All sedative drugs suppress the central nervous system in a dose-dependent manner. Typically this is accompanied by a reduction in CO2 responsiveness in the medullary respiratory center. Loss of airway control and respiratory depression are the most common serious adverse effects associated with sedative drug administration. The greater the degree of sedation, the greater the degree of respiratory depression. Respiratory depression increases when combining sedative drugs or when using large doses of a single drug.
Airway Control
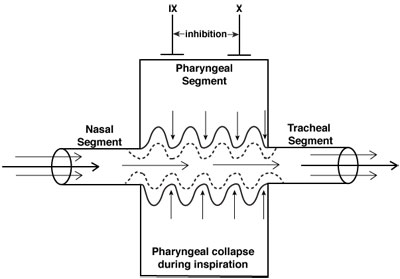
Neuromuscular control of the upper airway (CN IX and X) is inhibited to a greater degree than diaphragmatic activity (phrenic nerve) during sedation/anesthesia. Thus, the negative inspiratory pressures that develop with diaphragmatic contraction may reduce the diameter of the pharynx, a collapsible segment between two relatively well-supported structures, the nasal passage and the trachea. These areas typically involve narrowing of the anterior-posterior distance between the posterior pharynx and the soft palate, epiglottis, and, to a lesser degree, the base of the tongue. Consequently, the pharyngeal segment functions as a Starling resistor, a collapsible tube whose caliber is influenced by pressures within the lumen of the airway and soft tissue.
Airway obstruction during moderate or deep sedation occurs in the supraglottic structures due primarily to the soft palate and epiglottis falling back to the posterior pharynx. While it was previously thought that the base of the tongue was the primary cause of upper airway obstruction during unconsciousness, MRI studies of the airway in sedated children demonstrate that the soft palate and epiglottis are the most likely structures causing the obstruction.
The keys to appropriately managing the pediatric airway during sedation are proper airway positioning and application of positive pressure ventilation when required. Routine management of the pediatric airway includes placement of the patient’s neck in the sniffing position, often with a rolled towel placed underneath the shoulders and administration of “blow-by” oxygen. If obstruction persists despite these maneuvers, the patient’s airway should be repositioned and a chin lift performed to move the supraglottic soft tissue structures, primarily soft palate and epiglottis, anteriorly and away from the posterior pharynx. If a simple chin lift fails to relieve the obstruction, this should be followed by a jaw thrust and application of positive pressure through a flow-inflating anesthesia bag and mask. Failure to relieve the obstruction following application of positive pressure (PEEP) requires positive pressure ventilation with cricoid pressure and endotracheal intubation when necessary.
Ventilation Control
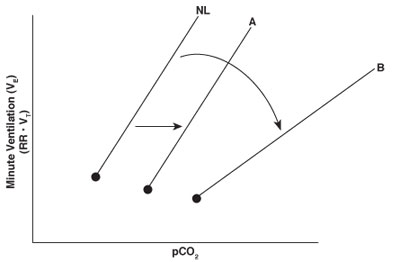
The central respiratory center is primarily located in the medulla and rapidly responds to changes in carbon dioxide. Changes in carbon dioxide concentration are among the most important determinants of respiratory drive from the medullary respiratory center. Carbon dioxide freely diffuses across the blood-brain barrier, resulting in an increase in H+ and a decrease in pH in the cerebral spinal fluid. The decrease in pH is accompanied by an increase in neural output from the respiratory center and in minute ventilation. Minute ventilation typically increases linearly with rises in PCO2.
The normal response to increases in carbon dioxide is noted by the line designated NL in the CO2 ventilation response curve. In general, sedative drugs suppress the central respiratory center and reduce the ventilatory response to a given level of carbon dioxide. Doses of sedative drugs that do not cause complete loss of consciousness (e.g., low-dose morphine or midazolam) usually displace only the CO2 ventilation response curve to the right while maintaining the slope of the response (line A). Under deeper levels of sedation, however, the slope of the CO2 ventilation response curve decreases as well as shifts to the right (line B). This response may occur when combining sedative drugs or using any sedative that results in unconsciousness. A decreased slope indicates less of an increase in minute ventilation for any given rise in carbon dioxide, a situation that may lead to severe hypercapnia, hypoxemia, or apnea.