC line Utilization at AFCH in 2020 |
| 4:12-4:19 | Paige Condit, MD | Familiarity, comfort and practice incorporation of Adverse Childhood Experiences screening by trainees and established providers |
| 4:19-4:26 | Paige Condit, MD | Perceived Resident Competency in ACGME-Required NICU Procedures |
| 4:26-4:33 | Shane Colvin, MD | Provider Comfort and Knowledge of Pediatric Obesity Comorbidity Screening |
| 4:33-4:40 | Lindsey Cox, MD | Assessing prevalence of sexual activity and contraceptive practices through intake screening of adolescent inpatients |
| 4:40-4:47 | Michelle Brenner, MD | Those that fail to learn from the past are doomed to repeat it”: Characterization of Central Line Associated Bloodstream Infections (CLABSIs) at American Family Children’s Hospital (AFCH) from 2018-2020 |
| 4:47-4:54 | Johanna Sehloff, MD, Rachel Heinze, MD | Pediatric resident knowledge about the push-pull method for rapid intravenous fluid administration |
| 4:54-5:00 | Wrap-Up |
This is an accordion element with a series of buttons that open and close related content panels.
An Outpatient Antimicrobial Stewardship Initiative in Pediatric Clinics
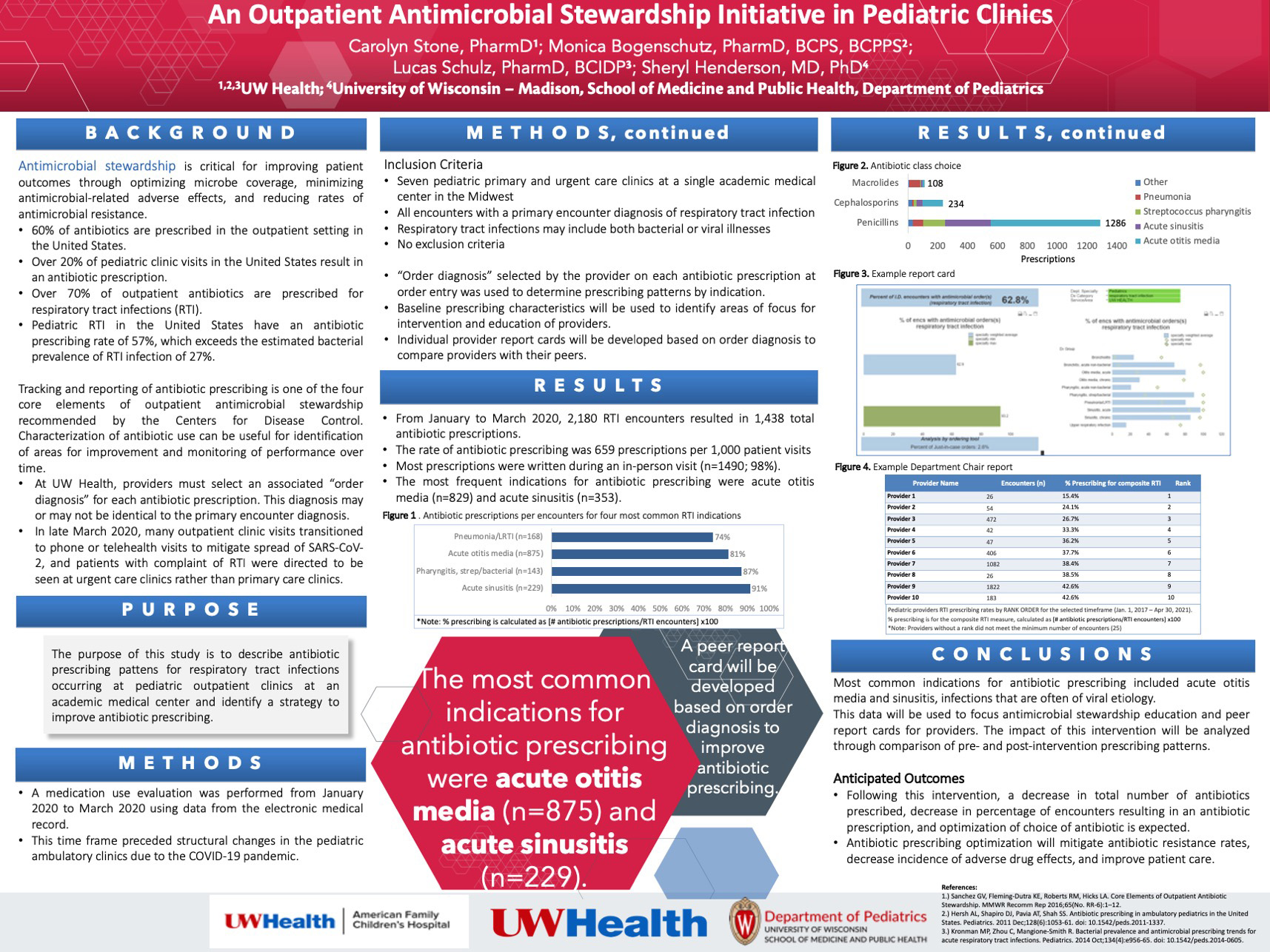
Click here for .pdf version of poster
Title: An Outpatient Antimicrobial Stewardship Initiative in Pediatric Clinics
Stone C, Bogenschutz M, Henderson S, Schulz L
Background: Antimicrobial stewardship improves patient outcomes through optimizing microbe coverage and reducing antimicrobial-related adverse effects. Nearly two-thirds of antibiotics in the United States are prescribed in an ambulatory setting including 21% of all pediatric clinic visits. Respiratory tract infections (RTI) are the most common indications for antibiotics, yet they often have viral causes. Tracking and reporting antibiotic prescribing is a core element of ambulatory antimicrobial stewardship and is used to monitor performance over time and identify improvement opportunities. Provider education and peer comparison improve antibiotic prescribing.
This project describes ambulatory antibiotic prescribing patterns for RTI diagnoses in pediatric clinics at a tertiary health system and identifies a strategy to improve prescribing.
Methods/Design: Baseline prescribing data were collected from January 2020 to March 2020 at five pediatric urgent and primary care clinics using the electronic medical record to assess provider, clinic, and indication information. Only RTI visits (based on encounter diagnosis) and prescriptions were included. Rates of antibiotic use were calculated and reported as prescriptions per 1000 visits and as percent of encounters with an antibiotic prescription.
Results: During the study timeframe, 2180 RTI-encounters generated 1438 antibiotic prescriptions (659 prescriptions/1000 visits). The most common diagnoses generating prescriptions were acute otitis media (708/875 encounters; 80.9%), acute sinusitis (209/229; 91.3%), and streptococcus pharyngitis (125/143; 87.4%). The most common antibiotic class prescribed was penicillins (1093 prescriptions). These results demonstrate opportunities for antibiotic prescribing improvement. A pediatric workgroup has identified two strategies to improve RTI antibiotic prescribing – education and provider peer comparison report cards.
Conclusions: Through development and implementation of a peer comparison report card coupled with provider education, we anticipate increased use of non-antibiotic treatment strategies and reduced antibiotic utilization measured by number of antibiotics prescribed, percent of encounters resulting in an antibiotic prescription, and optimized antibiotic choice, which will help mitigate community antibiotic resistance rates, decrease incidence of adverse drug effects, and improve patient care.
The Impact of a Scholarly Concentration Program on Medical Student Research in Pediatrics
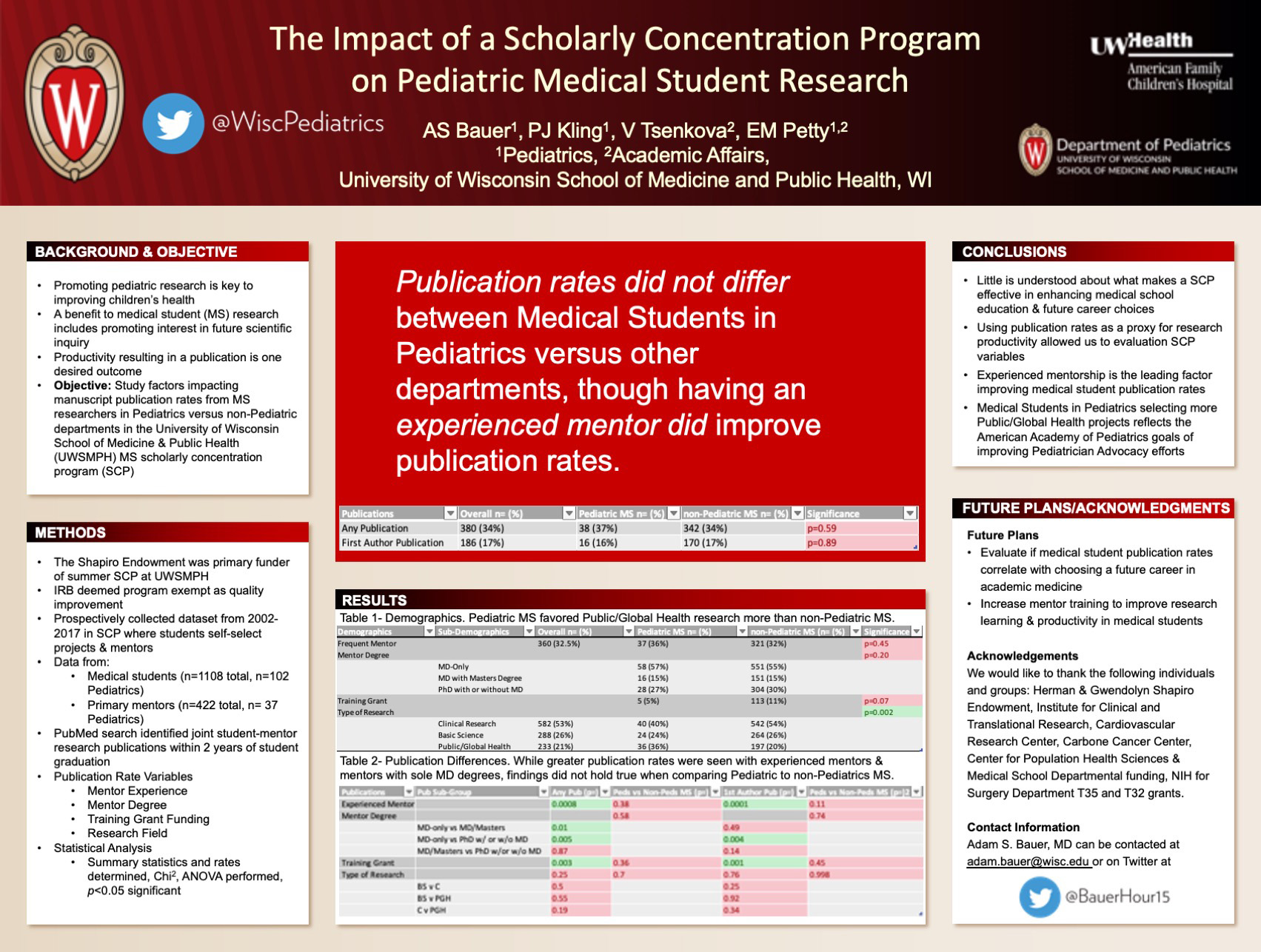
Click here for .pdf version of poster
Title: The Impact of a Scholarly Concentration Program on Medical Student Research in Pediatrics
Bauer A, Kling P Tsenkova V, Petty, E
Background: To promote scientific inquiry, medical schools provide scholarly concentration programs (SCP) for medical students (MS), such as the Shapiro Program at the University of Wisconsin School of Medicine and Public Health (UWSMPH). MS research productivity improves student satisfaction, but factors contributing to productivity are unknown. Because of unique challenges of research in Pediatrics, we examined UWSMPH MS research productivity in Pediatrics, compared to other departments. Productivity was defined as publication rates. Secondary aims examined whether publication rates were influenced by: 1. Mentor Experience, 2. Mentor degree, 3. Training grant funding, and 4. Research field.
Design/Methods: The IRB QI/Program evaluation tool determined exemption from review. We collected program data and searched PubMed for joint mentor/MS publications within 2 years of graduation.
Results: Between 2002-2017, 1108 MS self-selected mentors, with 9.2% in Pediatrics. 34% of MS published at least 1 manuscript. Pediatrics did not differ from other departments (p=0.6) in publication rates. Having an experienced mentor improved publication rates (p=0.0008). We observed that mentoring by MD only mentors resulted higher publication rates compared to MD with masters’ degree mentors (p=0.01) and compared to PhD with or without MD mentors (p=0.005). We found that MS funding with training grants had higher publication rates (p=0.003) and first author publication rates (p=0.001). In multivariate analysis, we found the significance of publication rates was lost when comparing Pediatrics to other departments in mentor degree (p=0.5) and type of training grant (p=0.36). MS in Pediatrics favored public/global health research over basic science or clinical research as compared to other departments (p=0.002). While in Pediatrics, publication rates did not differ depending upon research field (p=0.47), in other departments there was increased publication rates in clinical research as compared to public/global health and basic sciences (p=0.046).
Conclusions: Pediatricians play a key role in training MS researchers. Further mentor training will likely improve research productivity in MS researchers and would improve MS satisfaction with the SCP.
A Survey of Cholesterol Disease Management in Pediatric Cardiology
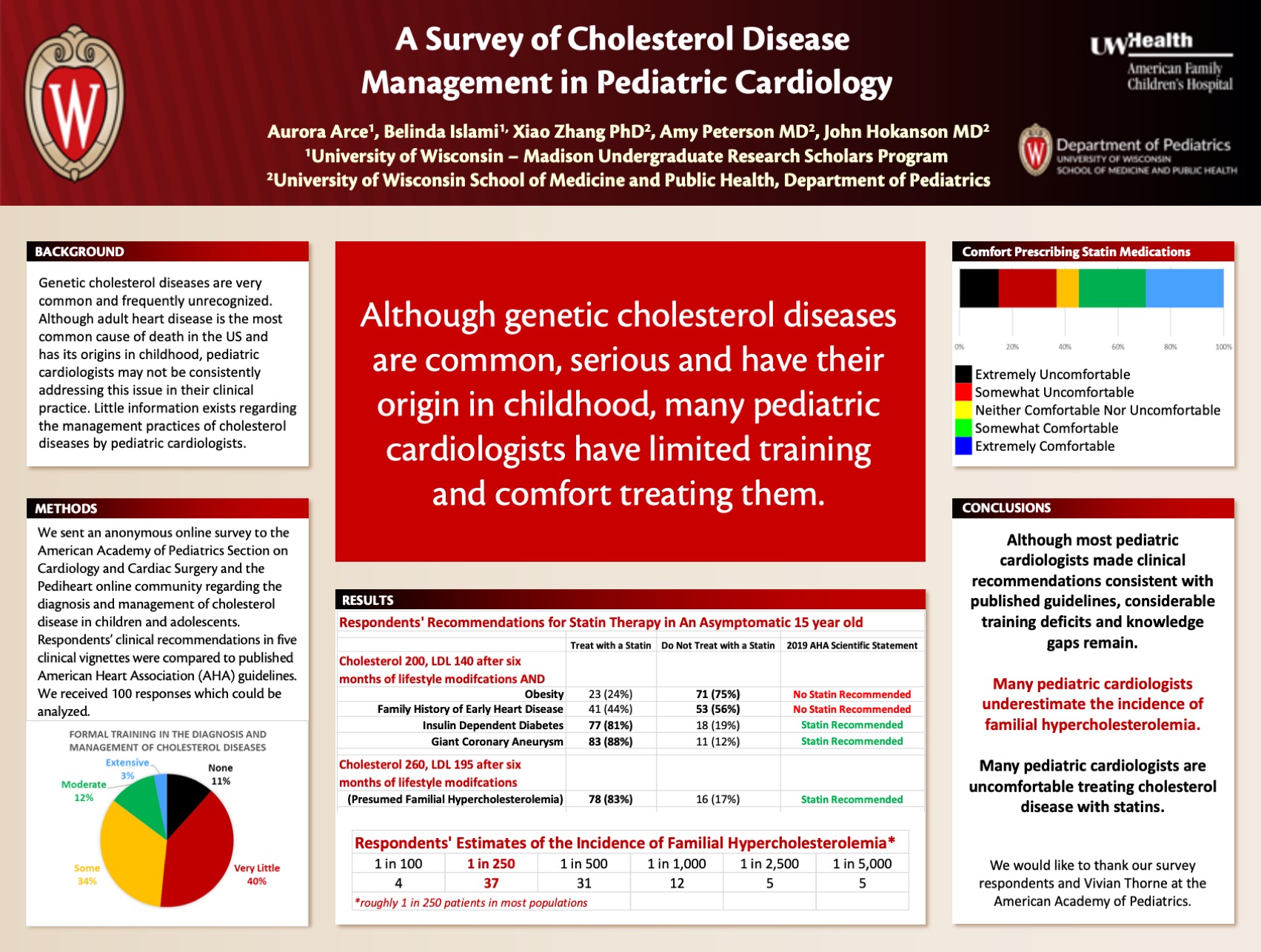
Click here for .pdf version of poster
Title: A Survey of Cholesterol Disease Management in Pediatric Cardiology
Arce A, Islami B, Peterson A, Hokanson
Background: Genetic cholesterol diseases are very common and frequently unrecognized. Although adult heart disease is the most common cause of death in the US and has its origins in childhood, pediatric cardiologists may not be consistently addressing this issue in their clinical practice. Little information exists regarding the management practices of cholesterol diseases by pediatric cardiologists.
Design/Methods: We created an online survey to addresses how pediatric cardiologists approach cholesterol screenings and cholesterol disease management. Respondents were asked questions about their formal training in the diagnosis and management of cholesterol diseases. They were also asked about their comfort using statins (cholesterol reducing drugs). We asked for their treatment recommendations for five hypothetical patients which were then compared to standard recommendations from the American Heart Association (AHA) guidelines.
Results: One hundred individuals completed the survey. The majority of respondents (85.3%) reported that they had some to no training in cholesterol disease management, and 14.7% reported having moderate to extensive training. A little more than half of respondents (54.7%) reported being somewhat comfortable to extremely comfortable prescribing a statin. For two of the vignettes presented, AHA guidelines would not recommend a statin. Most respondents appropriately chose not to treat with a statin in the case of obesity (75%) and family history of early heart disease (56%).
For the other three vignettes, AHA guidelines would recommend treatment with a statin. Most respondents appropriately chose to treat with a statin in the case of a giant coronary aneurysm (88%), familial hypercholesterolemia (83%) and insulin dependent diabetes (81%).
Conclusions: Overall, pediatric cardiologists gave recommendations consistent with guidelines. Unfortunately, many pediatric cardiologists still report gaps in training regarding pediatric cholesterol management. Additional pediatric cholesterol education represents an opportunity to improve the care of children with cholesterol diseases.
Asthma Action Plan Rates: Barriers for Pediatricians and Ideas for Improvement
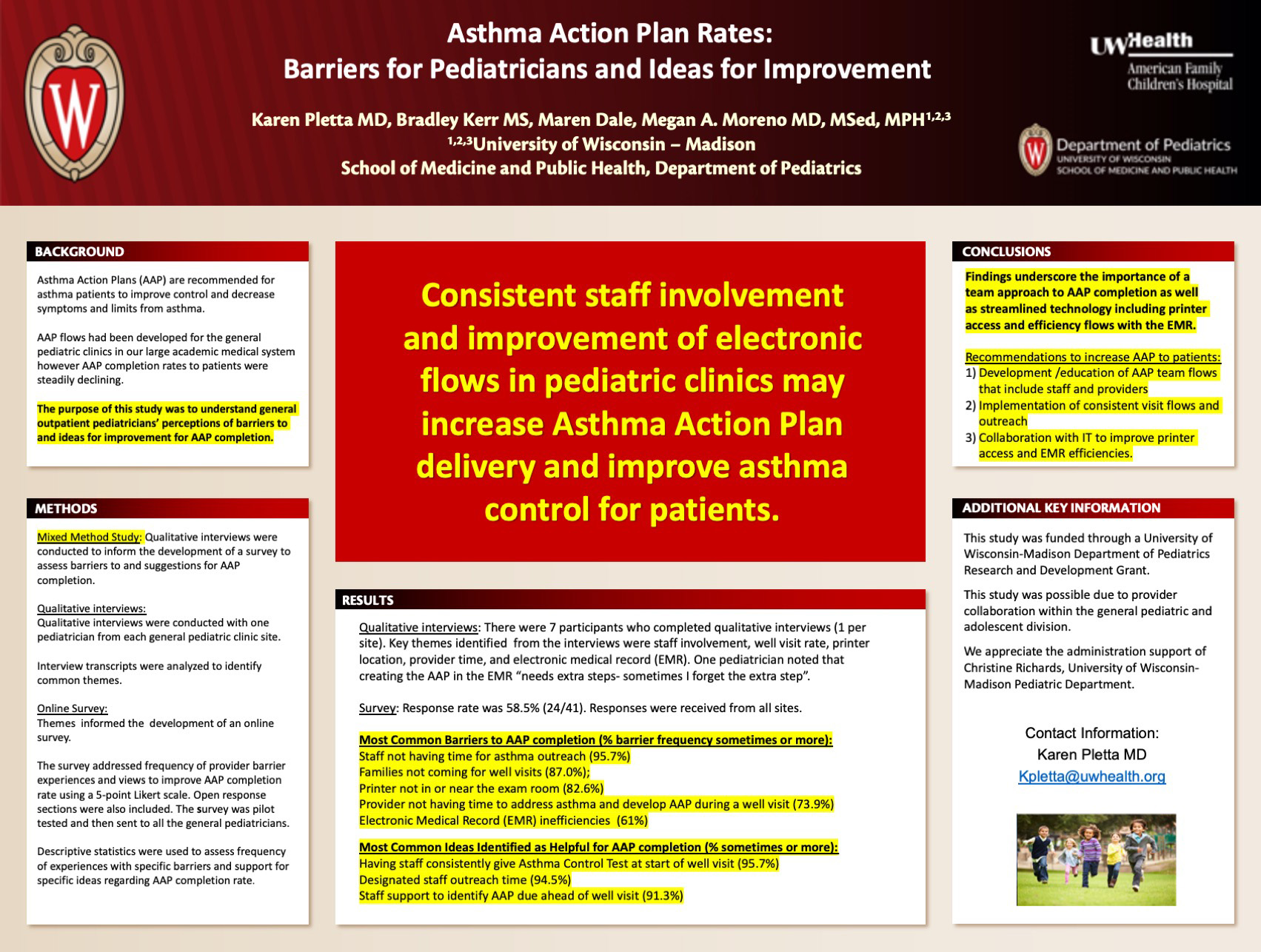
Click here for .pdf version of poster
Title: Asthma Action Plan Rates: Barriers for Pediatricians and Ideas for Improvement
Pletta K, Kerr B, Dale M, Moreno M
Background: Asthma Action Plans (AAP) are recommended by the American Academy of Pediatrics to decrease negative outcomes and improve asthma control for pediatric asthma patients. AAP completion rates in the general pediatric clinics of our large academic medical system were steadily declining. The purpose of this study was to understand pediatricians’ perceptions of barriers to and ideas for improvement for AAP completion.
Design/Methods: This mixed method study recruited pediatricians from general pediatric clinics in a large medical system. Qualitative interviews were conducted with a pediatrician from each clinic site to identify barriers to and ideas for improvement for AAP completion. Interview transcripts were analyzed to identify common themes, which informed the development of an online survey. The survey was pilot tested among pediatricians and distributed by email to all clinic pediatricians. Descriptive statistics were used to assess frequency of experiences with barriers and support for ideas to improve the AAP completion rate.
Results: Key themes from the 7 interviews were staff involvement, well visit rate, provider time, printer location and electronic medical record (EMR). One pediatrician noted that creating an AAP in the EMR “needs extra steps – sometimes I forget the extra step.” Among 41 eligible faculty, 24 completed the survey (58.5%). The most commonly reported barriers experienced sometimes to very often were 1) Staff not having time for asthma outreach (95.7%, n= 22), 2) Families not coming for well visits (87.0%, n= 20), 3) Printer not in or near the exam room (82.6%, n=19) and 4) Provider not having time to address asthma and develop an AAP during a well visit (both 73.9%, n=17). Additionally, participants noted barriers from the EMR (60.9%, n=14) and Staff not giving Asthma Control Test (ACT) at start of well visit (56%, n=13). Ideas reported as helpful sometimes or more for improving AAP completion were 1) Having staff consistently give ACT at start of well visit (95.7%, n=22), 2) Designated staff outreach time (94.5%, n=21) and 3) Staff support to identify AAP due ahead of well visit (91.3%, n=21).
Conclusions: Findings underscore the importance of a team approach to AAP completion as well as streamlined technology including printer access and efficient flows with the EMR. Staff involvement and improvement of electronic flows in pediatric clinics may increase AAP delivery to patients and improve asthma control for children.
Tobacco Use and Nicotine Addiction in Pediatric Cardiology Practices
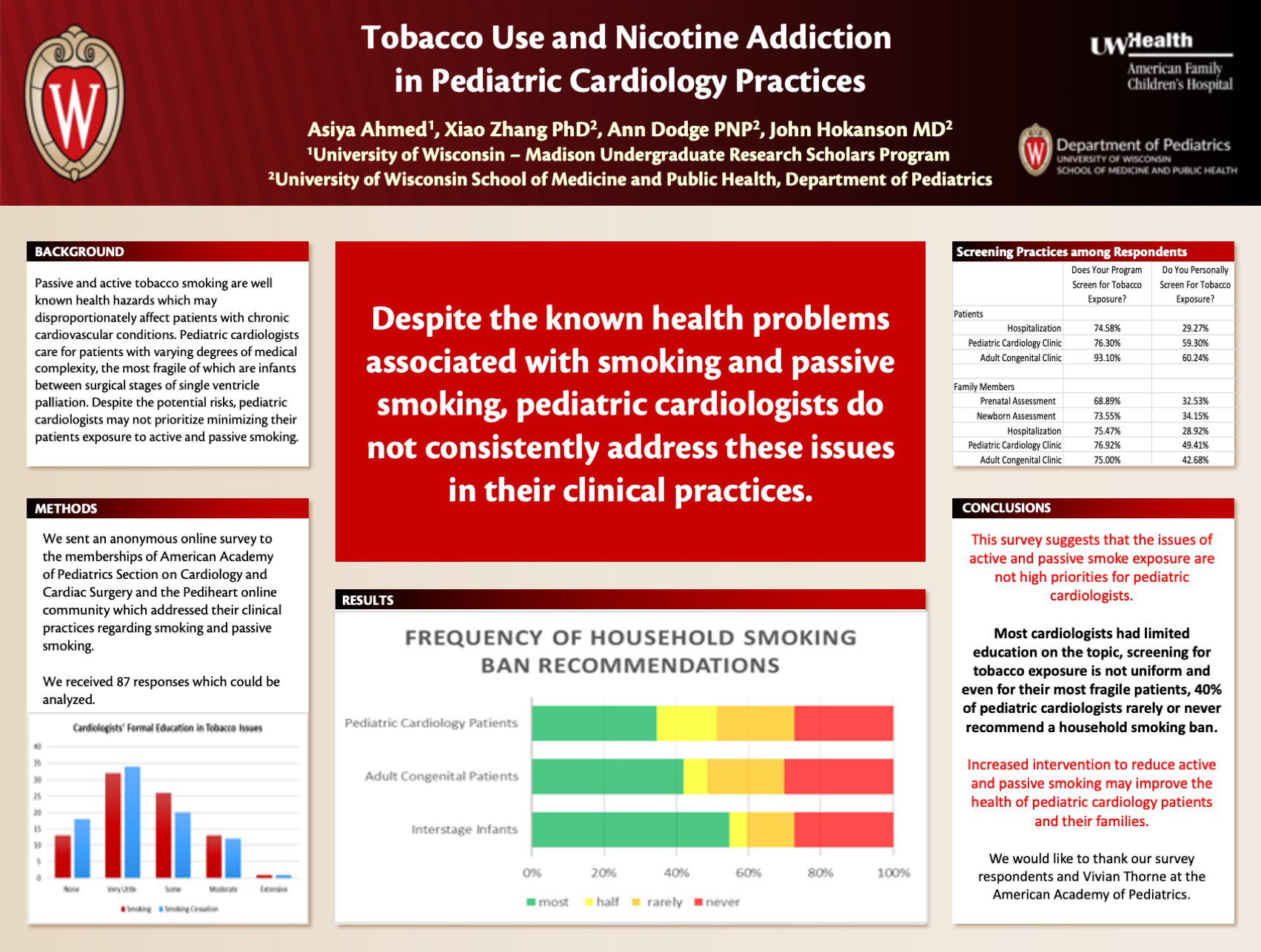
Click here for .pdf version of poster
Title: Tobacco Use and Nicotine Addiction in Pediatric Cardiology Practices
Ahmed A, Dodge A, Hokanson J
Background: Pediatric cardiologists, who would presumably recognize tobacco use and exposure to be health hazards, may not address this risk in their clinical practice. They might underestimate the urgency of the topic or don’t see managing this risk as part of their role. We sought to determine the current clinical practice patterns of pediatric cardiologists with regard to smoking and passive smoking in their clinical practices.
Design/Methods: We sent an anonymous electronic survey to the membership of the American Academy of Pediatrics Section on Cardiology and Cardiac Surgery and the Pediheart online community in February 2021. This survey addressed their training in tobacco related issues, their current practices in screening for smoking and secondhand smoke and their recommendations in clinical practice. This study was reviewed and approved by the University of Wisconsin Health Sciences Institutional Review Board.
Results: 82 of 87 respondents were pediatric cardiologists. Respondents had a range of 1 to 33 years in practice. More than half (52.3%) had very little or no formal training regarding tobacco addiction. Their programs screened patients in the following settings: hospitalization (74.6%), outpatient pediatric visits (76.3%), and outpatient adult congenital visits (93.1%). They personally screened patients 29.3% for hospitalization, 59.3% for outpatient pediatric visits, and 60.2% for outpatient adult congenital visits. For screening parents and other household members, most answered yes that their programs do screen, while most answered they personally do not. Respondents answered that lack of time (44.9%) and “not my role in patient care” (21.5%) as the main barriers they face. 27% said they do not advise a smoking ban in the homes of any of their patients. Pediatric cardiologists rarely or never advise a smoking ban in the following contexts: adult congenital heart disease patients 51.3%, general pediatric cardiology patients 48.8% and interstage single ventricle infants (arguably their highest risk patients) 40.5%.
Conclusions: The findings from this survey suggests that pediatric cardiologists do not routinely appear to place a high priority on addressing smoking and secondhand smoke exposure in their day to day practices despite the known risks associated with tobacco use and exposure.
Lessons Learned from Evaluation Of PICC Line Utilization at AFCH in 2020
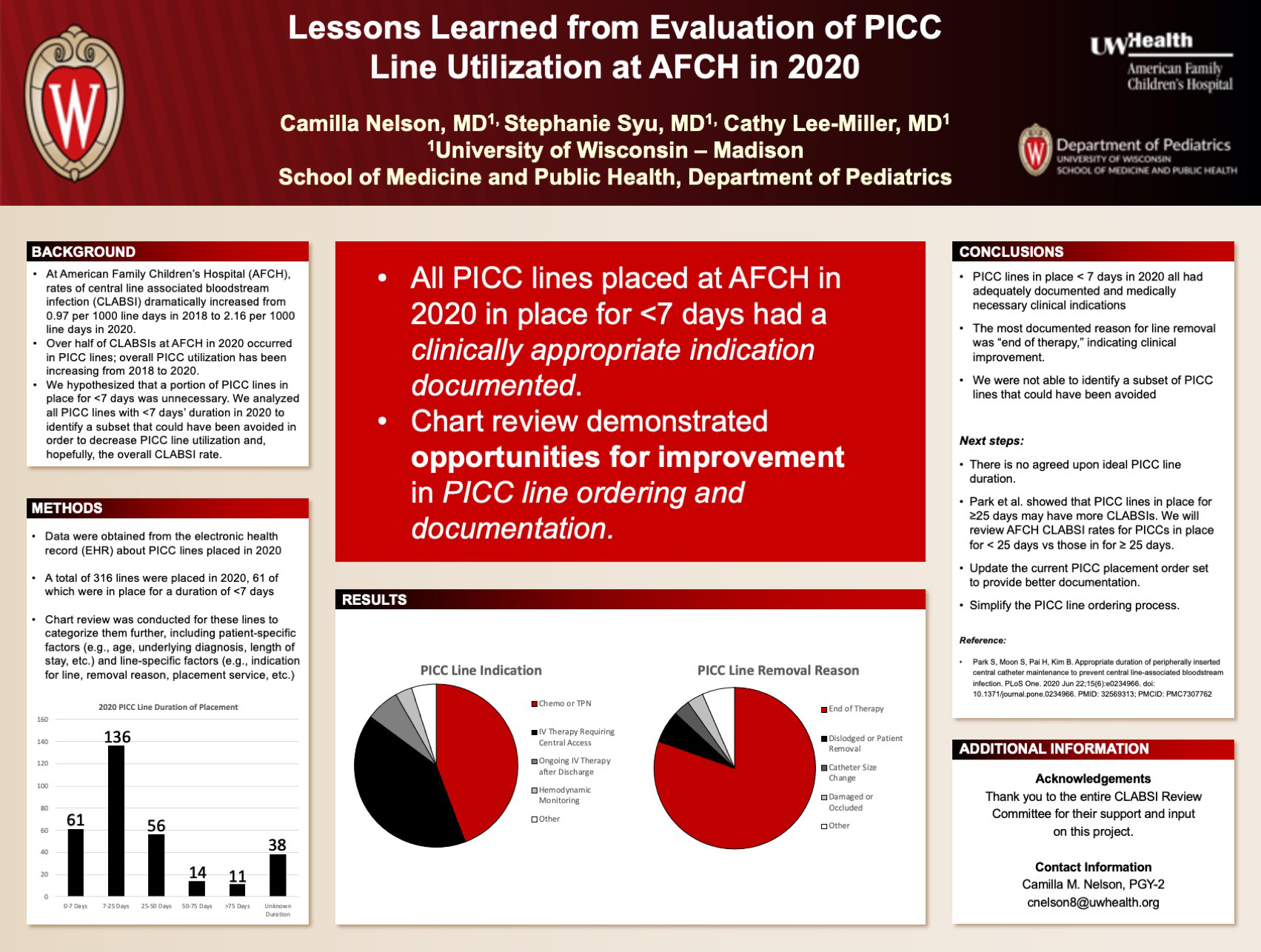
Click here for .pdf version of poster
Title: Lessons Learned from Evaluation Of PICC Line Utilization at AFCH in 2020
Nelson C, Syu S, Lee-Miller C
Background: At the American Family Children’s Hospital (AFCH), CLABSI (central line associated blood stream infection) rates dramatically increased from 2018 to 2020, leading to the creation of a multidisciplinary review committee. The CLABSI rate increased from 0.94 per 1000 line days in 2018 to 0.97 in 2019 to 2.14 in 2020. Of the 18 CLABSIs in 2020, 10 occurred in patients with PICC (peripherally inserted central catheter) lines in place. Over the same time period, there has been a small increase in the number of PICC lines placed as well. A sub-committee was formed to analyze PICC line data in 2020. By reviewing the data for PICC lines placed for 7 days or fewer, we hoped to identify areas of improvement to decrease number of PICC lines utilized and to identify opportunities to decrease CLABSI rates.
Design/Methods: Using a compilation of data of PICC lines placed in 2020 at AFCH from the EHR (electronic health record), we identified a total of 316 PICC lines placed in patients aged 0 – 18 years old. From this group, 61 PICC lines were in place for fewer than 7 days. A thorough chart review of these 61 lines was performed to confirm PICC placement date, duration, placement indication and removal reason. This project was considered IRB-exempt.
Results: Of the 61 PICC lines in place for fewer than 7 days in 2020, the most common indications were “TPN or Chemotherapy” (27) or “IV therapy requiring central access” (25). Removal reason was documented as “completion of therapy” in 47 of 61 lines. Of the 61 patients reviewed, only 4 had another PICC placed within 48 hours after the initial PICC was removed.
Conclusions: Our chart review confirmed that all the PICC lines placed for 7 days or fewer had a clinical indication documented with adequate clinical reasoning and the most common reason for removal was clinical improvement of the patient. Based on this analysis of short duration PICC lines, we were unable to identify practice changes that would decrease the overall number of PICC lines placed at AFCH. Our next steps will be to determine CLABSI rates in PICC lines in place for fewer than 25 days versus those in for greater than 25 days. We also plan to update the current PICC placement order to provide more granular reasons for PICC line placement and removal.
Differences in Familiarity, Comfort and Practice Incorporation of Adverse Childhood Experiences Screening by Trainees and Established Providers

Click here for .pdf version of poster
Title: Differences in Familiarity, Comfort and Practice Incorporation of Adverse Childhood Experiences Screening by Trainees and Established Providers
Condit P, Williams Al-Kharusy S, Sherfinski H, Lasarev M, Sklansky D, Moreno M
Background: Adverse childhood experiences (ACEs) were introduced in the 1998 CDC-Kaiser study, illuminating an array of traumatic events that increase a child’s risk of developing numerous chronic illnesses associated with substantial morbidity and mortality. Despite the CDC-Kaiser study, ACEs are not universally screened for in pediatric clinics and there is no American Academy of Pediatrics clinical practice guideline for ACEs screening. The objective of this study is to characterize trainee and established provider familiarity and comfort with ACEs and ACEs screening and identify variables that may influence incorporation of ACEs knowledge into practice.
Design/Methods: In this cross-sectional survey study, medical students (MS), residents(R), advanced practitioners (APP) and attending physicians(A) in Family Medicine and Pediatrics were recruited by email. The 21-item survey included predominantly Likert format questions assessing comfort and familiarity with ACEs and ACEs screening. Data were compared across groups using chi-square, Fisher’s exact, or non-parametric Kruskal-Wallis tests with follow-up pairwise comparisons based Nemenyi’s procedure.
Results: 274 surveys were completed. Of respondents, 40.1% were MS, 18.6% were R, 3.6% were APP and 37.6% were A. MS had less familiarity with the CDC-Kaiser ACEs study than R (p=0.001) and A (p=0.002). Education about ACEs was more commonly included during training among MS (50%) and R (69%) compared to A (20%, p<0.001 for each comparison). R and A had similar comfort discussing ACEs with patients (92% R and 91% A were at least somewhat comfortable) and reported similar frequencies of screening in their clinics (51% R and 39% A sometimes or frequently screened) yet the majority of both groups (61% R and 70% A) indicated the process is not standardized. A greater percentage of R not currently screening (70%) indicated interest in implementing ACEs screening compared to A (59%), though not statistically significant (p=0.896). MS were more interested in implementing screening than A (p=0.023).
Conclusions: Trainees had more experience and interest in ACEs screening than established providers. This finding could be due to increasing incorporation of ACEs education during training, however, more research evaluating barriers to ACEs screening is needed. Next steps to increasing ACEs familiarity and screening could include improved education for established providers and validated tools.
Perceived Resident Competency in ACGME-Required NICU Procedures
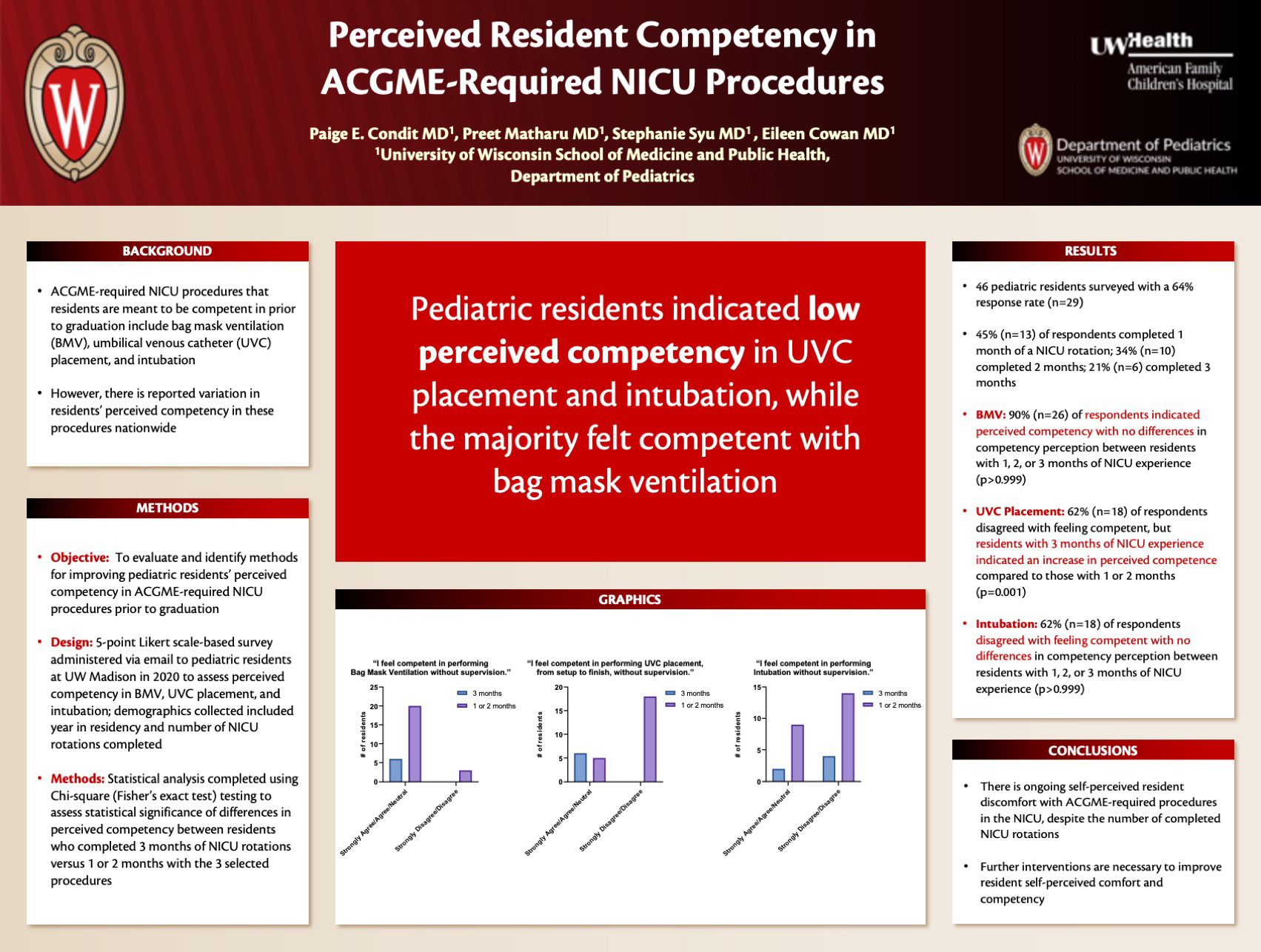
Click here for a .pdf version of poster
Title: Perceived Resident Competency in ACGME-Required NICU Procedures
Condit P, Matharu P, Syu S, Cowan E
Background: The Accreditation Council for Graduate Medical Education (ACGME) has established requirements for achieving competency in selected Neonatal Intensive Care Unit (NICU) procedures prior to graduating from a pediatrics residency program. These include Bag Mask Ventilation (BMV), Umbilical Venous Catheter (UVC) placement, and intubation. However, despite these requirements, American Academy of Pediatrics (AAP)-led national studies have demonstrated a wide variance regarding residents’ perceived competency in completing these procedures. Studies have demonstrated more opportunities to perform procedures leads to increased confidence, self-perceived competency, and perceived competency by program directors/attendings in performing vital skills such as neonatal resuscitation. The purpose of this study is to evaluate and identify methods for improving pediatric residents’ perceived comfort and competence in ACGME-required NICU procedures prior to graduation.
Design/Methods: A survey was administered via email to residents in our Midwest pediatric residency program to assess current perceived competency in BMV, UVC placement, and intubation using a 5-point Likert scale (Strongly Disagree to Strongly Agree). Additionally, we assessed the association of perceived competency and number of completed rotations in the NICU. Chi square analysis (Fisher’s exact test) was completed to assess statistical significance of differences in perceived competency between residents who completed 3 months of NICU rotations versus 1 or 2 months.
Results: Of 46 pediatrics residents surveyed, 64% responded (n=29). Thirteen respondents completed 1 month of a NICU rotation, 10 completed 2 months, and 6 completed 3 months. 90% (n=26) of respondents indicated perceived competency with BMV. 62% (n=18) of respondents disagreed with feeling competent with intubation and UVC placement. There was no significant difference in perceived procedural competence between the resident groups with 1, 2, or 3 months of rotation experience for BMV and intubation (p>0.999 BMV and intubation). However, residents with 3 months of experience indicated an increase in perceived competence than those with 1 or 2 months of experience (p= 0.001) with UVC placement.
Conclusions: Survey data demonstrates ongoing perceived discomfort in ACGME-required NICU procedures for residents, regardless of the number of completed rotations. As such, there is a need for interventions to improve resident perceived competency selected NICU procedures.
Provider Comfort & Knowledge of Pediatrics Obesity Comorbidity Screening
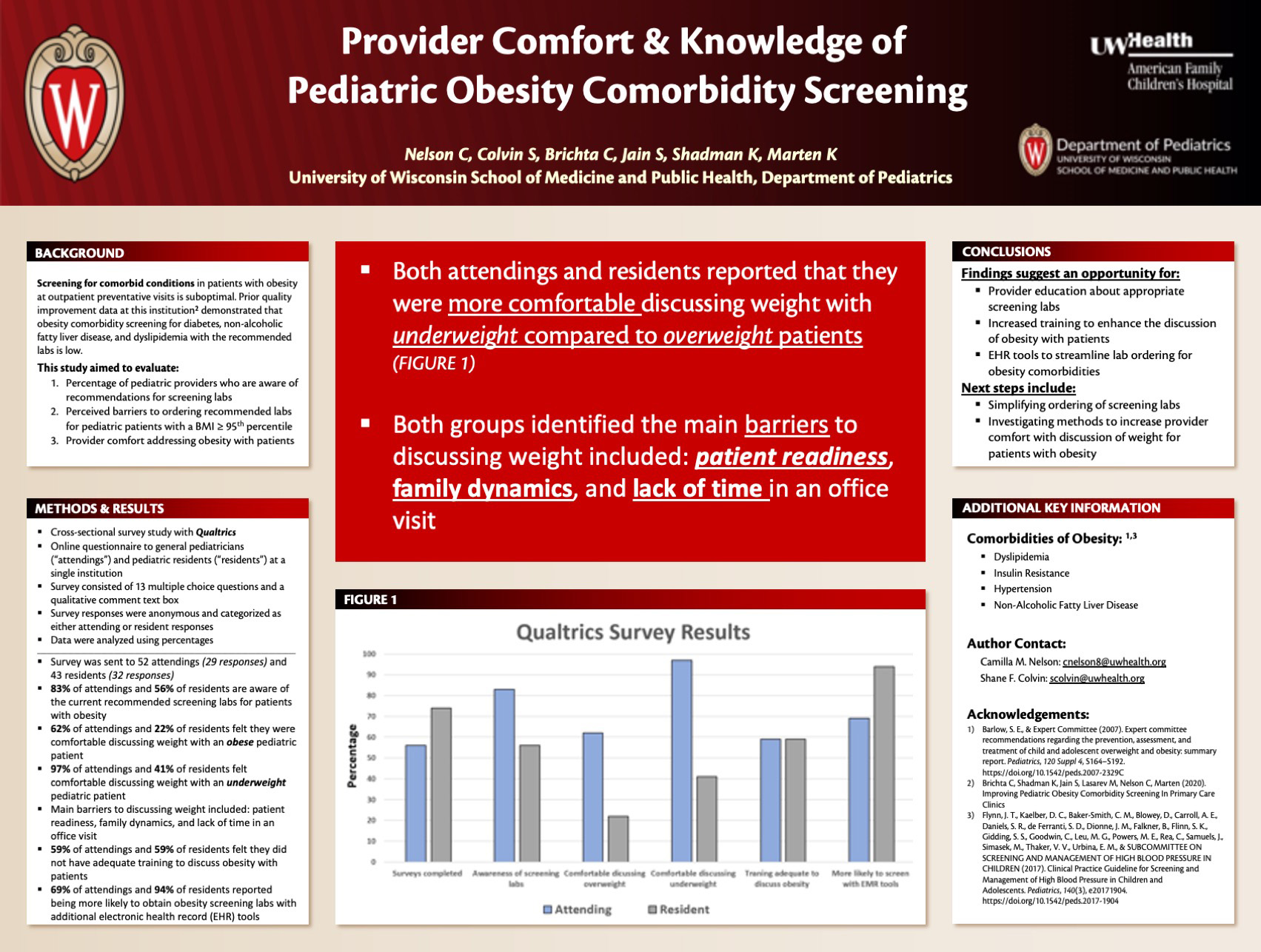
Click here for .pdf version of poster
Title: Provider Comfort & Knowledge of Pediatrics Obesity Comorbidity Screening
Nelson C, Colvin S, Brichta C, Jain S, Shadman K, Marten K
Background: Screening for comorbid conditions in obese patients at outpatient preventative visits is suboptimal. Prior quality improvement data at this institution demonstrated that obesity co-morbidity screening for diabetes, non-alcoholic fatty liver disease, and dyslipidemia with the recommended labs is low. This study aimed to evaluate: (1) The percentage of pediatric providers that know the recommendations for screening labs (2) Perceived barriers to ordering the recommended labs for pediatric patients with a BMI > 95th percentile, and (3) Provider comfort addressing obesity with patients.
Design/Methods: This was a cross-sectional survey study conducted by distributing an online questionnaire to general pediatricians (“attendings”) and pediatric residents (“residents”) at a single institution. The survey consisted of 13 multiple choice questions and a qualitative comment text box. The survey responses were anonymous, and categorized as either attending or resident responses. Data were analyzed using percentages.
Results: The survey was sent to 52 attendings and 43 residents, and yielded 29 responses from attendings and 32 responses from residents. Response review demonstrated that 83% of attendings and 56% of residents were aware of the current recommended screening labs for obese pediatric patients. Only 62% of attendings and 22% of residents felt they were comfortable discussing weight with an obese patient. Alternatively, 97% of attendings and 41% of residents felt comfortable discussing weight with an underweight patient. Both groups identified that the main barriers to discussing weight included patient readiness, family dynamics, and lack of time in an office visit. Just over half (59%) of both attendings and residents felt they did not have adequate training to discuss obesity with patients and the majority of both groups would like more training in counseling these patients. Interestingly, residents (94%) reported being more likely to obtain obesity screening labs if they had additional electronic health record (EHR) tools, compared to the attendings (69%).
Conclusions: These findings suggest a need for provider education about appropriate screening labs, increased training to enhance the discussion of obesity with patients, and an interest in EHR tools to streamline lab ordering for obesity comorbidities. Next steps include simplifying the ordering of screening labs and investigating methods to increase provider comfort with discussion of weight for obese patients.
Assessing Prevalence of Sexual Activity and Contraceptive Practices Through Intake Screening of Adolescent Inpatients
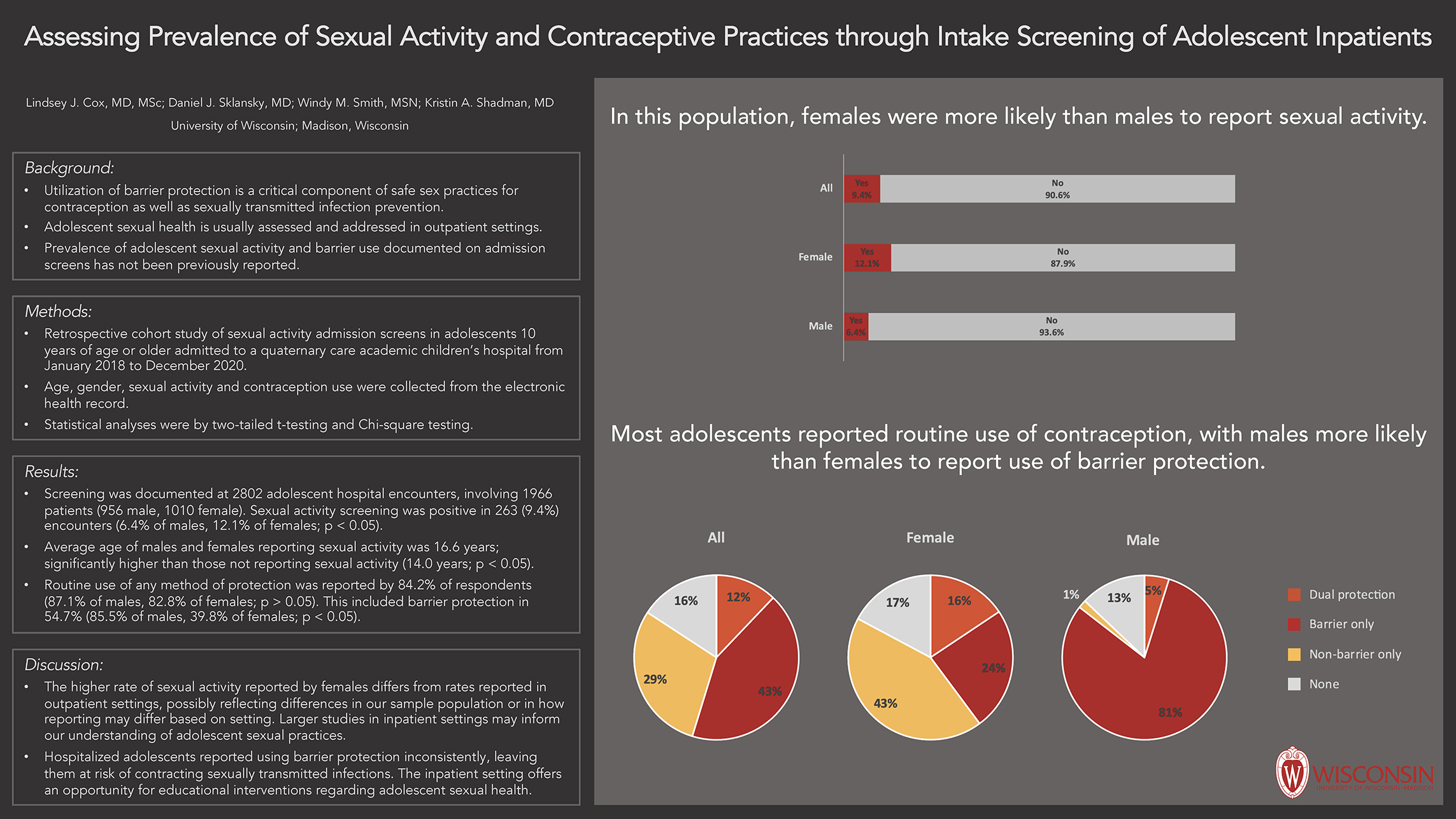
Click here for .pdf version of poster
Title: Assessing Prevalence of Sexual Activity and Contraceptive Practices Through Intake Screening of Adolescent Inpatients
Cox L, Sklansky D, Smith W, Shadman K
Background: Prevalence of adolescent sexual activity and contraception use is usually assessed in outpatient settings. Hospitalization provides an opportunity to screen adolescents for sexual practices; however, prevalence of sexual activity and barrier use documented on admission screens has not been previously reported.
Design/Methods: Assess the prevalence of reported sexual activity and use of barrier protection in hospitalized adolescents. This is a retrospective cohort study of all hospital admissions with completed sexual activity screens in adolescents 10 years of age or older admitted to a quaternary care academic children’s hospital from January 2018 to December 2020. Age, gender, sexual activity and contraception use were collected from the electronic health record. Gender differences in reported sexual activity and use of barrier protection were analyzed by Chi-square testing. Age differences in reported sexual activity were analyzed by two-tailed t-testing.
Results: Screening was documented at 2802 adolescent hospital encounters, involving 1966 patients (956 male, 1010 female). Sexual activity screening was positive in 263 (9.4%) of encounters, with females more likely than males to report sexual activity (12.1 vs 6.4%; p < 0.05). Average age of males and females reporting sexual activity was 16.6 years, which was significantly higher than those not reporting sexual activity (14.0 years; p < 0.05). Contraceptive use was noted in 190 (72%) encounters. Of those, 84.2% reported using at least one mode of contraception routinely (87.1% of males, 82.8% of females). While 54.7% reported consistent use of condoms, a gender difference was observed with 85.5% of males and 39.8% of females (p < 0.05) reporting condom use.
Conclusions: Hospitalized adolescents reporting sexual activity used barrier protection inconsistently, leaving them at risk of contracting sexually transmitted infections. The inpatient setting offers an opportunity for educational interventions regarding sexual health that should be explored. The higher rate of sexual activity reported by hospitalized females contrasts with rates reported in other settings, possibly reflecting differences in our sample population or in how hospitalized adolescents respond to sexual health questions. Larger studies of sexual activity reporting in inpatient settings may inform our understanding of adolescent sexual practices and how reporting may differ based on setting.
“Those That Fail to Learn from the Past are Doomed to Repeat It”: Characterization of Central Line Associated Bloodstream Infections (CLABSIS) at American Family Children’s Hospital (AFCH) from 2018-2020
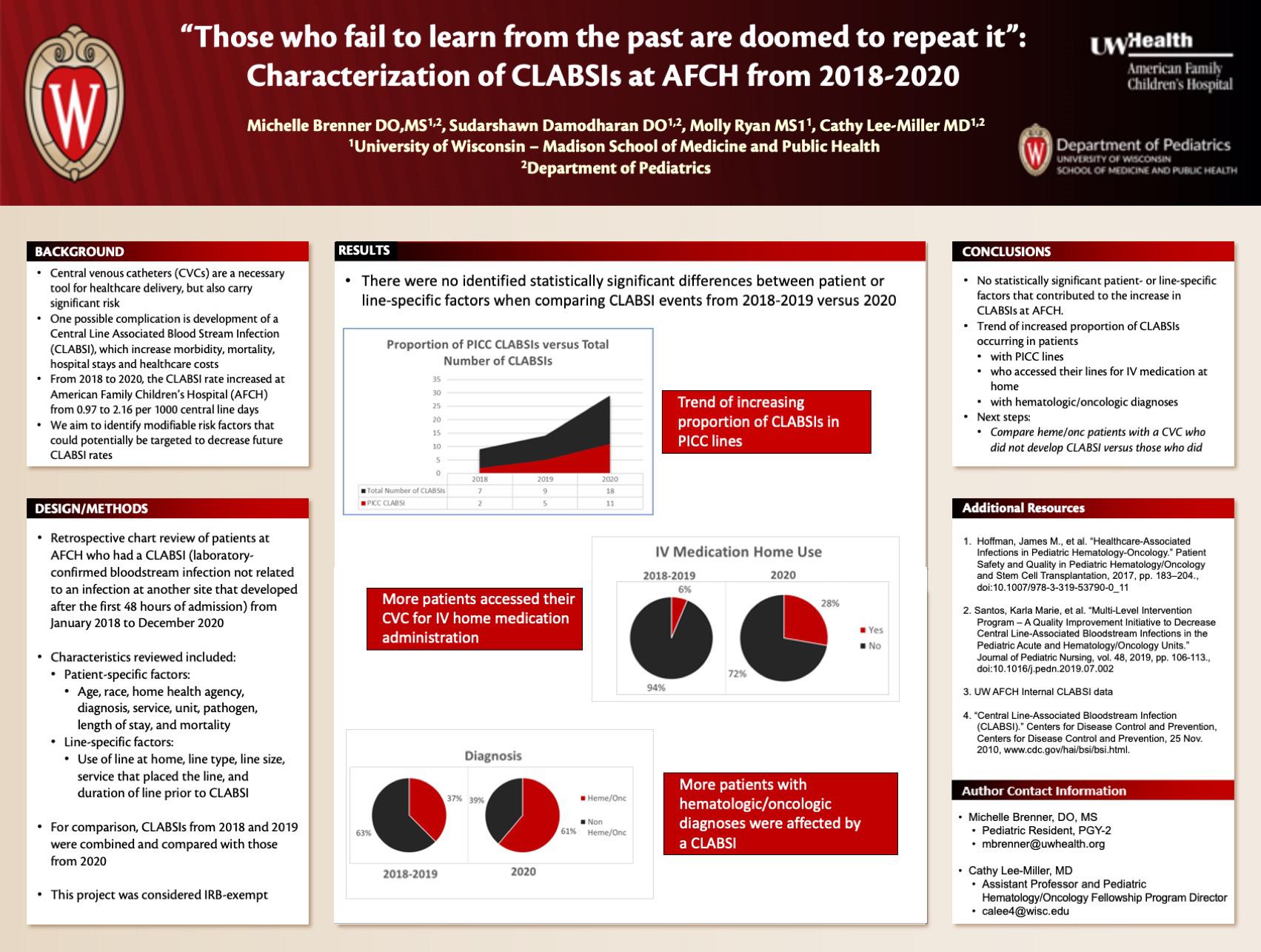
Click here for .pdf version of poster
Title: “Those That Fail to Learn from the Past are Doomed to Repeat It”: Characterization of Central Line Associated Bloodstream Infections (CLABSIS) at American Family Children’s Hospital (AFCH) from 2018-2020
Brenner M, Damodharan S, Ryan M, Lee-Miller C
Background: Central venous catheters (CVCs) are a necessary tool for healthcare delivery, but they also carry significant infectious risk, particularly the development of CLABSIs. Aside from associated morbidity and mortality, CLABSIs lengthen hospital stays and increase healthcare costs. From 2018 to 2020, the annual CLABSI rate has drastically increased at AFCH from 0.97 to 2.16 per 1000 central line days. We aim to identify modifiable risk factors that have changed over this interval that could potentially be targeted for process improvement efforts to decrease future CLABSI rates.
Design/Methods: Retrospective chart review of pediatric patients at AFCH who had a CLABSI (laboratory-confirmed bloodstream infection not related to an infection at another site that developed after the first 48 hours of admission) from January 2018 to December 2020. Characteristics reviewed included patient-specific factors (age, race, home health agency, diagnosis, service, unit, pathogen, length of stay, and mortality) and line-specific factors (use of line at home, line type, line size, service that placed the line, and duration of line prior to CLABSI). For comparison, CLABSIs from 2018 and 2019 were combined and compared with 2020. This project was considered IRB-exempt.
Results: There were no identified statistically significant differences between patient or line-specific factors when comparing CLABSI events from 2018–2019 versus 2020. A trend for increasing proportion of CLABSIs in PICC lines occurred with 2/7, 5/9, and 11/18 in each year, respectively. When comparing 2018–2019 versus 2020, more patients accessed their CVC for IV home medication administration (5/18 in 2020 versus 1/16 previously) and more patients with hematologic/oncologic diagnoses were affected by a CLABSI (11/18 in 2020 versus 6/16).
Conclusions: While there were no statistically significant patient or line-specific factors that contributed to the increase in CLABSIs at AFCH, there was a trend of increased proportion of CLABSIs occurring in patients with PICC lines, those who accessed their lines for IV medication at home, and patients with hematologic/oncologic diagnoses. This characterization lays the groundwork for further research comparing patients with a CVC who did not develop CLABSI versus those who did, specifically in patients with underlying hematologic/oncologic disorders.
Pediatric Resident Knowledge About the Push-Pull Method for Rapid Intravenous Fluid Administration
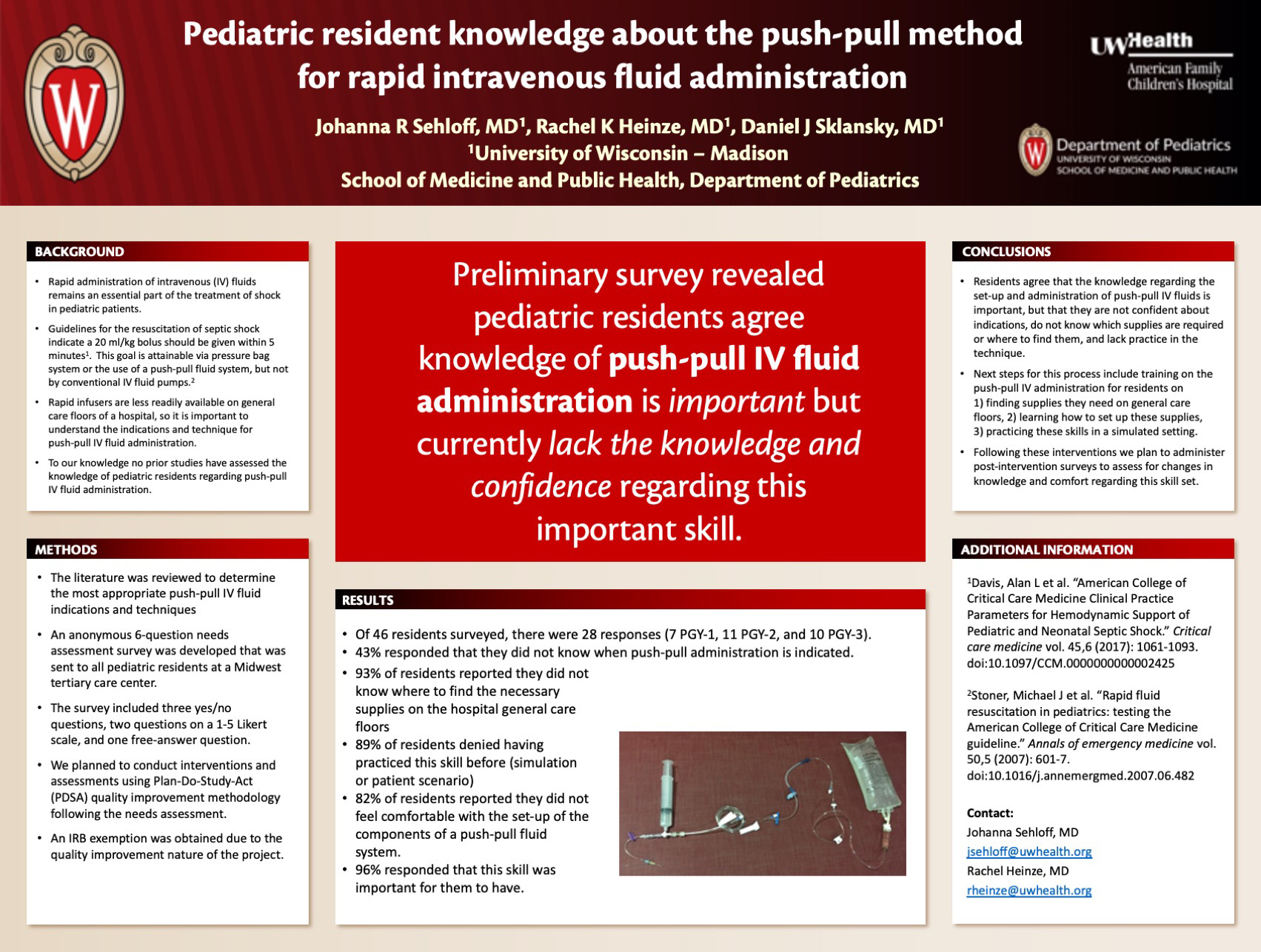
Click here for .pdf version of poster
Title: Pediatric Resident Knowledge About the Push-Pull Method for Rapid Intravenous Fluid Administration
Sehloff J, Heinze R, Sklansky D
Background: Rapid administration of intravenous (IV) fluids remains an essential part of the treatment of shock in pediatric patients. The American College of Critical Care Medicine guidelines for the resuscitation of septic shock indicate a 20 ml/kg bolus should be given within 5 minutes.1 A recent prospective study found that this goal was attainable via pressure bag system or the use of a push-pull fluid system, but not by conventional IV fluid pumps. 2 Given that rapid infusers are less readily available on the general care floors of a hospital, it is important for providers to understand the indications and technique for push-pull IV fluid administration. To our knowledge no prior studies have assessed the knowledge of pediatric residents regarding push-pull IV fluid administration.
Design/Methods: After reviewing the literature to determine the most appropriate push-pull IV fluid indications and techniques, we developed an anonymous 6-question needs assessment survey that was sent to all pediatric residents at a Midwest tertiary care center. The survey included three yes/no questions, two questions on a 1-5 Likert scale, and one free-answer question. We planned to conduct interventions and assessments using Plan-Do-Study-Act (PDSA) quality improvement methodology following the needs assessment. An IRB exemption was obtained due to the quality improvement nature of the project.
Results: Of 46 residents surveyed, there were 28 responses (7 PGY-1, 11 PGY-2, and 10 PGY-3). Survey results revealed a lack of knowledge of indications for the administration push-pull fluids with 43% responding that they did not know when such administration is indicated. In addition, 93% of residents reported they did not know where to find the necessary supplies on the hospital general care floors, 89% of residents denied having practiced this skill before, and 82% of residents reported they did not feel comfortable with the set-up of the components of a push-pull fluid system. A large majority (96%) responded that this skill was important for them to have.
Conclusions: Residents agree that the knowledge regarding the set-up and administration of push-pull IV fluids is important, but that they are not confident about indications, do not know which supplies are required or where to find them, and lack practice in the technique. Next steps for this process include training on the push-pull IV administration for residents on 1) finding supplies they need on general care floors, 2) learning how to set up these supplies, 3) practicing these skills in a simulated setting. Following these interventions, we plan to administer post-intervention surveys to assess for changes in knowledge and comfort regarding this important skill set.
Session E: Patient Experience
Moderator: Emily Ruedinger, MD
6 minutes each, 14 presenters
3:30-5:00
| Time | Presenter | Title |
|---|---|---|
| 3:30-3:36 | Henry Zapata Galarza, MD | Predictors of Adverse Neurodevelopmental outcomes in extremely premature infants (<27 weeks) |
| 3:36-3:42 | Brandon Tomlin, MD | Oxygen Saturation Profiles in Healthy Term Neonates |
| 3:42-3:48 | Paige Selenski | Pediatric COVID-19 in Hospitalized Children |
| 3:48-3:54 | Paige Condit, MD | Searching for Risk Factors Associated with the development of pulmonary hypertension in extremely premature infants |
| 3:54-4:00 | Sima Ramratnam, MD | Relationship of Rhinitis and Respiratory Allergy and Asthma Phenotypes in an Urban Birth Cohort |
| 4:00-4:06 | Arij Beshish, MD | Outpatient IV Sotalol Load Used to Replace Oral Sotalol Hospital Admission |
| 4:06-4:12 | Melissa Villegas, MD | Comparison of Early Diagnosis of Cerebral Palsy in the High-Risk Neonatal Population |
| 4:12-4:18 | Tim Livett, MD | Pediatric Diabetes Mellitus in the Time of COVID-19 |
| 4:18-4:24 | Zachary Weber, MD | Characteristics of Pediatric Emergency Department Patients with Suspected Arrhythmias |
| 4:24-4:30 | Megan Williams, MD | Adverse Outcomes Associated with Enteral Nutrition In Children with Bronchiolitis Admitted to the PICU and Requiring Non-Invasive Ventilation |
| 4:30-4:36 | Annie Uhing, MD | Progressive shortness of breath and hypoxia in an adolescent female athlete: A case report |
| 4:36-4:43 | Aisha Ansar, MD
Jon Fliegel, MD |
The one with confusion: Tics? Toxic? COVID? |
| 4:43-4:49 | Paige Selenski | Assessing the Risk of Hypovitaminosis and Vitamin C Deficiency in Critically Ill Pediatric Patients Undergoing Cardiopulmonary Bypass |
| 4:49-4:55 | Lauren Kacvinksy, MD | Palliative Care in a Pediatric Oncology Population |
| 4:55-5:00 | Wrap-Up |
This is an accordion element with a series of buttons that open and close related content panels.
Predictors of Adverse Neurodevelopmental Outcomes in Extremely Premature Infants (<27 Weeks)
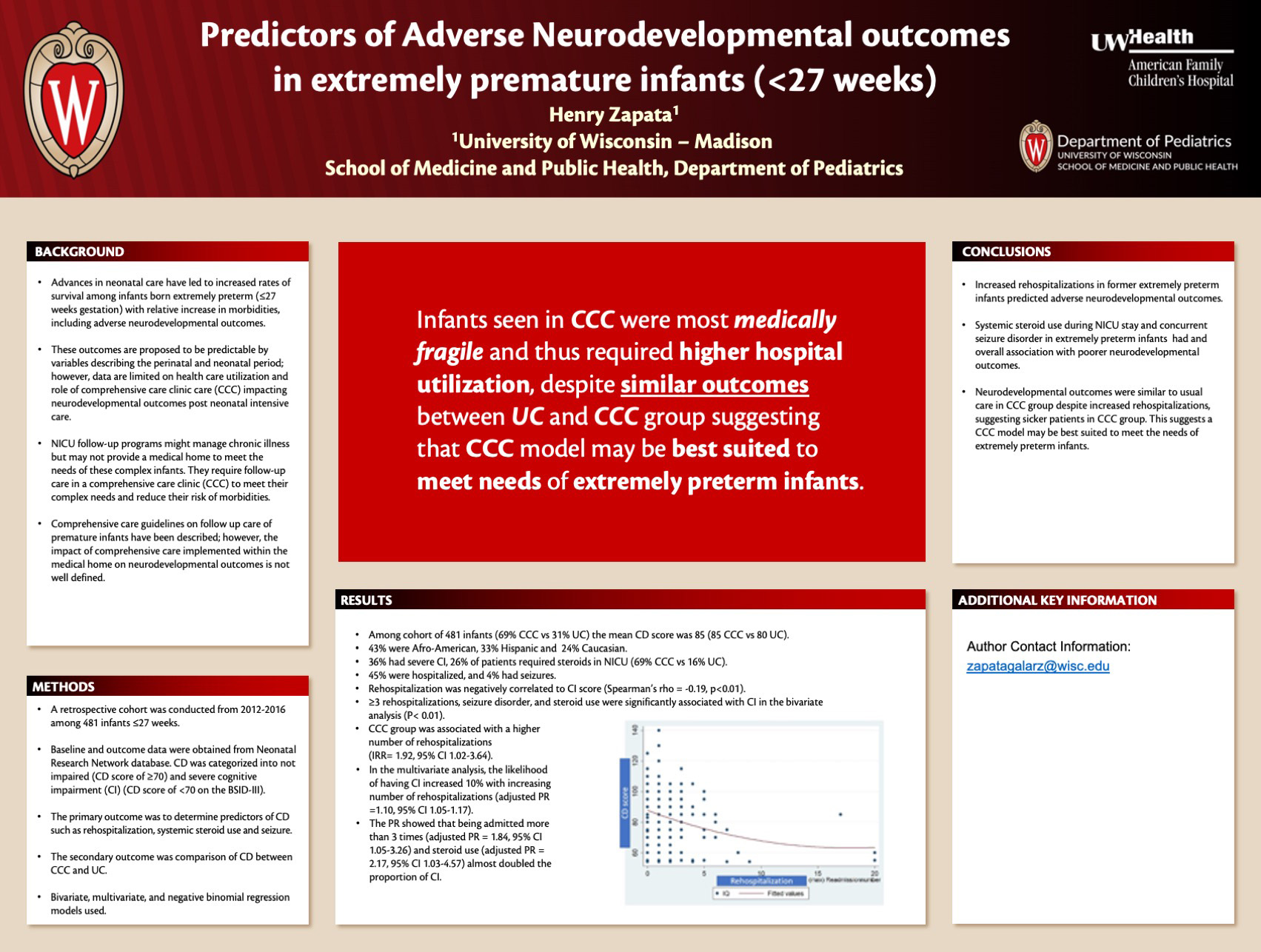
Click here for .pdf version of poster
Title: Predictors of Adverse Neurodevelopmental Outcomes in Extremely Premature Infants (<27 Weeks)
Zapata Galarza H
Background: Advances in neonatal care have led to increased rates of survival among infants born extremely preterm (≤27 weeks gestation) with relative increase in morbidities, including adverse neurodevelopmental outcomes. These outcomes are proposed to be predictable by variables describing the perinatal and neonatal period; however, data are limited on health care utilization and role of comprehensive care clinic care (CCC) impacting neurodevelopmental outcomes post neonatal intensive care.
Design/Methods: Assessment of risk predictors for adverse neurodevelopmental outcome, including rehospitalization at 2 years of age in ≤27 weeks infants and comparison of cognitive development (CD) in patients enrolled in CCC vs usual care (UC). A prospective cohort was conducted from 2012-2016 among 481 infants ≤27 weeks. Data was obtained from Neonatal Research Network database. CD was categorized into not impaired (CD score of ≥70) and severe cognitive impairment (CI) (CD score of <70 on the BSID-III). The primary outcome was to determine predictors of CD such as rehospitalization, systemic steroid use and seizure. The secondary outcome was comparison of CD between CCC and UC. Bivariate, multivariate, and negative binomial regression models used.
Results: Among cohort of 481 infants (69%CCC vs 31% UC) the mean CD score was 85 (85 CCC vs 80 UC). 36% had severe CI, 26% of patients required steroids in NICU (69% CCC vs 16% UC), 45% were hospitalized, and 4% had seizures. Rehospitalization was negatively correlated to CI score (Spearman’s rho = -0.19, p<0.01). ≥3 rehospitalizations, seizure disorder, and steroid use were significantly associated with CI (P< 0.01). CCC group was associated with a higher number of rehospitalizations (IRR= 1.92, 95% CI 1.02-3.64). In the multivariate analysis, the likelihood of having CI increased 10% with increasing number of rehospitalizations (adjusted PR =1.10, 95% CI 1.05-1.17). ≥3 rehospitalizations (adjusted PR = 1.84, 95% CI 1.05-3.26) and steroid use (adjusted PR = 2.17, 95% CI 1.03-4.57) almost doubled the proportion of CI.
Conclusions: Increased rehospitalizations, steroid use, and seizure disorder in extremely preterm infants predicted adverse neurodevelopmental outcomes. Neurodevelopmental outcomes were similar to usual care in CCC group despite increased rehospitalizations, suggesting sicker patients in CCC group. This suggests a CCC model may be best suited to meet the needs of extremely preterm infants.
Oxygen Saturation Profiles in Healthy Term Neonates
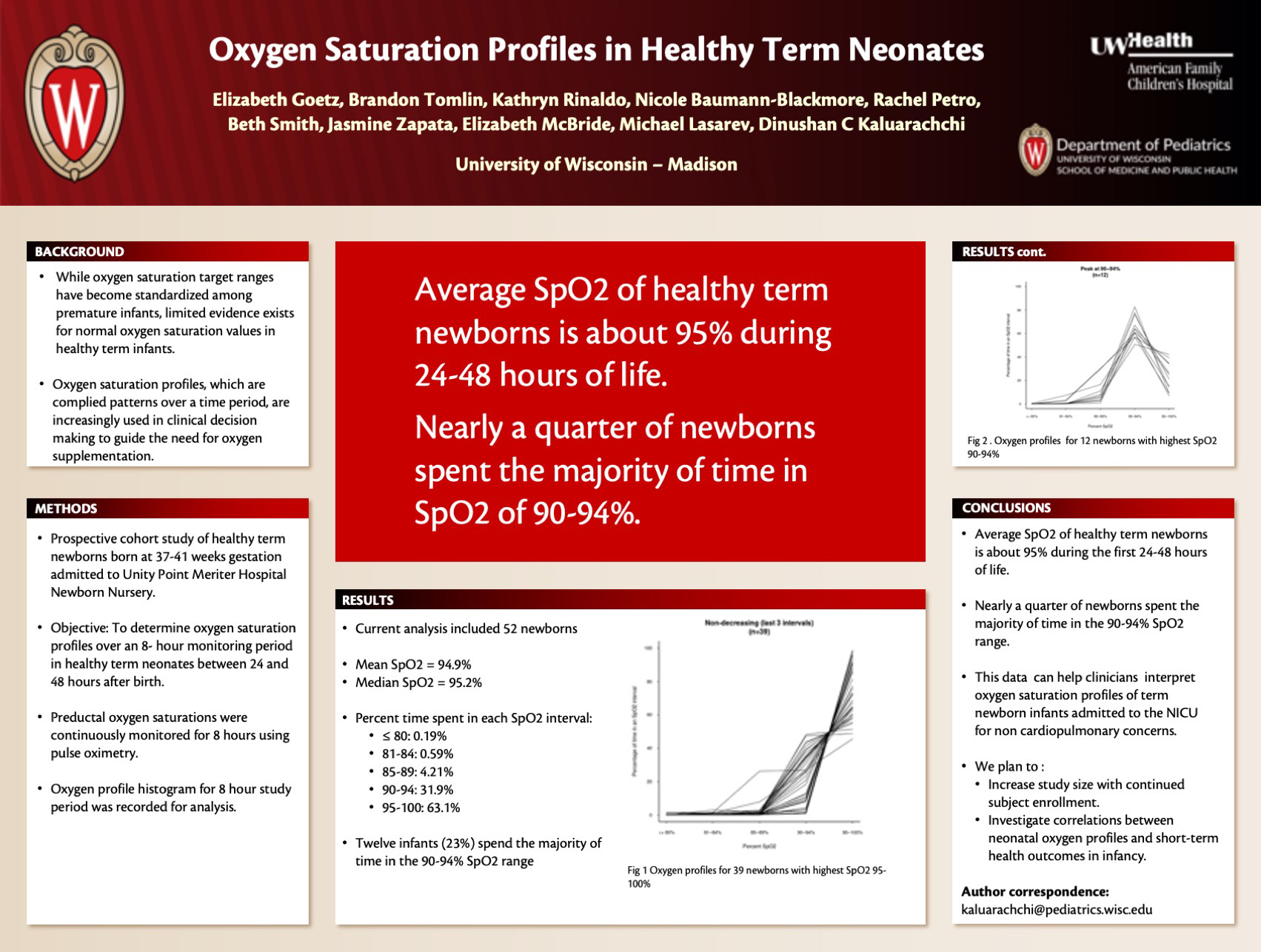
Click here for .pdf version of poster
Title: Oxygen Saturation Profiles in Healthy Term Neonates
Goetz E, Tomlin B, Rinaldo, K, Baumann-Blackmore N, Petro R, Smith B, Zapata J, McBride E, Lasarev M, Kaluarachchi D
Background: Continuous oxygen saturation monitoring using pulse oximetry is routinely used in the neonatal intensive care units (NICU). Oxygen saturation profiles generated by pulse oximetry are commonly used to make management decisions on respiratory support and oxygen supplementation in preterm infants. Oxygen saturation profile data in term infants admitted to NICU are also being increasingly used in clinical decision making. However, there’s only limited evidence on normal oxygen saturation profile values in term infants.
Design/Methods: Objective was to Determine oxygen saturation profile over an 8-hour monitoring period among healthy term neonates between 24 to 48 hours after birth. This is a prospective cohort study of healthy term newborns >24 hours of age born at 37-41 weeks of gestation admitted to University of Wisconsin newborn nursery hospitalist service at Unity Point Meriter Hospital. Preductal oxygen saturations were continuously monitored for an eight-hour period using pulse oximetry in study subjects between 24 and 48 hours of life. At completion of 8 hours, the recording was downloaded to a computer. Periods where pulse waveform was disturbed were excluded. Oxygen profile histogram for 8-hour study period was be recorded for analysis. Average percent oxygen saturation (SpO2) was measured over the entire study duration for each neonate and was also described as the fraction of the entire study duration a neonate’s SpO2 reading was in each of five intervals: ≤ 80%, 81–84%, 85–89%, 90–94%, and 95–100%.
Results: Fifty-two newborns were included in the current analysis of this ongoing study. Mean gestational age and mean birth weight were 39.5 weeks and 3478g respectively. Pulse oximetry was started at mean age of 28 hours and continued for mean duration of 514 minutes. Mean and median SpO2 was 94.9% and 95.2% respectively. Percent time spent on each of the five SpO2 intervals are as follows, <= 80; 0.19%, 81-84; 0.59%, 85-89; 4.21%, 90-94; 31.9%, 95-100; 63.1%. Twelve infants (23%) had majority of SpO2 in 90-94%. Female gender and lower maternal age were modestly associated with odds of having highest SpO2 between 95–100%. None of the other study variables such as gestational age, birth weight, race, delivery mode was associated with odds of having highest SpO2 between 95–100%.
Conclusions: Interim analysis of this ongoing study showed that mean SpO2 of healthy term newborns is about 95% during 24-48 hours of life. Nearly quarter of newborns spent majority of time in SpO2 of 90-94%. This is data is important when interpreting oxygen saturation profiles of term newborn infants admitted to the NICU for non-cardio-respiratory concerns.
Pediatric COVID-19 in Hospitalized Children
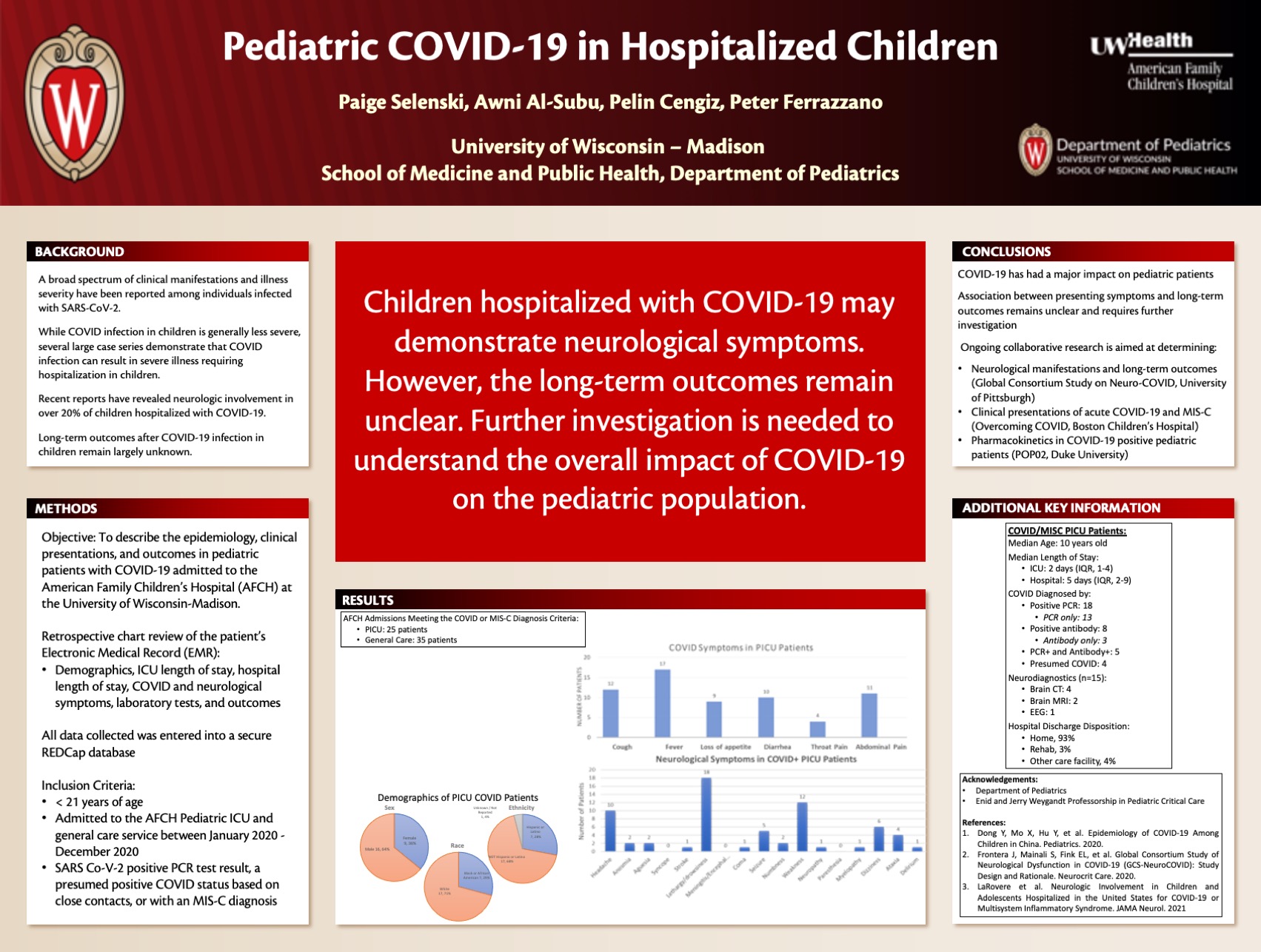
Click here for .pdf version of poster
Title: Pediatric COVID-19 in Hospitalized Children
Selenski P, Al-Subu A, Cengiz P, Ferrazzano P
Background: As the COVID-19 pandemic has evolved worldwide, a broad spectrum of clinical manifestations has been described among different age groups infected with SARS-CoV-2. Given the lower incidence in, children, data in the pediatric population is limited, leaving the short-term and long-term outcomes related to COVID-19 largely unknown. Recent reports have revealed neurologic involvement in over 20% of children hospitalized with COVID. The full impact of COVID-19 in children remains unclear, warranting collaborative data sharing that captures the entirety of a patient’s hospital course and beyond. This collaborative data is critical to understanding the manifestations and overall impact of COVID-19 on the pediatric population.
Design/Methods: The primary objective of this retrospective study was to describe the epidemiology, clinical presentations, and outcomes in pediatric patients with COVID-19 admitted to the American Family Children’s Hospital at the University of Wisconsin-Madison. Pediatric patients (< 21 years of age) admitted to the Pediatric ICU and ward between January 2020 -December 2020 and with a SARS Co-V-2 positive PCR test result, a presumed positive COVID status based on close contacts, or with an MIS-C diagnosis were reviewed using the Electronic Medical Record (EMR). Data collection was conducted on factors related to demographics, ICU length of stay, hospital length of stay, COVID and neurological symptoms, laboratory tests, and outcomes. All data was entered into a secure REDCap database.
Results: A total of 25 patients were admitted to the PICU, and 35 patients were admitted to general care, meeting the COVID-19 or MIS-C diagnosis criteria. Among patients admitted to the PICU, the median age was 10 years old. The mean ICU length of stay was 4 (1-18) days, and the mean hospital length of stay was 12.1 (2-99) days. The primary admitting problem included acute COVID-19 in 4 patients, MIS-C in 6 patients, and other diagnoses unrelated to COVID-19 (incidental finding) in 15 patients.
Conclusions: COVID-19 has had a major impact on pediatric patients. The association between presenting symptoms and long-term outcomes remains unclear and requires further investigation. Ongoing research is aimed at determining neurological manifestations and long-term outcomes (Global Consortium Study on Neuro-COVID, University of Pittsburgh), clinical presentations of acute COVID-19 and MIS-C (Overcoming COVID, Boston Children’s Hospital), and pharmacokinetics in COVID-19 positive pediatric patients (POP02, Duke University).
Searching for Risk Factors Associated with the Development of Pulmonary Hypertension in Extremely Premature Infants
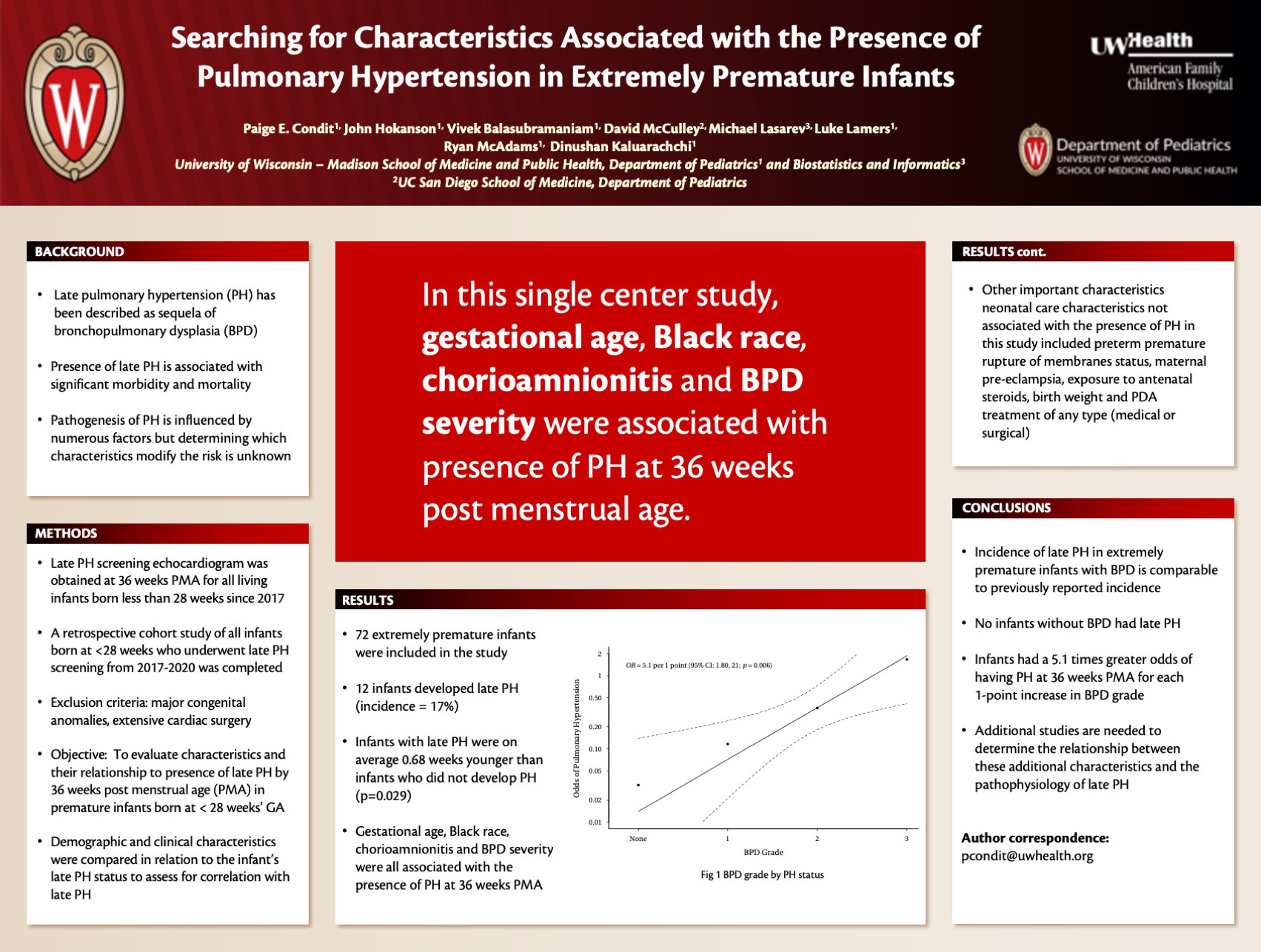
Click here for .pdf version of poster
Title: Searching for Risk Factors Associated with the Development of Pulmonary Hypertension in Extremely Premature Infants
Condit PE, Hokanson J, McCulley D, Balasubramaniam V, Lasarev M, Lamers L, McAdams R, Kaluarachchi D
Background: Late pulmonary hypertension (PH) is a well described as sequela of bronchopulmonary dysplasia (BPD) in extremely premature infants born at < 28 weeks gestational age (GA) and is associated with significant morbidity and mortality. The pathogenesis of PH is influenced by numerous factors but determining which factors modify the risk is unknown. The purpose of this study is to evaluate risk factors and their relationship to development of late PH by 36 weeks post menstrual age (PMA) in premature infants born at < 28 weeks’ GA.
Design/Methods: A late PH screening echocardiogram was obtained at 36 weeks PMA for all surviving extremely preterm infants admitted to a Midwest neonatal intensive care unit since January of 2017. A retrospective chart review of all extremely preterm infants who underwent late PH screening was completed. Infants with major congenital anomalies, and those undergoing extensive cardiac surgery were excluded. Demographic and clinical characteristics were compared in relation to the infant’s late PH status to assess for correlation with late PH development.
Results: Out of 83 extremely preterm infants admitted, 72 (average GA = 25.2 weeks) were included. 12 infants developed late PH (incidence = 17%). Average age of infants who developed late PH was 0.68 weeks less than those without late PH (p=0.029). Race was also significantly different between groups; 58% of infants with late PH were Black whereas 58% of infants without late PH were White (p <0.001). Infants with late PH were more likely to have been born to mothers with chorioamnionitis (p=0.005) and more likely to require a higher fractional inspired oxygen concentration (FiO2) at 4 weeks of life (p=0.02). Likewise, no infants with late PH were in room air without respiratory support at 36 weeks PMA (p=0.005). A strong association was found among the grade of BPD and late PH such that odds of late PH increased 5.1 times per each additional 1-point gain in BPD grade (p=0.01).
Conclusions: Based on this study, ~1 in 6 (17%) extremely premature infants with BPD develop PH, a finding similar to previous reports (14%). Characteristics associated with development of PH at 36 weeks PMA, include gestational age, Black race, chorioamnionitis, and BPD severity. In contrast to previous reports, none of the infants without BPD developed PH. Further studies are needed to determine how these potential risk factors may contribute to the pathogenesis of PH.
Relationship of Rhinitis and Respiratory Allergy and Asthma Phenotypes in an Urban Birth Cohort
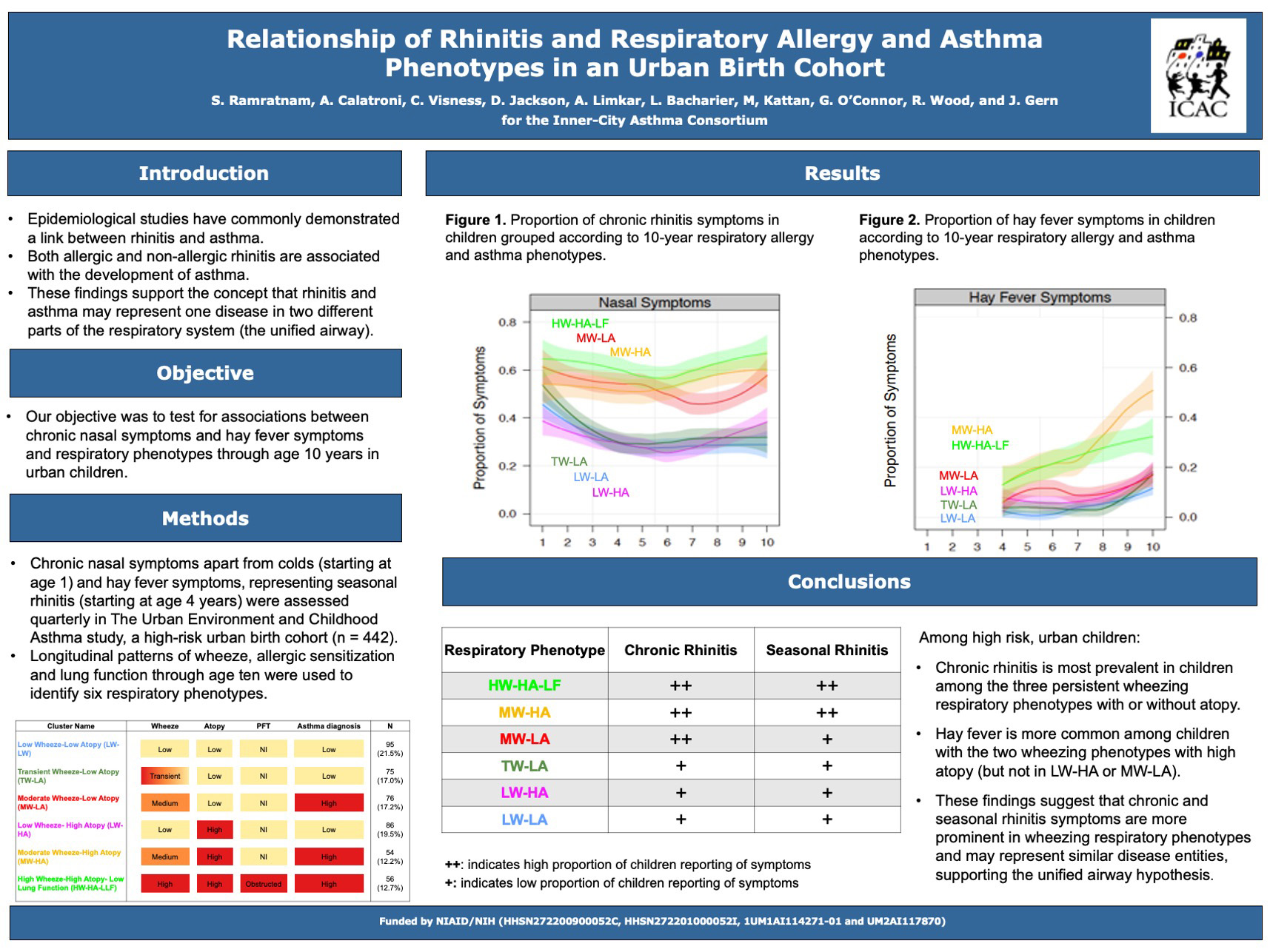
Click here for .pdf version of poster
Title: Relationship of Rhinitis and Respiratory Allergy and Asthma Phenotypes in an Urban Birth Cohort
Ramratnam S, Calatroni A, Bacharier L, Kattan M, O’Connor G, Wood R, Visness C, Jackson DJ, Gern JE
Background: Our objective was to test for associations between rhinitis symptoms and respiratory phenotypes through age 10 years in urban children.
Design/Methods: Chronic nasal symptoms (starting at age 1) and seasonal rhinitis symptoms (starting at age 4 years) were assessed yearly in The Urban Environment and Childhood Asthma study, a high-risk urban birth cohort (n=442). Longitudinal patterns of wheeze, allergic sensitization and lung function through age ten were used to identify six respiratory phenotypes: 1) low wheeze, low atopy (“LW-LA”); 2) transient wheeze, low atopy (“TW-LA”); 3) moderate wheeze, low atopy (“MW-LA”); 4) low wheeze, high atopy (“LW-HA”); 5) moderate wheeze, high atopy (“MW-HA”); 6) high wheeze, high atopy, low lung function (“HW-HA-LF”). Differences in chronic and seasonal rhinitis symptoms among phenotypes were examined using longitudinal data analyses.
Results: Rhinitis in the first year was common in all groups, but nasal symptoms differentially associated with wheeze and atopy thereafter. Chronic rhinitis symptoms were more prevalent in the three wheezing phenotypes (HW-HA-LF, MW-LA, and MW-HA) compared to the transient wheeze and low wheeze groups (~75% increase in symptoms over the first 10 years, p<0.001). Seasonal rhinitis symptoms were most prevalent (>2-fold increase) in the two high-atopy groups with wheeze (MW-HA and HW-HA-LF, p<0.001).
Conclusions: Among high risk, urban children, chronic rhinitis is most prevalent in children among the three persistent wheezing respiratory phenotypes, while seasonal rhinitis is most prevalent in children among the high atopy respiratory phenotypes with wheezing. These close relationships between trajectories of wheeze and rhinitis in early life suggest shared pathogenic mechanisms.
Outpatient IV Sotalol Load Used to Replace Oral Sotalol Hospital Admission
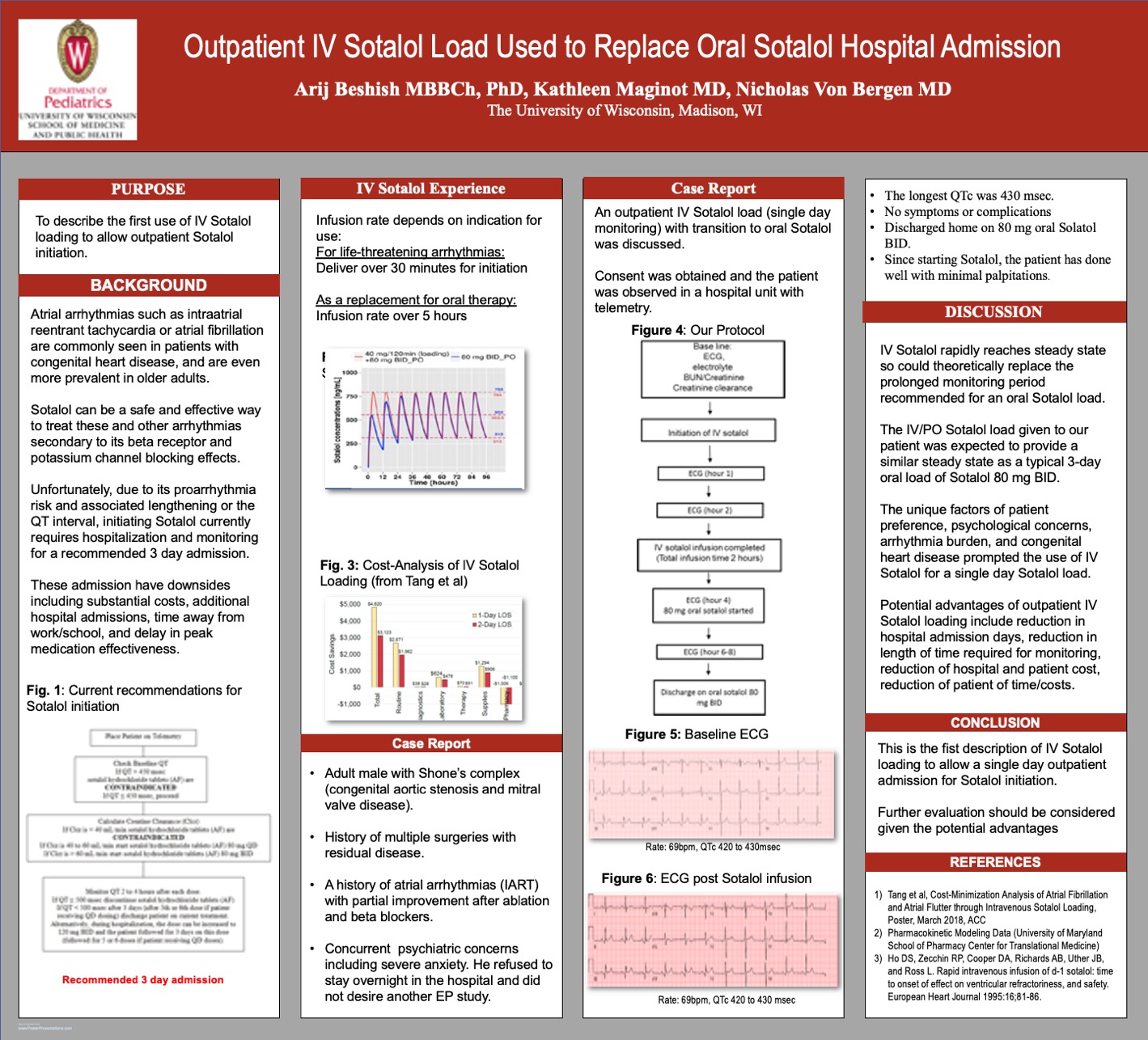
Click here for .pdf version of poster
Title: Outpatient IV Sotalol Load Used to Replace Oral Sotalol Hospital Admission
Beshih AG, Maginot KM, Von Bergen NH
Case Report: A 33-year-old male with a history of congenital aortic stenosis status post multiple palliations including valvuloplasty, Ross procedure and Bentall with a mitral valve repair and with residual pulmonary, aortic and mitral valve disease had a history of atrial arrhythmias. He also had concurrent psychiatric concerns including anxiety and concerns of overnight hospitalization. He had undergone an Electrophysiology study with ablation of multiple arrhythmia circuits of intra-atrial reentrant tachycardia (IART) in 2016 with some improvement of symptoms. However, he continued to have short salvo’s of atrial arrhythmias suggestive of IART. A repeat EP study or medication adjustments were discussed. However, in part due to underlying psychiatric concerns, the patient was reluctant to undergo any procedures, and refused overnight admission. This prompted us to consider discontinuing Carvediolol and attempting an IV Sotalol load before transition to oral Sotalol to allow a single daytime admission. The patient was admitted in the morning to a unit with telemetry. Consent was obtained from the patient. Baseline vitals were taken and peripheral IV was put in place, electrolyte, BUN/Cr were obtained and were normal with a normal Cr clearance. A baseline EKG showed a QTc which was within normal range (~400msec). Based on mathematical modeling of a steady state, 40 mg Sotalol was administered IV over 2 hours. The telemetry was set to alarm if there was a significant lengthening of the QTC. In addition, an ECG was performed every hour throughout infusion and was repeated at 2 hours post infusion with a decision to stop the infusion if the QTc increased above 500msec. After 2 hours an 80 mg oral Sotalol was started and ECG was evaluated at 2 and 4 hours after ingestion. This is expected to provide a similar steady state to the full 3-day admission at 80mg PO BID. The ECGs continued to show a QTc that was only slightly prolonged (longest ~430msec). He was discharged home on 80 mg oral Solatol and carvedilol was discontinued. The transition was tolerated well, patient was asymptomatic. Since starting the sotalol patient has done well with minimal palpitations.
Conclusions: Atrial arrhythmias are the most common sustained cardiac arrhythmia in clinical practice. Sotalol may be considered for arrhythmia control but typically requires a 3-day admission. IV Sotalol rapidly reaches a steady state, so could theoretically replace the prolonged monitoring period. The unique factors of patient preference, psychological concerns, arrhythmia burden and congenital heart disease prompted the use of IV Sotalol to allow a single day admission for Sotalol loading. This has the advantage of decreasing the length of hospital admissions, potentially decreasing hospital charges and saving patient time. This first in man case report suggests that this may be considered for other patients.
Comparison of Early Diagnosis of Cerebral Palsy in The High-Risk Neonatal Population
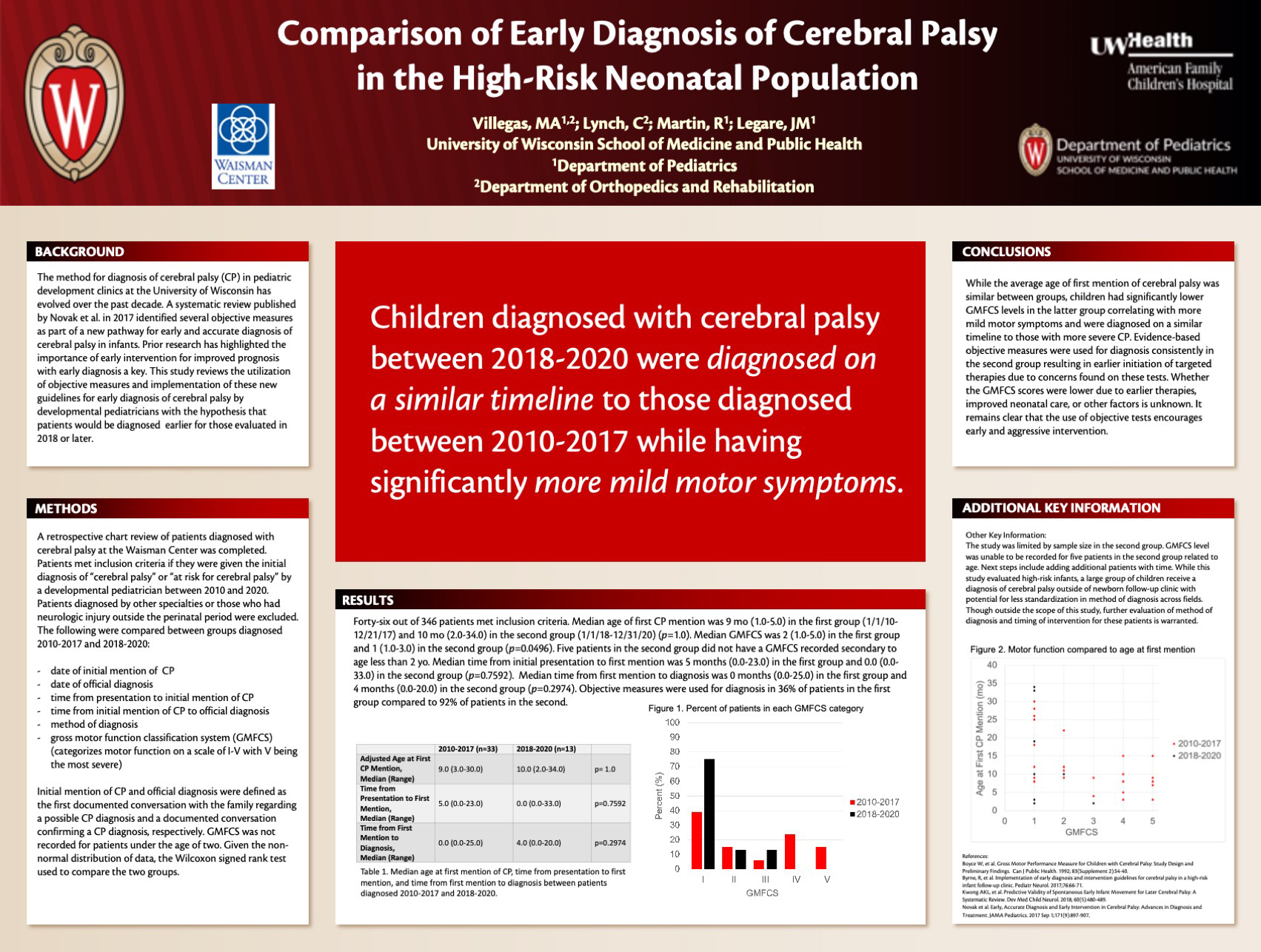
Click here for.pdf version of poster
Title: Comparison of Early Diagnosis of Cerebral Palsy in The High-Risk Neonatal Population
Villegas M, Lynch C, Martin R, Legare J
Background: The method for diagnosis of cerebral palsy (CP) in pediatric development clinics at the University of Wisconsin has evolved over the past decade. A systematic review published by Novak et al. in 2017 identified several objective measures as part of a new pathway for early and accurate diagnosis of CP in infants. Prior research has highlighted the importance of early intervention for improved prognosis with early diagnosis a key. This study reviews the utilization of objective measures and implementation of these new guidelines for early diagnosis of CP by developmental pediatricians with the hypothesis that patients would be diagnosed earlier for those evaluated in 2018 or later.
Design/Methods A retrospective chart review of patients diagnosed with CP at the Waisman Center was completed. Patients met inclusion criteria if they were given the initial diagnosis of “cerebral palsy” or “at risk for cerebral palsy” by a developmental pediatrician between 2010 and 2020. Patients diagnosed by other specialties or who had neurologic injury outside the perinatal period were excluded. Demographics, date of initial mention of CP, date of official diagnosis, timing of therapy initiation, and gross motor function classification system (GMFCS), which ranges between I-V with V being most severe, were compared between groups.
Results: Out of the original 345 charts, a total of 46 patients met inclusion criteria. The average age of first CP mention was 11.7 mo in the first group (1/1/10-12/31/17) and 12.3 mo in the second group (1/1/18-12/31/20), not reaching clinical significance. Average GMFCS was 2.6 in the first group and 1.4 in the second which reached clinical significance. Objective measures were used consistently for diagnosis starting in 2018.
Conclusions: While the average age of first mention of CP was similar between groups, children had significantly lower average GMFCS in the latter group correlating with more mild motor symptoms and were diagnosed on a similar timeline to those with more severe CP. Therapies were initiated earlier due to concerns found on early objective tests. Whether the GMFCS scores were lower due to earlier therapies or improved neonatal care is unknown. It remains clear that the use of objective tests encourages early aggressive intervention.
Pediatric Diabetes Diagnosis in the Time of COVID-19
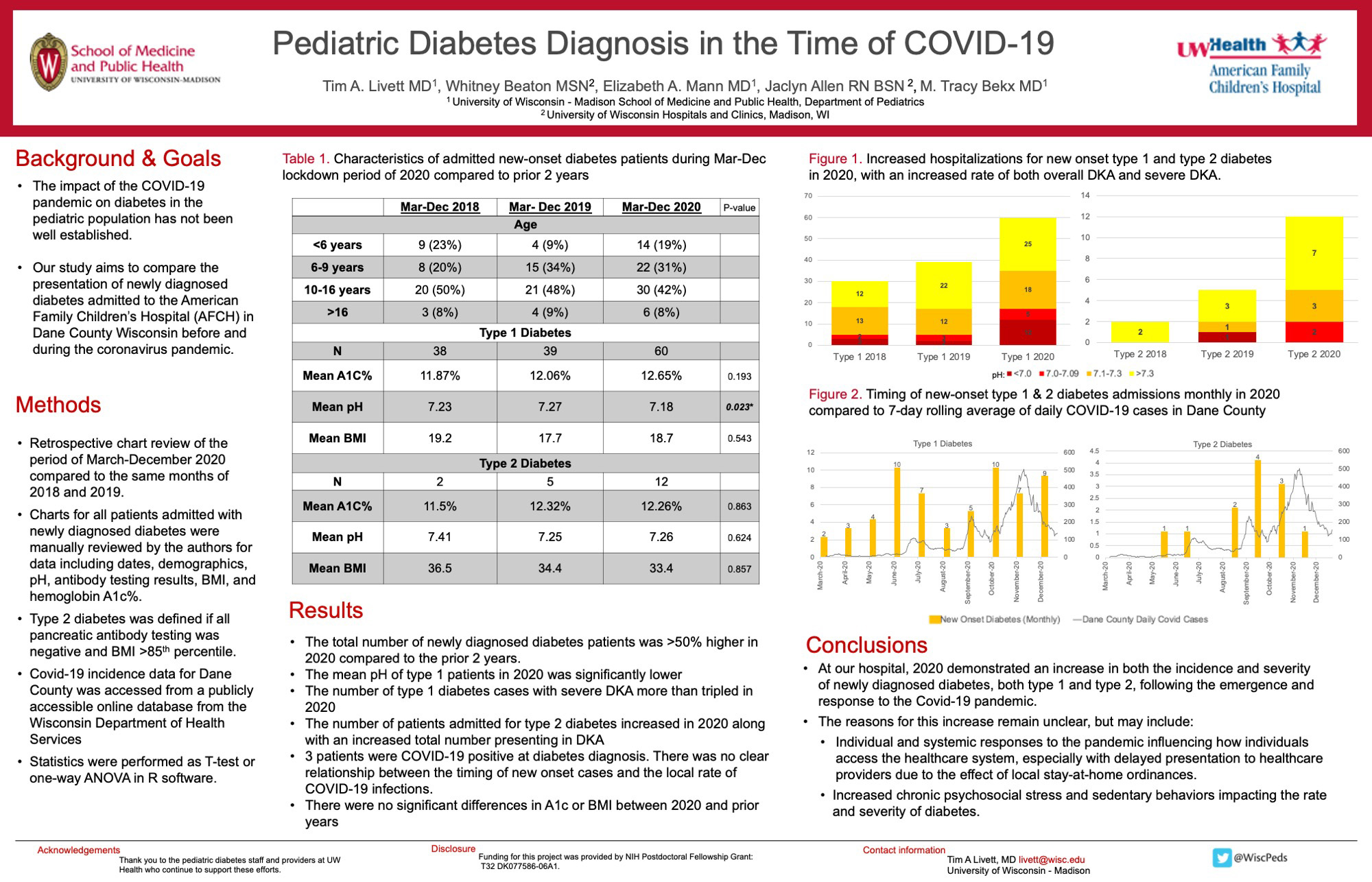
Click here for .pdf version of poster
Title: Pediatric Diabetes Diagnosis in the Time of COVID-19
Livett T, Beaton W, Mann W, Allen J, Bekx T
Background: The impact of the COVID-19 pandemic on the diagnosis and presentation of diabetes in the pediatric population has not been well established. This study aims to compare and characterize the presentation of newly diagnosed diabetes admitted to the American Family Children’s Hospital (AFCH) in Dane County Wisconsin before and during the coronavirus pandemic. A second aim is to compare the numbers of newly diagnosed patients in 2020 to the rate of COVID-19 in Dane County.
Design/Methods: This is a retrospective chart review of all pediatric patients with newly diagnosed diabetes admitted to AFCH in 2018-2020 during the months of March to December. In addition to date of diagnosis, variables assessed included age, body mass index, hemoglobin A1c % and pH at presentation, presence of autoimmune pancreatic antibodies, and COVID-19 PCR testing results at admission. Type 2 diabetes was defined if all pancreatic antibody testing was negative and BMI >85th percentile.
Results: More patients were admitted with newly diagnosed type 1 and type 2 diabetes in the studied months of 2020 compared to 2019 or 2018 (72 total patients in 2020 compared to 40 in 2018 and 44 in 2019). For type 1 diabetes there was a significant decrease in pH at time of diagnosis (average pH decreased by 0.07, p=0.023) and the number with severe DKA (pH <7.1) more than tripled in 2020 compared to 2019 or 2018. A higher fraction of admitted patients were diagnosed with type 2. There was no significant change in body mass index (BMI) or hemoglobin A1c% at the time of diagnosis. 63 patients were tested for COVID-19, with 3 positive results. There was no significant difference in severity in COVID-19 positive patients. There was a surge of type 2 diabetes patients in fall 2020 that did not appear to occur in prior years. Although there have been waves of COVID-19 in the community, it is unclear how this relates to the timing of newly diagnosed diabetes at this time.
Conclusions: There was increases in rate and severity of new onset diabetes during the coronavirus pandemic at our children’s hospital. This has multiple potential contributing factors including delayed presentation to the healthcare system, changes in local specialty referral patterns, decreased access of routine healthcare, the effects of lockdown on psychosocial stress & sedentary activity levels, or effects of the virus itself. Ongoing evaluation of the relationship between the pandemic effects and the rates of diabetes may help to clarify this further.
Characteristics of Pediatric Emergency Department Patients with Suspected Arrhythmias
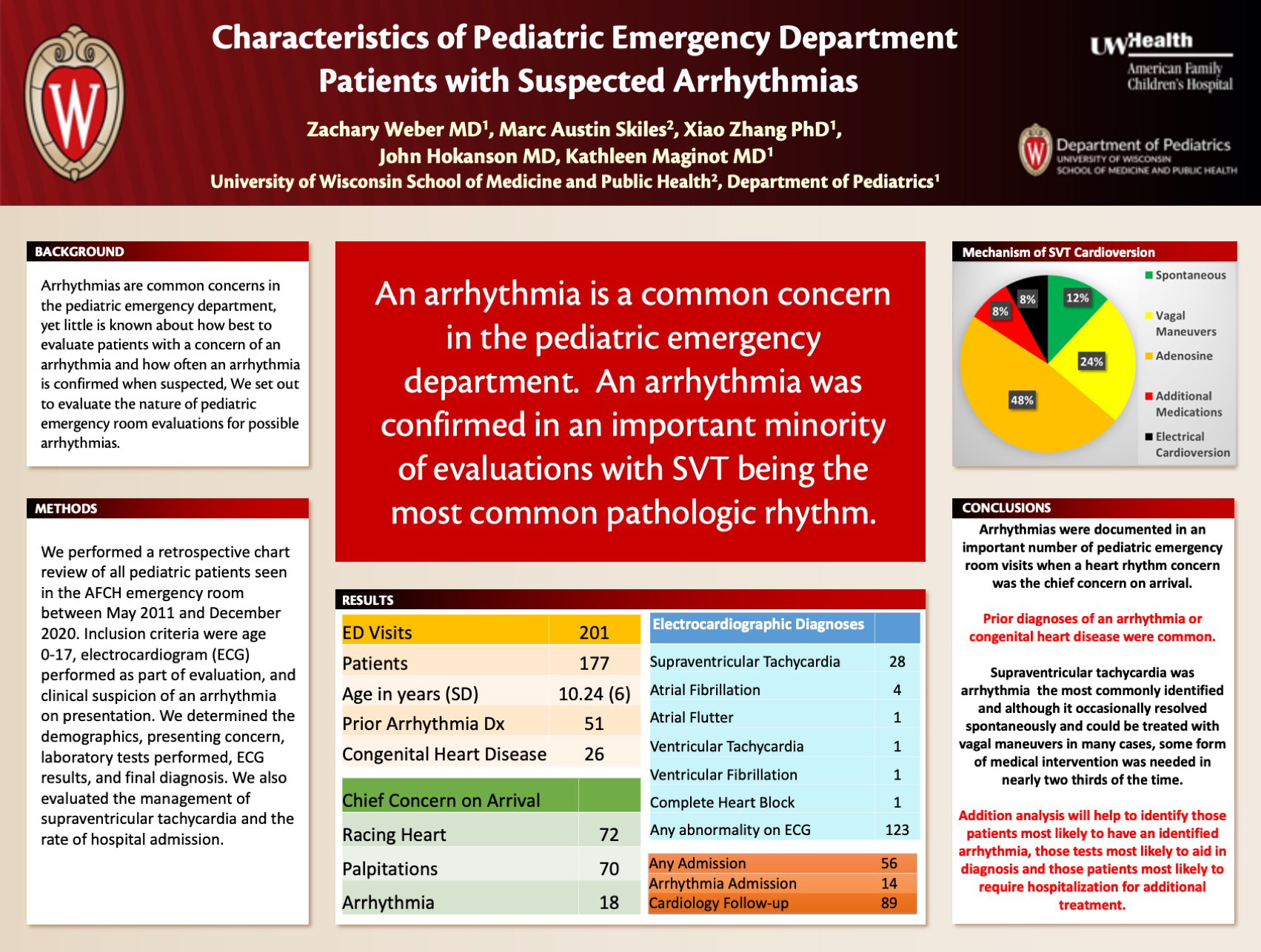
Click here for .pdf version of poster
Title: Characteristics of Pediatric Emergency Department Patients with Suspected Arrhythmias
Weber Z, Skiles M, Hokanson J, Maginot K
Background: Many children are seen for evaluation of their heart rhythm in the emergency department but little is known about the presentation, evaluation, and final diagnoses of these patients.
Design/Methods: A retrospective chart review was conducted on all pediatric patients seen in the AFCH emergency room between May 2011 and December 2020. Inclusion criteria were age 0-17, electrocardiogram (ECG) performed as part of evaluation, and clinical suspicion of an arrhythmia on presentation. We determined the demographics, presenting concern, laboratory tests performed, ECG results, and final diagnosis.
Results: In total, 177 pediatric patients had 201 emergency room visits where an arrhythmia was suspected. The average age at the time of visit was 10.24 years (SD 5.97 years). There were 97 boys and 104 girls. There was a total of 24 different presenting chief complaints, with the most common being racing heart (72), palpitations (70), and arrhythmia (18). Of the patients evaluated, 51 had a prior arrhythmia diagnosis and 26 had known congenital heart disease.
SVT was documented in 28 and atrial fibrillation in 4 patients. There were single episodes of atrial flutter, ventricular tachycardia, and ventricular fibrillation. Fifty-three visits resulted in hospital admission for management of an arrhythmia or other concern. Following emergency department discharge, 89 patients had an outpatient cardiology follow-up appointment arranged and 56 patients had a Holter monitor ordered.
Of the patients with SVT, conversion occurred spontaneously (3), with vagal maneuvers (6), with adenosine (12), with additional antiarrhythmic medication (2), and with electrical cardioversion (2).
A total of 14 were admitted for additional treatment of their arrhythmia. In total, 123/171 patients had some abnormality on their ECG.
Conclusions: Symptoms suggesting heart rhythm concerns are frequently addressed in the pediatric emergency department, but arrhythmias are diagnosed in a minority of cases. SVT is the most common documented arrhythmia. Future directions include examining frequency and usefulness of laboratory studies ordered as part of arrythmia evaluations in the emergency department.
Adverse Outcomes Associated with Enteral Nutrition in Children with Bronchiolitis Admitted to the PICU and Requiring Non-Invasive Ventilation
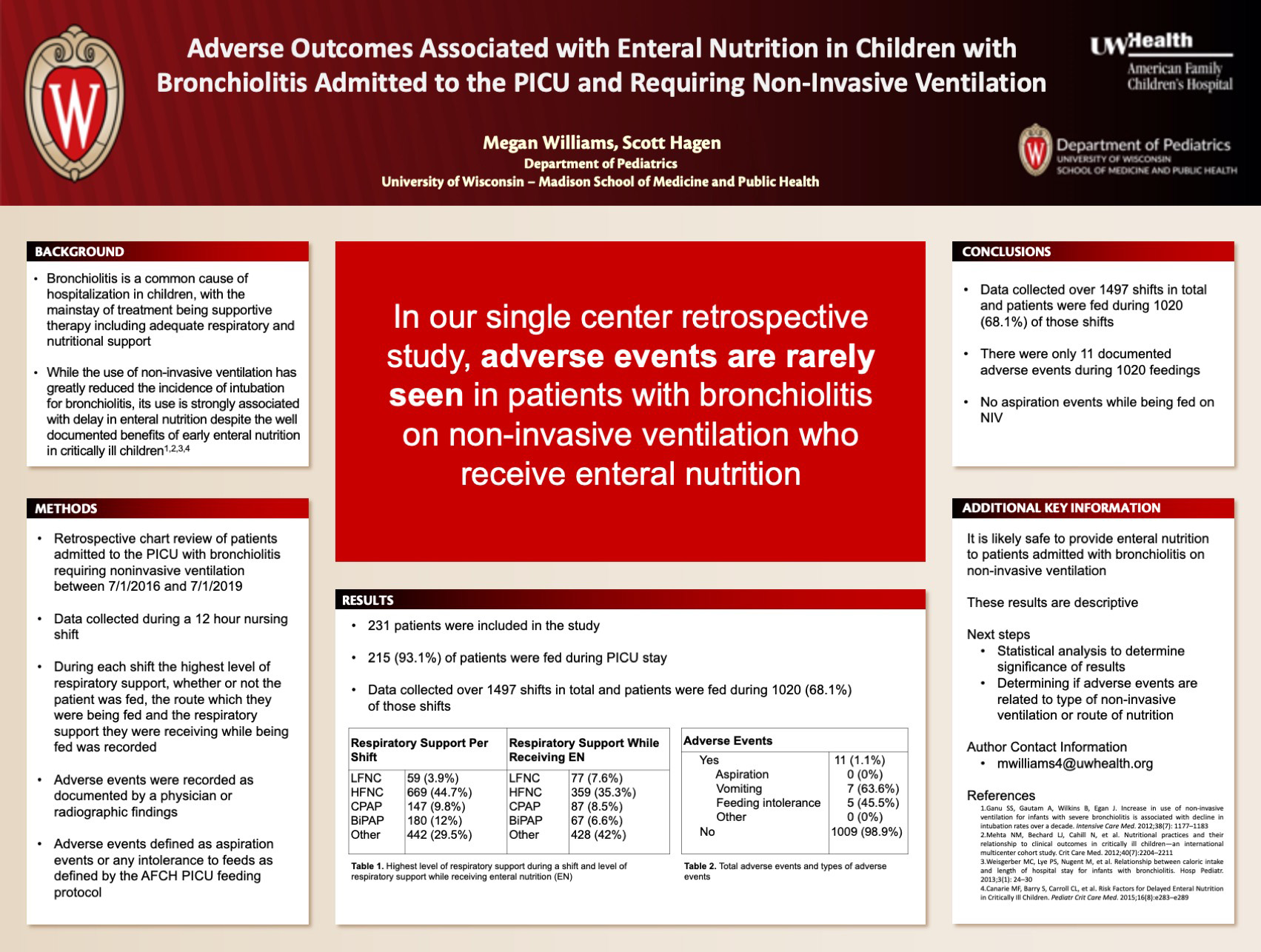
Click here for .pdf version of poster
Title: Adverse Outcomes Associated with Enteral Nutrition in Children with Bronchiolitis Admitted to the PICU and Requiring Non-Invasive Ventilation
Williams M, Hagen S
Background: Bronchiolitis is one of the most common causes of hospitalizations in children less than 2 years old worldwide and the increasing use of non-invasive ventilation has decreased the need for intubation significantly. Nutrition practices in children on non-invasive ventilation vary, and often lead to children being kept NPO despite evidence to support improved outcomes in critical illness with adequacy of nutrition. The purpose of our study is to compare the incidence of adverse outcomes in children receiving nutrition compared to those kept NPO while on HFNC.
Design/Methods: Retrospective study including children less than 24 months admitted to the PICU with bronchiolitis requiring HFNC or non-invasive ventilation between July 1, 2016 and July 1, 2019. Data collected included demographics, amount of respiratory support during each nursing shift (12-hour shifts, 7am – 7pm and 7pm – 7am), respiratory support while fed during each nursing shift, as well as feeding related adverse events.
Results: A total of 231 patients met inclusion criteria and 215 were fed during their PICU stay. Data was recorded over 1497 shifts, with patients being fed during 1020 (68.1%) shifts. Of the 1020 feeding shifts there were 11 (1.1%) documented adverse events. Patients were on HFNC while receiving enteral nutrition during 359 shifts (35.5%), with flow rates ranging from 0.08 L/kg to 3.71 L/kg. Average HFNC flow while receiving enteral nutrition was 1.16 L/kg.
Conclusions: In this single-center retrospective study, adverse events related to feeding while on HFNC were rare.
Progressive Shortness of Breath and Hypoxia in an Adolescent Female Athlete: a Case Report
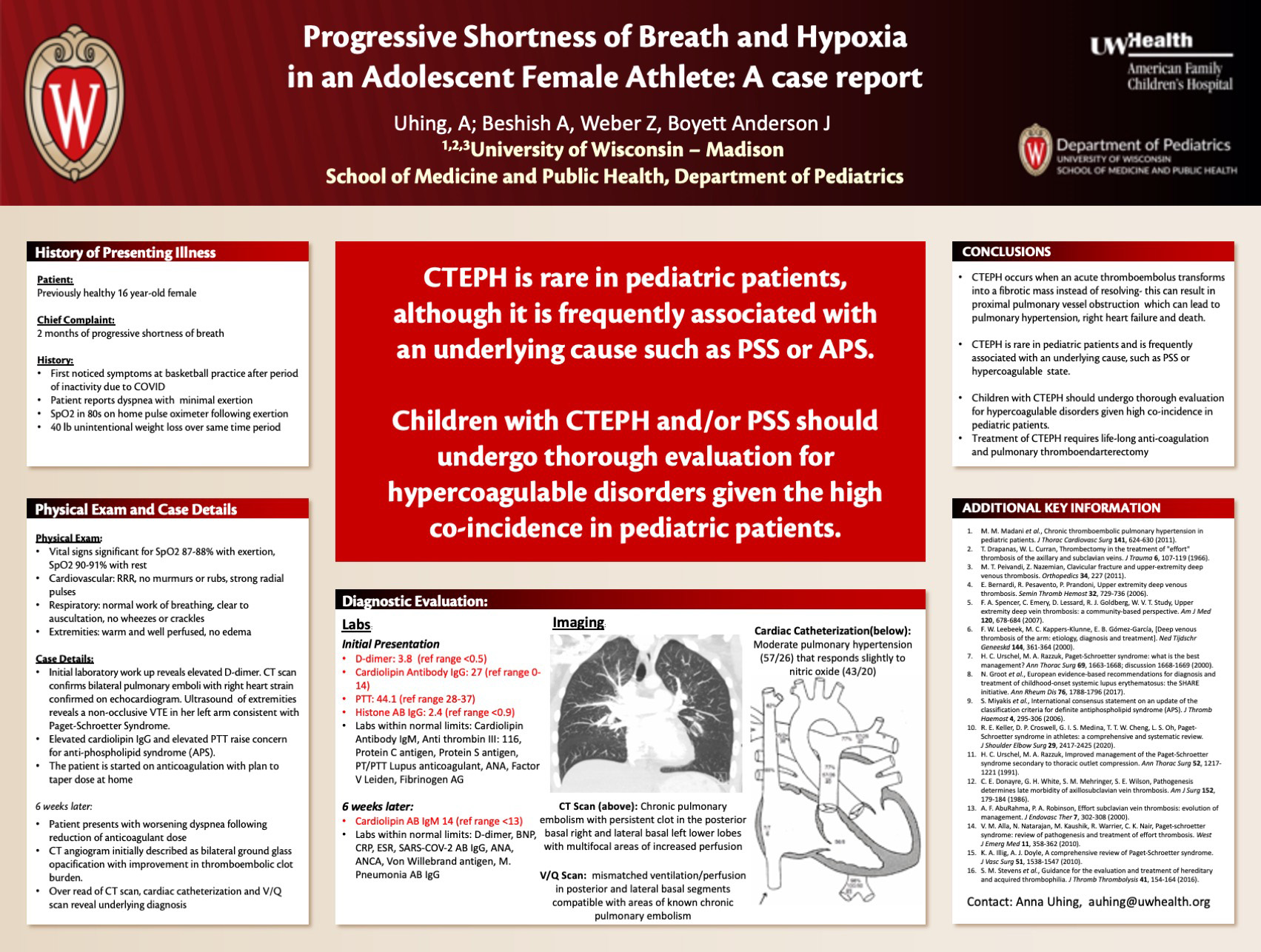
Click here for .pdf version of poster
Title: Progressive Shortness of Breath and Hypoxia in an Adolescent Female Athlete: a Case Report
Uhing A, Beshish A, Weber Z, Boyett Anderson
Case: A 16-year-old female presents to an ED with two months of progressive dyspnea, chest pain, dizziness, and unintentional 40-pound weight loss. Physical exam is notable for oxygen saturations in the high 80s. Elevated D-dimer prompts acquisition of CT angiography that shows acute PE with evidence of right heart strain, confirmed on echocardiography. Extremity ultrasound reveals a non-occlusive VTE in her left arm consistent with Paget-Schroetter Syndrome (PSS). Both cardiolipin IgG and PTT are elevated raising concern for possible antiphospholipid syndrome (APS). The patient is discharged on anticoagulation with a plan to gradually taper her dose. At her Cardiology visit six weeks later, the patient describes worsening dyspnea after decreasing her anticoagulation dose. CT angiogram, cardiac catheterization, and V/Q scan are consistent with chronic thromboembolic pulmonary hypertension (CTEPH) and cardiolipin IgG remains elevated. She is started on oxygen and tadalafil for pulmonary hypertension, re-started on anticoagulation, and referred to another center for definitive treatment of CTEPH with thrombendarteriectomy. During hospitalization for thrombendarteriectomy, her cardiolipin IgG remains elevated, confirming the diagnosis of APS. Due to recurring clot burden despite anticoagulation and thrombendarteriectomy, she is scheduled for staged bilateral thoracic outlet decompression surgeries for treatment of PSS.
Discussion: This case demonstrates the rare presentation of CTEPH in a pediatric patient in conjunction with PSS and APS. CTEPH occurs when an acute thromboembolus transforms into a fibrotic mass instead of resolving. This results in proximal pulmonary vessel obstruction and distal arteriopathy which can lead to pulmonary hypertension, right heart failure and death. CTEPH is only seen in 0.5-3.8% of patients after acute or recurrent PE, although pediatric patients make up only 1% of all patients with this disorder. In children this disorder is often associated with an underlying cause, as seen in the co-incidence of PSS (axillary subclavian vein thrombosis secondary to thoracic outlet narrowing) and APS (thrombosis in the setting of antiphospholipid antibodies detected three months apart). Our case emphasizes the need for thorough evaluation for hypercoagulable disorders in the setting of both CTEPH and PSS given the high co-incidence between these disorders among the pediatric patient population.
The One with Confusion: Tics? Toxic? COVID?
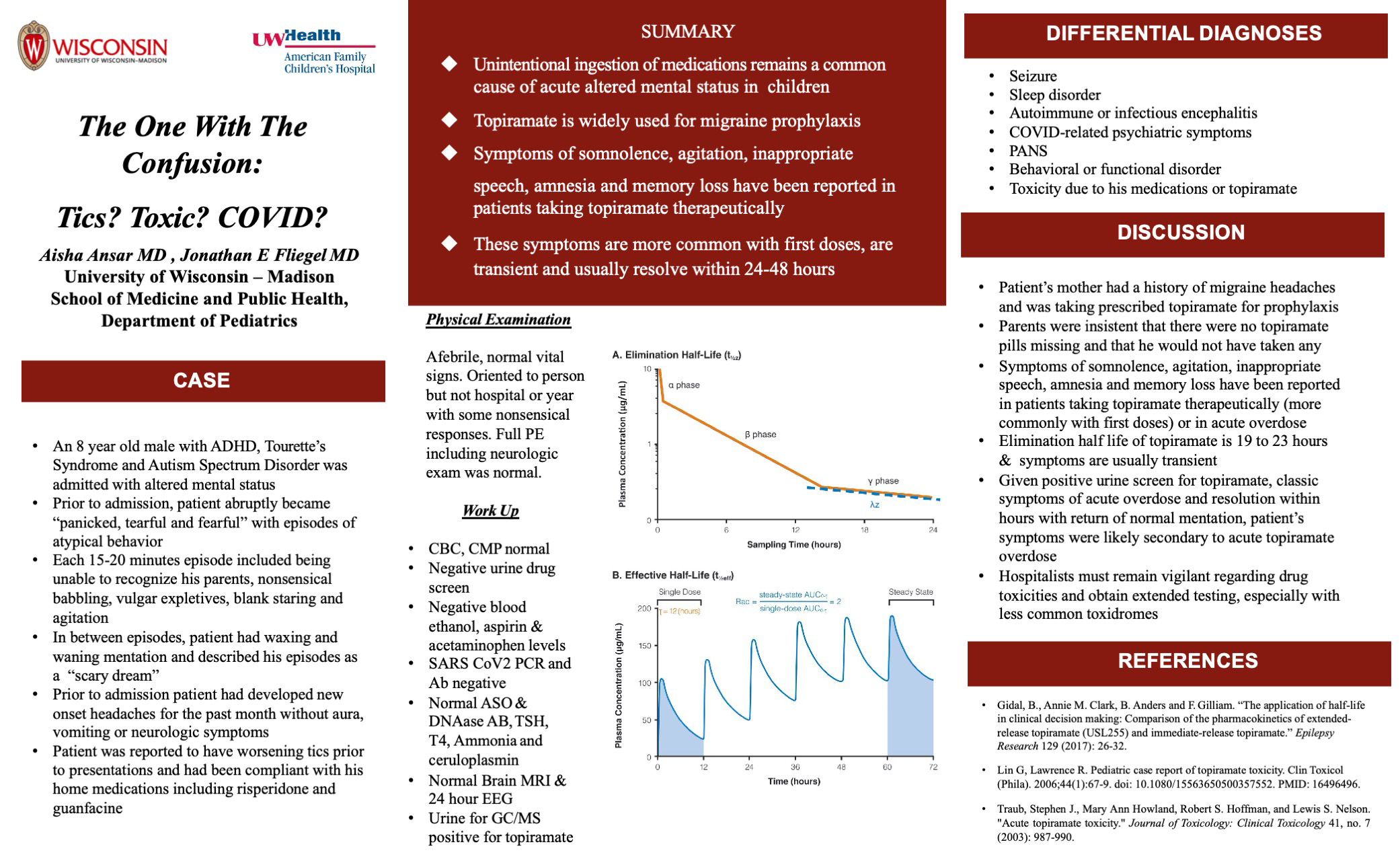
Click here for .pdf version of poster
Title: The One with Confusion: Tics? Toxic? COVID?
Ansar A, Fliegel J
Initial History: An 8-year-old male with ADHD, Tourette’s Syndrome and Autism Spectrum Disorder was admitted with altered mental status. He presented to an outside ED after he abruptly became “panicked, tearful and fearful” and developed behaviors his parents stated were atypical. Episodes lasting 10-15 minutes occurred at home, ED and en route to our hospital. These episodes included being unable to recognize parents, non–sensical babbling, vulgar expletives, blank staring and agitation. In between, his parents report he did not return to normal. Afterwards, he described the experience as a “scary dream.” Additional history revealed new onset headaches for the past month without aura, vomiting or neurologic symptoms. During the previous day, his parents noted more frequent tics. His parents administer his home medications– risperidone and guanfacine and had not changed or missed doses. His mother takes prophylactic topiramate for migraine headaches. Her count showed that no pills were missing. There are no other drugs at home.
Physical exam: Afebrile, normal vital signs. Oriented to person but not hospital or year with some non-sensical responses. Full PE including neurologic exam was normal.
Diagnostic evaluation: In outside ED, labs included normal CBC, CMP, VBG, negative urine drug screen and negative ethanol, aspirin and acetaminophen levels. SARS CoV2 PCR was negative. Subsequently, SARS CoV2 PCR Ab, ASO & DNAse B Ab, TSH, T4, ammonia, and ceruloplasmin were normal. A 24-hour video EEG was normal including during an episode. Brain MRI was normal. After admission, we sent additional urine for GC/MS that was positive for topiramate.
Diagnosis: Acute delirium due to topiramate toxicity.
Discussion: Our differential diagnosis at the time of admission included seizure, sleep disorder, autoimmune or infectious encephalitis, COVID-related psychiatric symptoms, PANS, behavioral or functional disorder, and toxicity due to his medications or topiramate. Symptoms of somnolence, agitation, inappropriate speech and amnesia have been reported in patients taking topiramate therapeutically (more commonly with first doses) or in acute overdose. With an elimination half-life of 19 to 23 hours, symptoms are transient. His symptoms resolved completely over the next day. Despite his positive test, classic symptoms, and resolution as expected, his parents remained insistent that he did not take any topiramate. Hospitalists must remain vigilant regarding drug toxicities and obtain extended testing, especially with less common toxidromes.
Assessing the Risk of Hypovitaminosis and Vitamin C Deficiency in Critically Ill Pediatric Patients Undergoing Cardiopulmonary Bypass
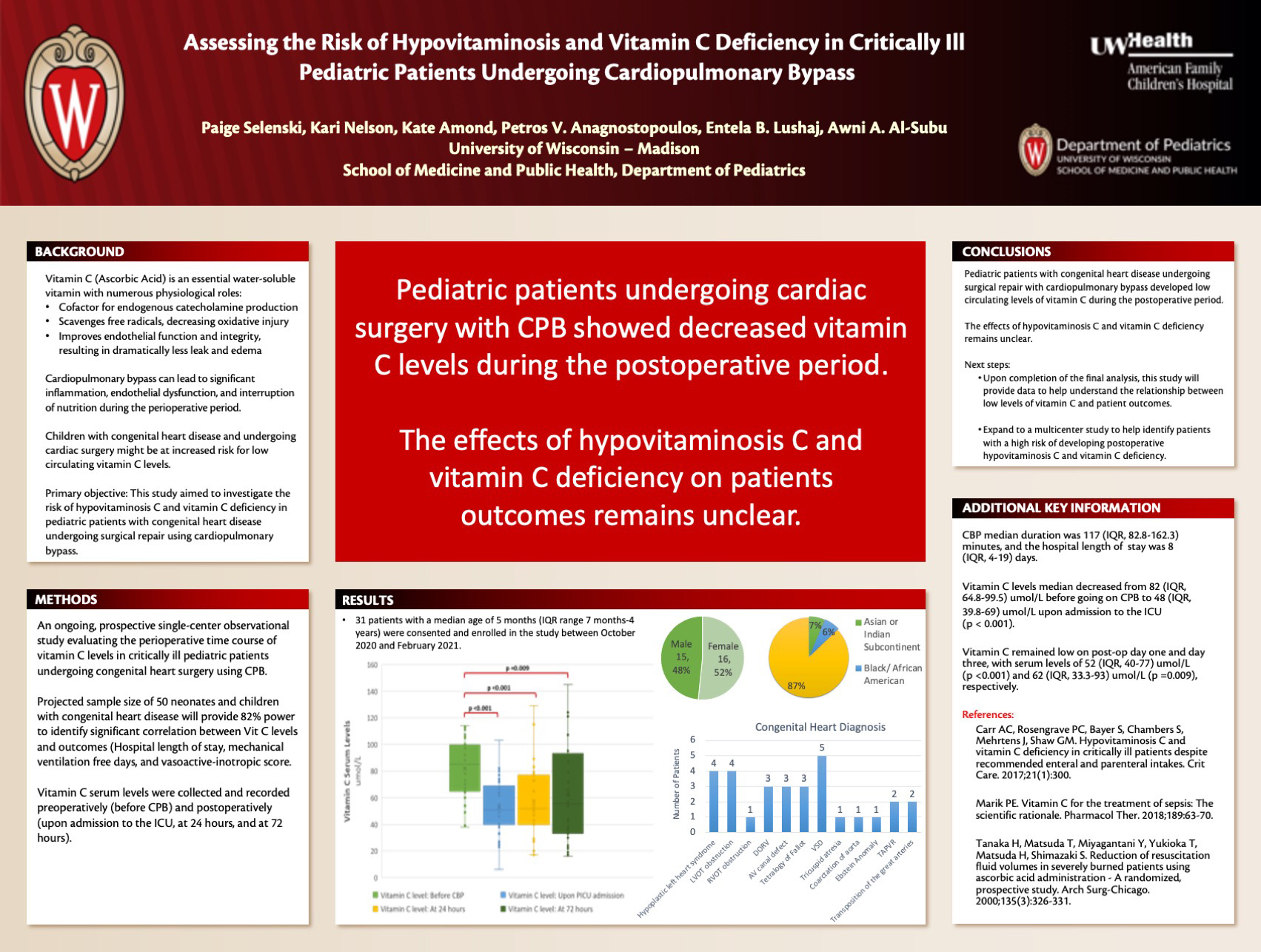
Click here for .pdf version of poster
Title: Assessing the Risk of Hypovitaminosis and Vitamin C Deficiency in Critically Ill Pediatric Patients Undergoing Cardiopulmonary Bypass
Selenski P, Nelson K, Amond K, Anagnostopoulos P, Lushaj E, Al-Subu A
Background: Vitamin C levels are known to be decreased in adult critical illness and associated with illness severity. Cardiopulmonary bypass (CPB) can lead to significant inflammation, endothelial dysfunction, and interruption of nutrition during the perioperative period. Combining these effects, children with congenital heart disease (CHD) and undergoing cardiac surgery might be at increased risk for low circulating vitamin C levels. This study aimed to investigate the risk of hypovitaminosis C and vitamin C deficiency in pediatric patients with congenital heart disease undergoing surgical repair using cardiopulmonary bypass.
Design/Methods: An ongoing prospective single-center observational study evaluating the perioperative time course of vitamin C levels in critically ill children (< 18 years of age) who are undergoing congenital heart surgery using CPB. Vitamin C serum levels were collected and recorded preoperatively (before CPB) and postoperatively (upon admission to the ICU, at 24 hours, and at 72 hours).
Results: A total of 31 patients with a median age of 5 months (range 3 days-17 years) were consented and enrolled in the study between October 2020 and February 2021. CBP median duration was 117 (IQR 82.75-162.25) minutes, and the hospital length of stay was 8 (3-97) days. Vitamin C levels median decreased from 82 (IQR 64.75-99.5) umol/L before going on CPB to 48 (IQR 39.75-69) umol/L upon admission to the ICU (p < 0.001). Vitamin C remained low on post-op day one and day three, with serum levels of 52 (IQR 40-77) umol/L (p <0.001) and 62(IQR 33.25-93) umol/L (p =0.009), respectively.
Conclusions: Pediatric patients undergoing cardiac surgery with CPB showed decreased vitamin C levels during the postoperative period. The effects of hypovitaminosis C and vitamin C deficiency in this population remains unclear, and further investigation is needed to understand the potential effect of treatment with intravenous vitamin C.
Palliative Care in a Pediatric Oncology Population
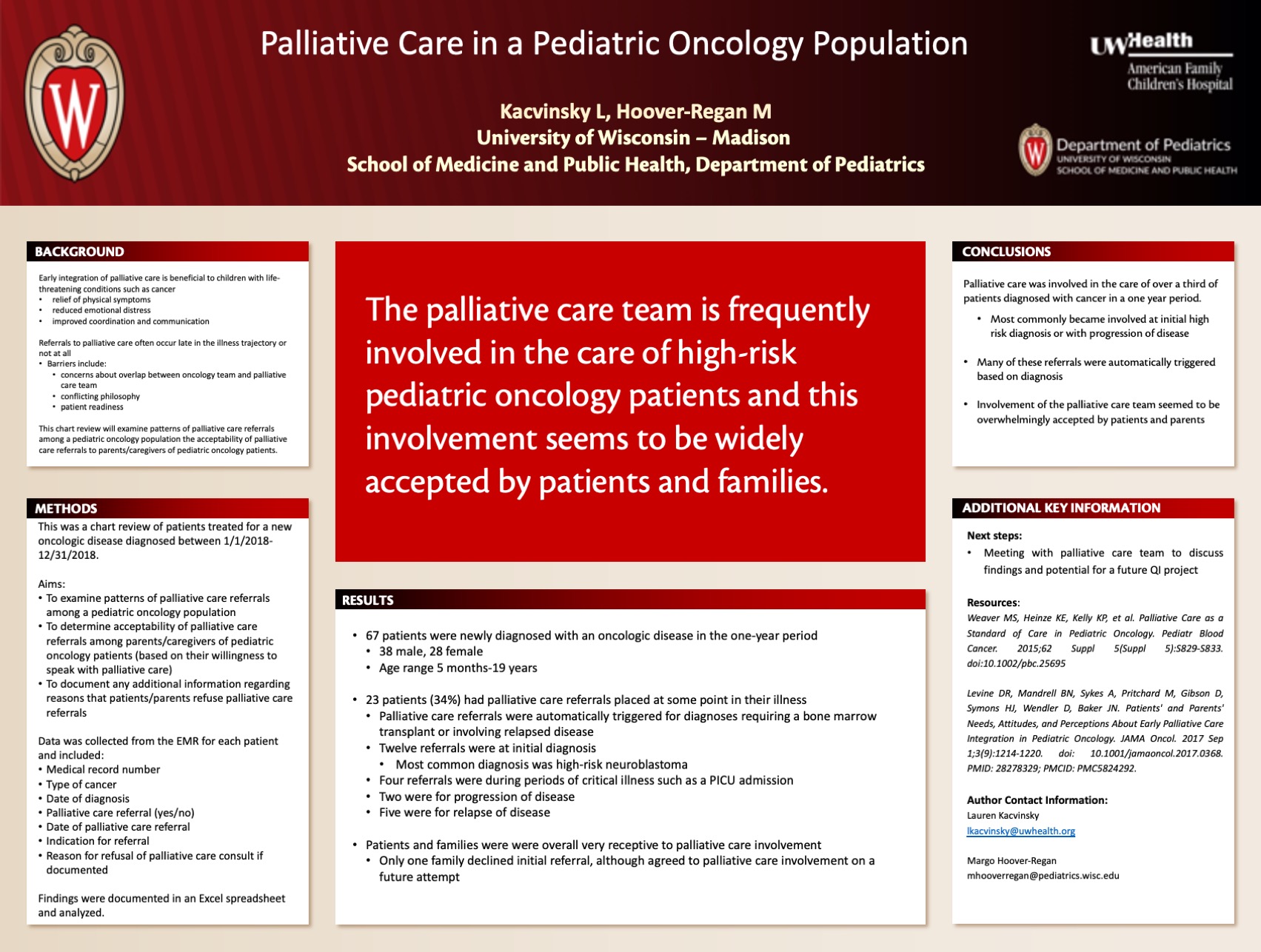
Click here for.pdf version of poster
Title: Palliative Care in a Pediatric Oncology Population
Kacvinsky L, Hoover-Regan M
Background: Early integration of palliative care is beneficial to children with life-threatening conditions such as cancer. Benefits of palliative care include relief of physical symptoms, reduced emotional distress, and improved coordination and communication. However, studies frequently show that referrals to palliative care occur late in the illness trajectory or not at all. Barriers to referral include concerns about overlap between the oncology team and the palliative care team, conflicting philosophy, and patient readiness and emotional influence. This chart review will examine patterns of palliative care referrals among a pediatric oncology population the acceptability of palliative care referrals to parents/caregivers of pediatric oncology patients.
Design/Methods: This was a chart review of patients treated at a medium-sized pediatric children’s hospital for a new oncologic disease diagnosed between 1/1/2018-12/31/2018. A list of patients originally diagnosed during this year was obtained. Data collected from the hospital’s electronic medical record (EMR) included patient medical record number, type of cancer, date of diagnosis, palliative care referral (yes/no), date of palliative care referral, indication for referral, and reason for refusal of palliative care consult if documented. Records were reviewed from date of diagnosis through the present. Findings were documented in an Excel spreadsheet and data was analyzed.
Results: There were 67 patients (39 male, 28 females with age range 5 months-19 yrs) newly diagnosed with an oncologic disease in the one-year period. Of these patients, 23 (34%) had palliative care referrals placed at some point in their illness. Of note, palliative care referrals were automatically triggered for diagnoses requiring a bone marrow transplant or involving relapsed disease. There were 12 referrals at initial diagnosis (most commonly high-risk neuroblastoma), four during periods of critical illness such as a PICU admission, two for progression of disease, and five for relapse. Only one family initially declined palliative care referral although agreed to meet on a subsequent attempt.
Conclusions: The palliative care team was involved in the care of over a third of pediatric oncology patients during a year’s time, with their initial involvement most commonly occurring either at diagnosis of a high-risk disease or at progression/relapse. Patients and caregivers were overall agreeable to palliative care consultation which indicates that families are interested in efforts to improve quality of life.