Session A: Translational and Mechanisms of Disease Abstracts – Blackboard Collaborate Session
This is an accordion element with a series of buttons that open and close related content panels.
Inflammasome Activation To Staphylococcus aureus Is Associated With Increased Wheezing In Early Life
Click here for .pdf version of poster
TITLE:
Inflammasome Activation To Staphylococcus aureus Is Associated With Increased Wheezing In Early Life
Eric Schauberger, Victoria Rajamanickam, Robert F Lemanske, Jr., James E Gern, Daniel J Jackson
RATIONALE:
Aberrant immune responses to pathogenic airway bacteria in infancy have been associated with the development of asthma later in childhood. Bacterial products activate the inflammasome which is critical for the generation of the proinflammatory cytokines IL-1beta and IL-6. We hypothesized that increased inflammasome activation to Staphylococcus aureus in peripheral blood mononuclear cells (PBMCs) will be associated with early childhood wheezing.
METHODS:
PBMCs were obtained at age 1 year from children enrolled in the Childhood Origins of Asthma (COAST) study. Cells were stimulated with Staphylococcus aureus Cowan strain (SAC) for 24 hours and supernatants collected and stored. A multiplex cytokine assay was used to quantitate IL-1beta and IL-6 production. Nasal samples were collected during respiratory illnesses and etiology was assessed by multiplex PCR. We examined associations between inflammasome activation at age 1 year and histories of wheezing during early childhood.
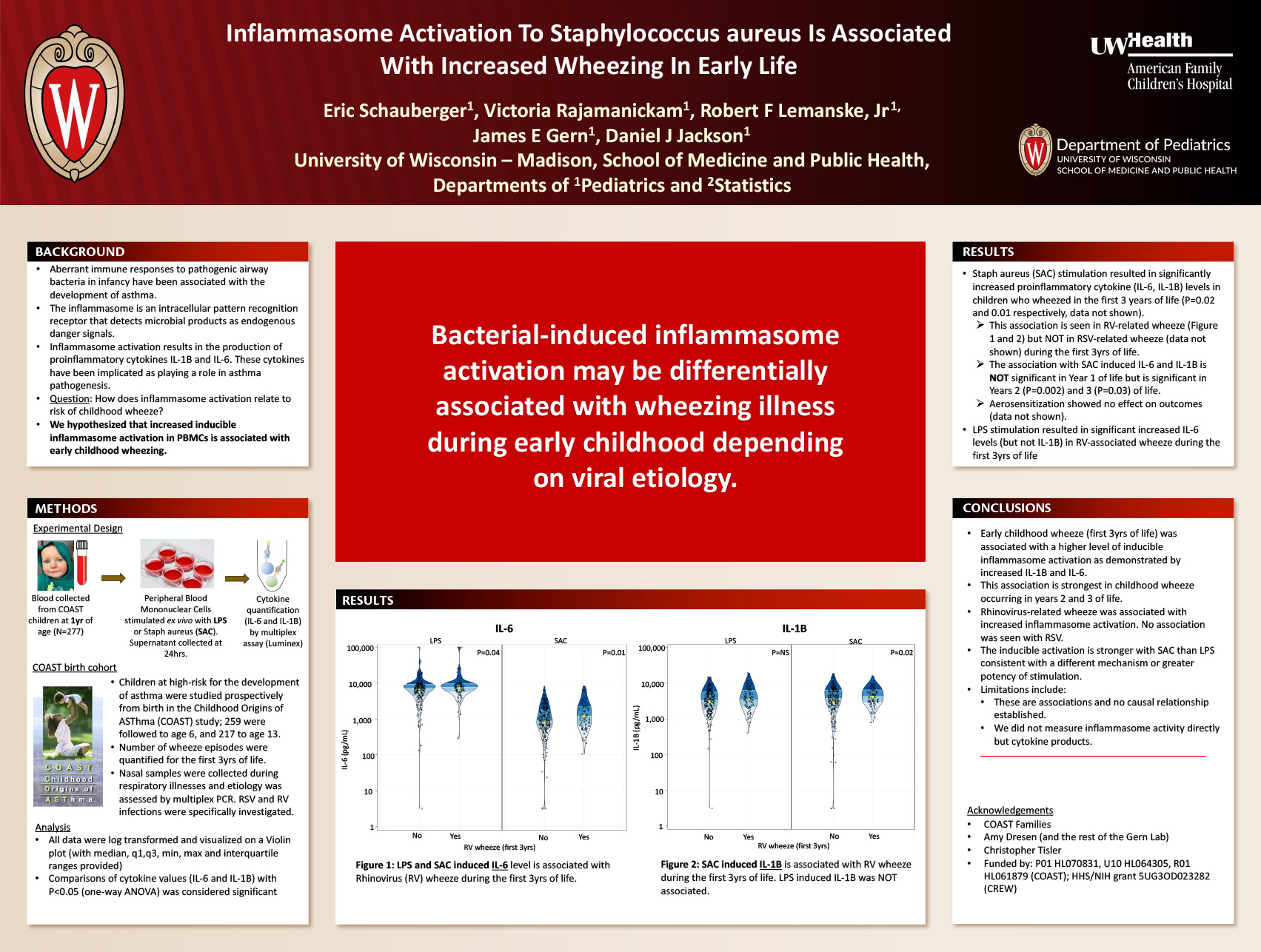
RESULTS:
Stimulation of PBMCs with SAC resulted in significantly increased concentrations of IL-6 (p=0.02) and IL-1beta (p=0.01) in children with wheezing in the first 3 years of life. Children with rhinovirus (RV) wheezing in the first 3 years of life had increased SAC-induced IL-6 (p=0.002) and IL-1beta (p=0.003). However, RSV wheezing was not associated with differential SAC- induced IL-6 or IL-1beta (p=NS).
CONCLUSIONS:
Stimulated PBMCs from children with RV (but not RSV) associated wheeze produce increased levels of proinflammatory cytokines IL-1beta and IL-6. These data suggest that bacterial inflammasome activation may be differentially associated with wheezing illnesses during early childhood depending on viral etiology.
Sex differences in hippocampal brain derived steroid contents following hypoxic ischemic encephalopathy
Click here for .pdf version of poster
Title: Sex differences in hippocampal brain derived steroid contents following hypoxic ischemic encephalopathy
Hackett1,2; B. Ozaydin3; N. Deveci1,2; S. Yapici1,2M; N. Aycan1; R.W. Goy4; A. Kapoor4; P. Ferrazzano1,2; J. Levine4,5; P. Cengiz1,2
1Waisman Center, University of Wisconsin, Madison, WI, USA; 2Department of Pediatrics, Division of Critical Care Medicine, University of Wisconsin, Madison, WI, USA; 3Department of Neurosurgery, Division of Critical Care Medicine, University of Wisconsin, Madison, WI, USA 4Wisconsin National Primate Research Center, Madison, WI, USA; 5Department of Neuroscience, University of Wisconsin, Madison, WI, USA
Background: Neonatal hypoxia ischemia (HI) related encephalopathy is one of the major causes of learning disabilities and memory deficits in children. Clinical and experimental studies have shown that male newborns are two times more susceptible to the effects of HI, a phenomenon that is poorly understood. Our recent studies show that estrogen receptor alpha (ER) expression is upregulated following HI in the female hippocampus and confers sex-specific neuroprotection via a neurotrophin receptor, tyrosine kinase B receptor (TrkB).
Objective: To determine whether the neuroprotective responses following HI are mediated by brain derived estradiol (E2) as a ligand to ER produced by local aromatization of testosterone (T).
Design/Methods: HI was induced in P9 C57BL/6J mice by left common carotid artery ligation and exposure of the mice to 10% O2 for 50 min using Vannucci’s HI model. Hippocampi were dissected, weighted and frozen immediately 3 days post-HI. For E2 and T content measurement, two IL hippocampi were pooled and homogenized on ice in lysis buffer containing preservatives. Extractions were then performed on the homogenate to clean and concentrate the sample and analyzed for hormones by LC-MS/MS. ANOVA was used to compare IL hippocampal E2 and T contents of sham and HI mice.
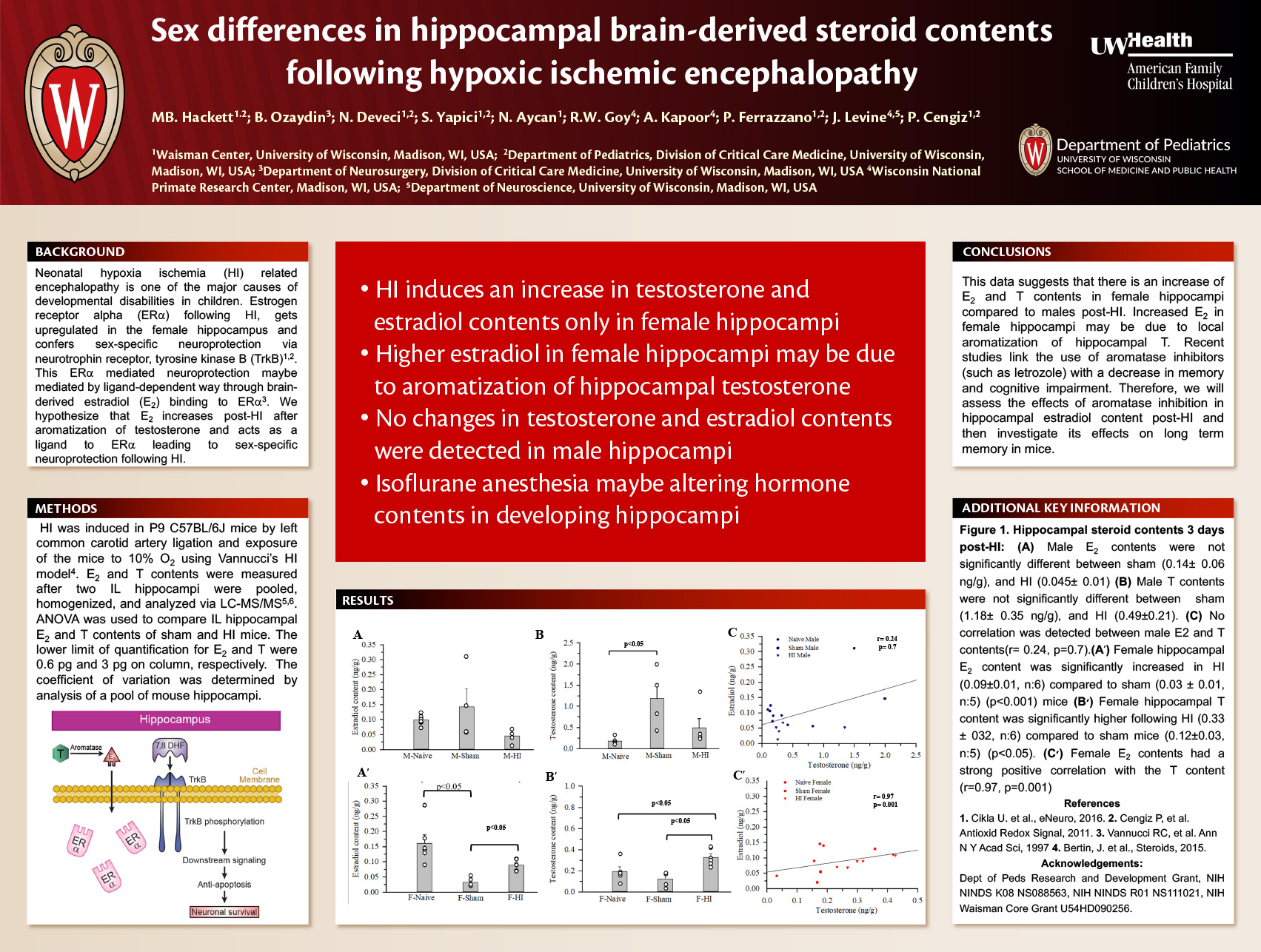
Results: The limit of quantitation for E2 and T were 0.6 pg and 3 pg on column, respectively. Hippocampal E2 and T contents were not significant between male sham (0.14± 0.06 and 1.18±
0.35 ng/g, n:4) and HI (0.045± 0.009 and 0.49±0.21, n:5) mice, respectively. Female hippocampal E2 content was significantly increased in HI (0.09±0.007, n:6) compared to sham (0.03 ± 0.007, n:5) (p<0.001) mice. Female hippocampal T content was significantly higher in HI (0.33 ± 032, n:6) compared to sham (0.12±0.03, n:5) (p<0.05) mice. HI increased E2 content in female hippocampi compared to male (p<0.05). No significant difference was detected in hippocampal T content between sexes.
Conclusion(s): This data suggest that HI induces increase of E2 and T in female hippocampi compared to males 3 days post-HI. We will next test the effect of aromatase inhibition on hippocampal E2 contents.
Combining an engineered costimulatory vaccine with NK cells induces an anti-tumor effect against murine neuroblastoma in vitro and after bone marrow transplant in vivo
Click here for .pdf version of poster
Nicholas R. Mohrdieck1, Sean P. Rinella1, Paul D. Bates1, Christian M. Capitini1,2
1Department of Pediatrics University of Wisconsin School of Medicine and Public Health, 2UW Carbone Cancer Center
Background
High risk neuroblastoma remains a challenge to cure despite multi-modality treatment, with only 50% survival. “Tumor-specific” therapies are needed to improve survival. AgN2a 4P is an aggressive variant of the murine neuroblastoma cell line, Neuro-2a, that is engineered to express four co-stimulatory markers: CD54, CD80, CD86, and CD137L, but has never been studied after allogeneic bone marrow transplant (BMT).
Objective
The objective of this study was to observe anti-tumor immunity by vaccination of AgN2a 4P, with and without adoptive transfer of donor-derived NK cells, in a post allogeneic BMT model.
Design/Methods
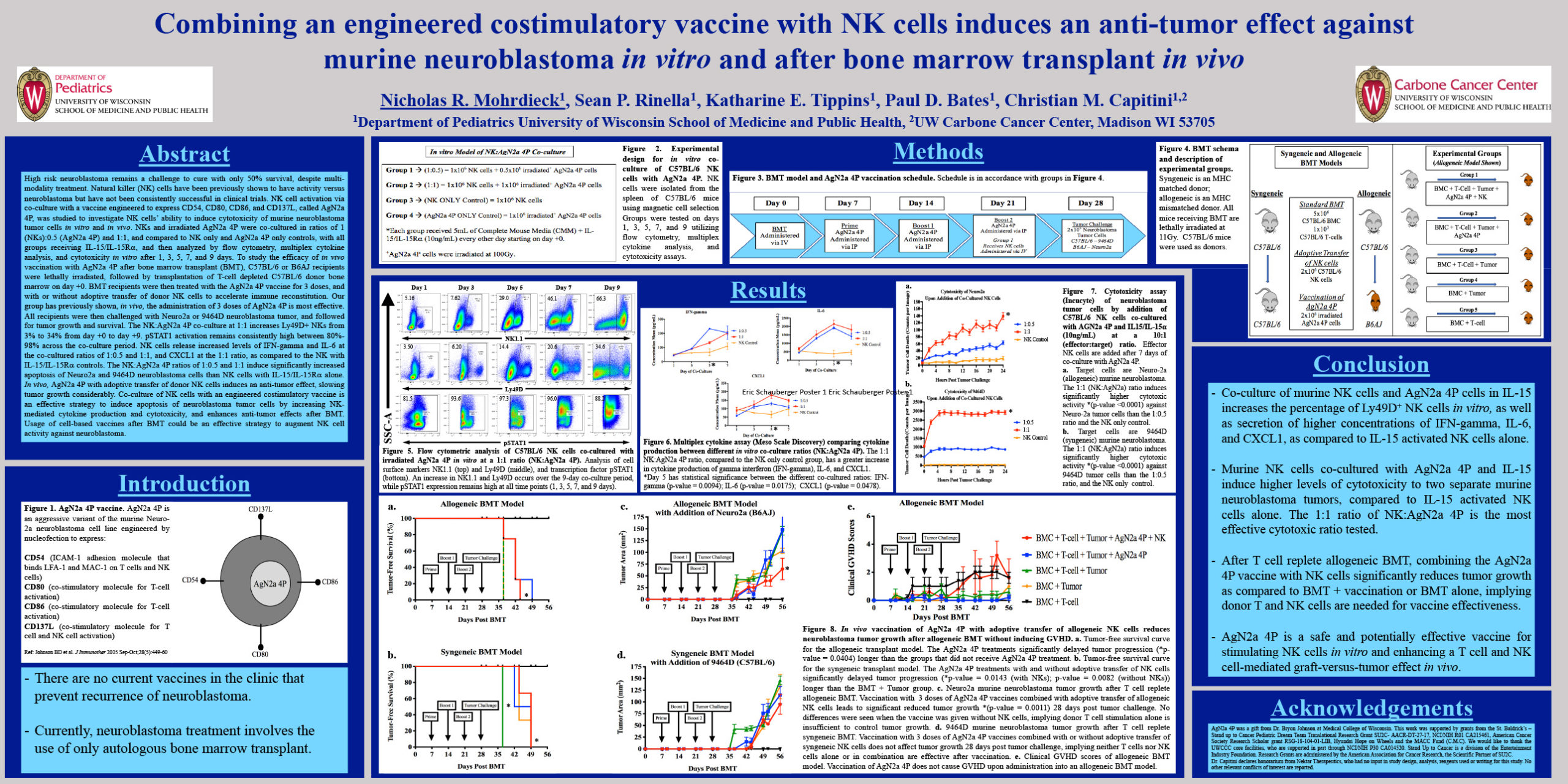
In vitro, we co-cultured donor-derived NK cells with the AgN2a 4P vaccine, at ratios of 1:1 and 1:0.5 (NK:AgN2a 4P). After 7 days, cytotoxicity was tested on Neuro-2a (allogeneic) and 9464D (syngeneic) neuroblastoma tumor cell lines. In vivo, we performed syngeneic (MHC-matched) and allogeneic (MHC- mismatched) BMT, using C57BL/6 and B6AJ mouse recipients. The standard BMT included 5e6 C57BL/6 BMC and 1e3 C57BL/6 T-cells. The AgN2a 4P vaccine was administered on day +7, +14, and
+21 to the respective groups. C57BL/6 donor-derived NK cells were administered on day +21 to the respective group. Neuroblastoma tumor challenge was introduced on day +28. All groups were tracked for tumor-free survival, tumor growth, and clinical score.
Results
In vitro, the co-culture of donor-derived NK cells with the AgN2a 4P vaccine at the 1:1 ratio had significantly (P<0.0001) increased cytotoxicity against both neuroblastoma tumor cell lines, compared to the 1:0.5 ratio and an NK only control. In vivo, an allogeneic BMT with AgN2a 4P vaccination, and with donor-derived NK cells, induced significant (p=0.0011) anti-tumor immunity compared to AgN2a 4P vaccination alone, and tumor only controls. The syngeneic BMT model did not show significant anti- tumor immunity. Based on clinical score data, administration of the AgN2a 4P vaccine in an allogeneic BMT model does not cause GVHD.
Conclusion
Based on data, we can conclude that AgN2a 4P can induce an anti-tumor effect against neuroblastoma in vitro, and in vivo, after allogeneic BMT with adoptive transfer of NK cells. It was also demonstrated that administration of the AgN2a 4P vaccine in the allogeneic BMT model did not cause GVHD. Future studies are focusing on addition of immune inhibition blockade to induce preventative anti-tumor immunity.
Epigenetic Regulation of Estrogen Receptor Alpha via DNA Repair Gene Gadd45b Following Neonatal Hypoxic Ischemic Encephalopathy
Click here for .pdf version of poster
Nida Karahan1; Vishal Chanana1; Jaya Chandrashekhar1; Dila Zafer1; Burak Ozaydin1; Peter Ferrazzano1,2; AP Auger4; JE Levine3; Pelin Cengiz1,2
1Waisman Center, University of Wisconsin, Madison, WI, USA; 2Department of Pediatrics, Division of Critical Care Medicine, University of Wisconsin, Madison, WI, USA; 3Department of Neuroscience, University of Wisconsin, Madison, WI, USA; 4Department of Psychology, University of Wisconsin, Madison, WI, USA
Background: Neonatal hypoxia ischemia (HI) related encephalopathy is an important cause of life-long mortality and morbidity. Female newborn brains are relatively resistant to the detrimental effects of HI while male newborn brains are more susceptible. Our recent findings reveal that HI increases hippocampal estrogen receptor a (ERa) expression leading to neuroprotection only in the female mice hippocampi through crosstalk with the neurotrophin receptor, tyrosine kinase B (TrkB). We hypothesized that upregulation of ERa in female hippocampu is regulated by epigenetic mechanisms. We hypothesized that gadd45b upregulation is required for ERa upregulation leading to TrkB-mediated neuroprotection in female hippocampi following neonatal HI.
Objective: To determine the underlying epigenetic mechanisms of sex-specific ERa upregulation.
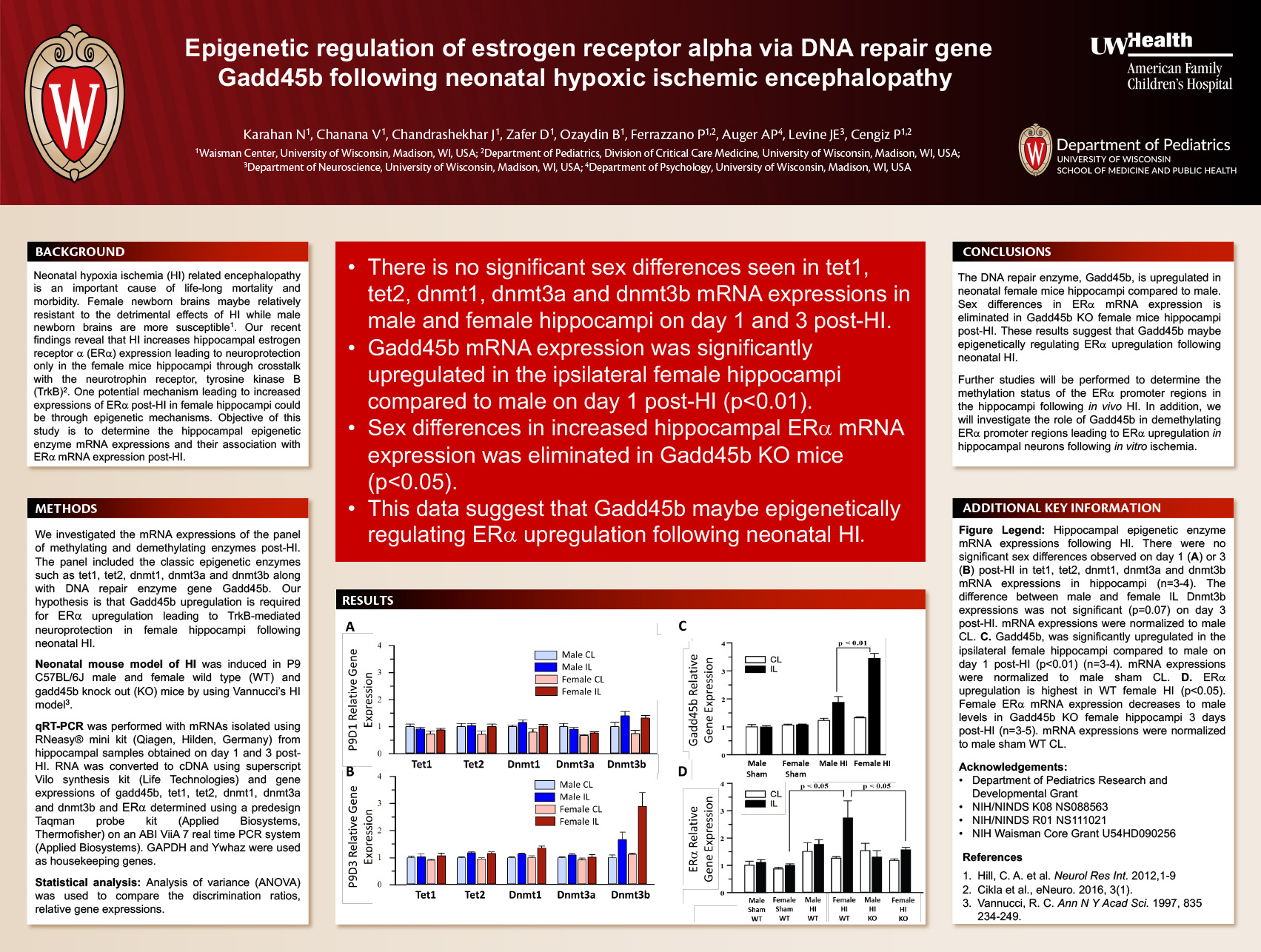
Design/Methods: HI was induced in P9 C57BL/6J male and female wild type (WT) and gadd45b knock out (KO) mice by using Vannucci’s HI model. We investigated the panel of methylating and demethylating genes including gadd45b, tet1, tet2, dnmt1, dnmt3a and dnmt3b. Hippocampi were extracted at 1 day and 3 days post-HI for gadd45b, tet1, tet2, dnmt1, dnmt3a and dnmt3b and ERa mRNA expressions using qPCR, respectively. ANOVA was used for analysis (mean ± SEM).
Results: We did not observe any significant sex differences on day 1 or 3 post-HI in tet1, tet2, dnmt1, dnmt3a and dnmt3b expressions in hippocampi of male and female neonates. Interestingly, the demethylating DNA repair enzyme, gadd45b, was significantly upregulated in the ipsilateral female hippocampi compared to male post-HI on day 1 (p<0.01). Increased hippocampal ERa expression was eliminated in gadd45b KO female mice (p<0.05).
Conclusion: Our results suggest that ERa upregulation in female hippocampi is differentially modulated by the gadd45b. Further studies will be performed to study the role of gadd45b in demethylating ERa promoter regions leading to ERa upregulation following HI.
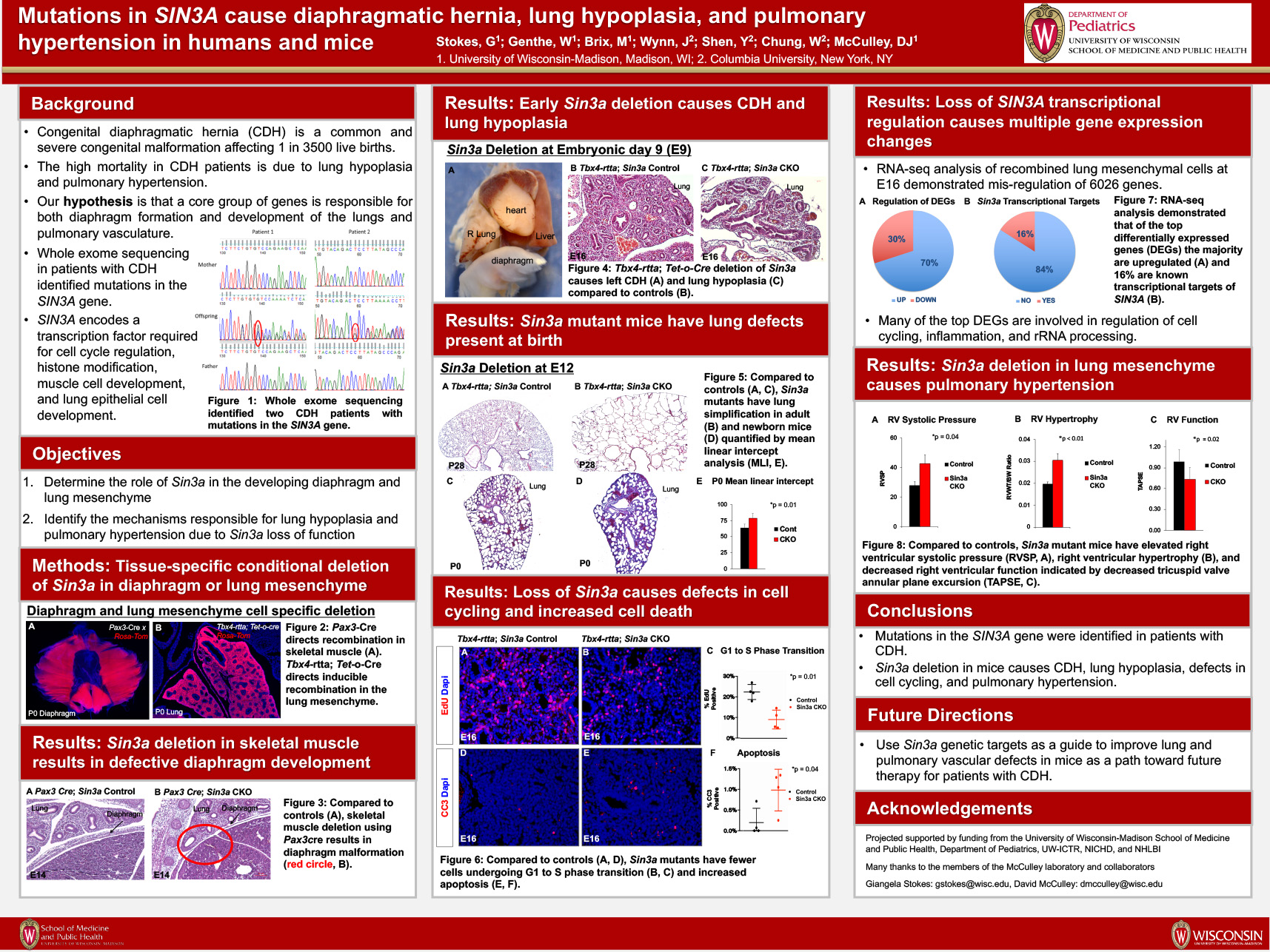
Mutations in SIN3A cause diaphragmatic hernia, lung hypoplasia, and pulmonary hypertension in humans and mice
Click here for .pdf version of poster
AUTHORS (LAST NAME, FIRST NAME): Stokes, Giangela M.1; Genthe, William1; Brix, Maria1; Wynn, Julia2; Hernan, Rebecca2; Shen, Yufeng2; Chung, Wendy2; McCulley, David J.1
INSTITUTIONS (ALL):
- University of Wisconsin-Madison, Madison, WI, United States.
- Columbia University, New York, NY, United States.
Background: Congenital diaphragmatic hernia (CDH) is a common and severe congenital malformation, affecting 1 in 3500 live births, with a mortality rate of 20-50%. The high mortality is due to failure of normal lung and pulmonary vascular development causing a lethal combination of lung hypoplasia and pulmonary hypertension. The severity of these defects is highly variable between patients, and their developmental origins are unclear. We hypothesize that a core group of genes is required for both diaphragm formation and development of the lungs and pulmonary vasculature. Using genome sequencing, mutations in the SIN3A gene have recently been identified in patients with CDH; however, the role that SIN3A plays in diaphragm, lung, or pulmonary vascular development remains unclear.
Objective: To determine the role of Sin3a in the developing diaphragm and lung mesenchyme and identify the mechanisms responsible for lung hypoplasia and pulmonary hypertension.
Design/Methods: Using a tissue-specific, conditional knockout approach in a mouse model, we inactivated the expression of Sin3a in the developing diaphragm or lung mesenchyme. We used a combination of histology and gene expression analysis to analyze the mutant phenotype.
Results: Deletion of Sin3a in the diaphragm mesothelium or skeletal muscle resulted in failure of diaphragm formation and CDH in mice. Furthermore, deletion of Sin3a in the lung mesenchyme alone resulted in lung hypoplasia and pulmonary hypertension in the absence of CDH. Lung and pulmonary vascular defects were caused by failure of G1 to S-phase transition and impaired cellular differentiation in Sin3a mutant lungs. RNA-seq analysis from embryonic and post-natal lungs revealed a majority of differentially expressed genes to be expressed in the mesenchyme, along with an over-representation of genes to be upregulated in Sin3a mutant mice. A majority of the top differentially expressed genes were found to play roles in cell cycling, inflammation, and ribosomal RNA processing.
Conclusion(s): Mutations in the SIN3A gene were identified in humans with CDH. Tissue-specific deletion of Sin3a resulted in CDH with lung hypoplasia and pulmonary hypertension. Sin3a is required for normal cell proliferation and differentiation during lung development. These data support the model that genetic defects in patients with CDH can cause abnormal development of the lung and pulmonary vasculature independent of the associated diaphragm defect.
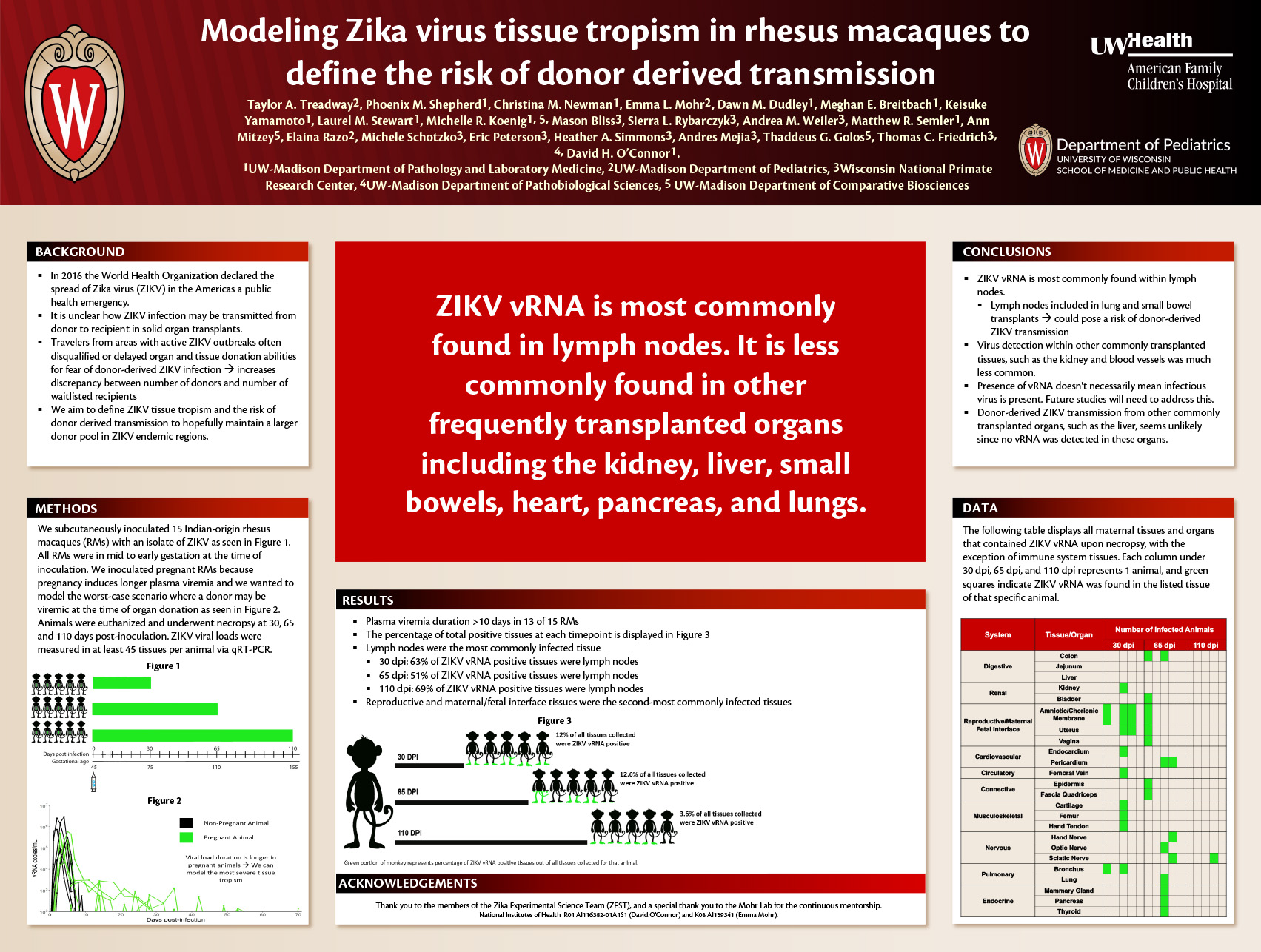
Modeling Zika virus tissue tropism in rhesus macaques to define the risk of donor derived transmission
Click here for .pdf version of poster
Taylor A. Treadway2, Phoenix M. Shepherd1, Christina M. Newman1, Emma L. Mohr2, Dawn M. Dudley1, Meghan E. Breitbach1, Keisuke Yamamoto1,, Laurel M. Stewart1,, Michelle R. Koenig1,5, Mason Bliss3, Sierra L. Rybarczyk3, Andrea M. Weiler3, Matthew R. Semler1, Ann Mitzey5, Elaina Razo2, Michele Schotzko3, Eric Peterson3, Heather A. Simmons3, Andres Mejia3, Thaddeus G. Golos5, Thomas C. Friedrich3,4, David H. O’Connor1.
1UW-Madison Department of Pathology and Laboratory Medicine, 2UW-Madison Department of Pediatrics, 3Wisconsin National Primate Research Center, 4UW-Madison Department of Pathobiological Sciences, 5UW-Madison Department of Comparative Biosciences
Background: Almost 115,000 people in the United States are currently on a transplant waitlist, which vastly exceeds the number of organ donors every year. This discrepancy emphasizes the need for retention of all possible donors. Those who have recently traveled to an area with an active outbreak of Zika virus (ZIKV) are often disqualified as a donor because immunosuppressed recipients would be at risk of a donor-derived ZIKV infection.
Objective: We aim to define ZIKV tissue tropism and the risk of donor derived transmission using a rhesus macaque (RM) model.
Methods: We subcutaneously inoculated 15 Indian-origin rhesus macaques with a Puerto Rican isolate of ZIKV (PRVABC59). We inoculated during pregnancy because plasma viremia is typically prolonged in pregnancy and we wanted to model tissue tropism for donor derived transmission in the worst scenario of prolonged viremia. At 30, 65, and 105 days post-infection (dpi), the animals were euthanized and comprehensive necropsies were performed, which evaluated a minimum of 60 tissues per animal. ZIKV RNA was quantified in tissues via qRT-PCR.
Results: Plasma viremia duration was >10 days in 13 of 15 RMs. ZIKV RNA was most commonly detected in lymph nodes, with 19/45 vRNA positive lymph nodes in 5 RMs at 30 dpi. There were 15/45 vRNA positive lymph nodes at 60 dpi and 8/38 at 105 dpi. Reproductive and maternal fetal-interface (MFI) tissues were the second most commonly positive tissues. Twenty-five MFI tissues, including the amniotic/chorionic membrane, decidua, placenta, uterus, and placental bed, were positive. Other vRNA positive tissues included the primary bronchus, femoral vein, kidney, thyroid, lung, colon, mammary gland, pericardium, hand nerve, and sciatic nerve in 1-2 RMs at one of the three timepoints.
Conclusions: We found ZIKV RNA most frequently within lymph nodes. Lymph nodes are included in lung and small bowel transplants, indicating that these transplants could pose a risk of donor-derived ZIKV transmission. Virus detection within other commonly transplanted tissues was much less common. We did not determine what fraction of vRNA comes from replication-competent virus in each tissue; some tissues with vRNA might not contain virions that could initiate new infections. Donor-derived Zika virus transmission from other commonly transplanted organs, such as liver, seems unlikely since no viral RNA was detected in this organ.
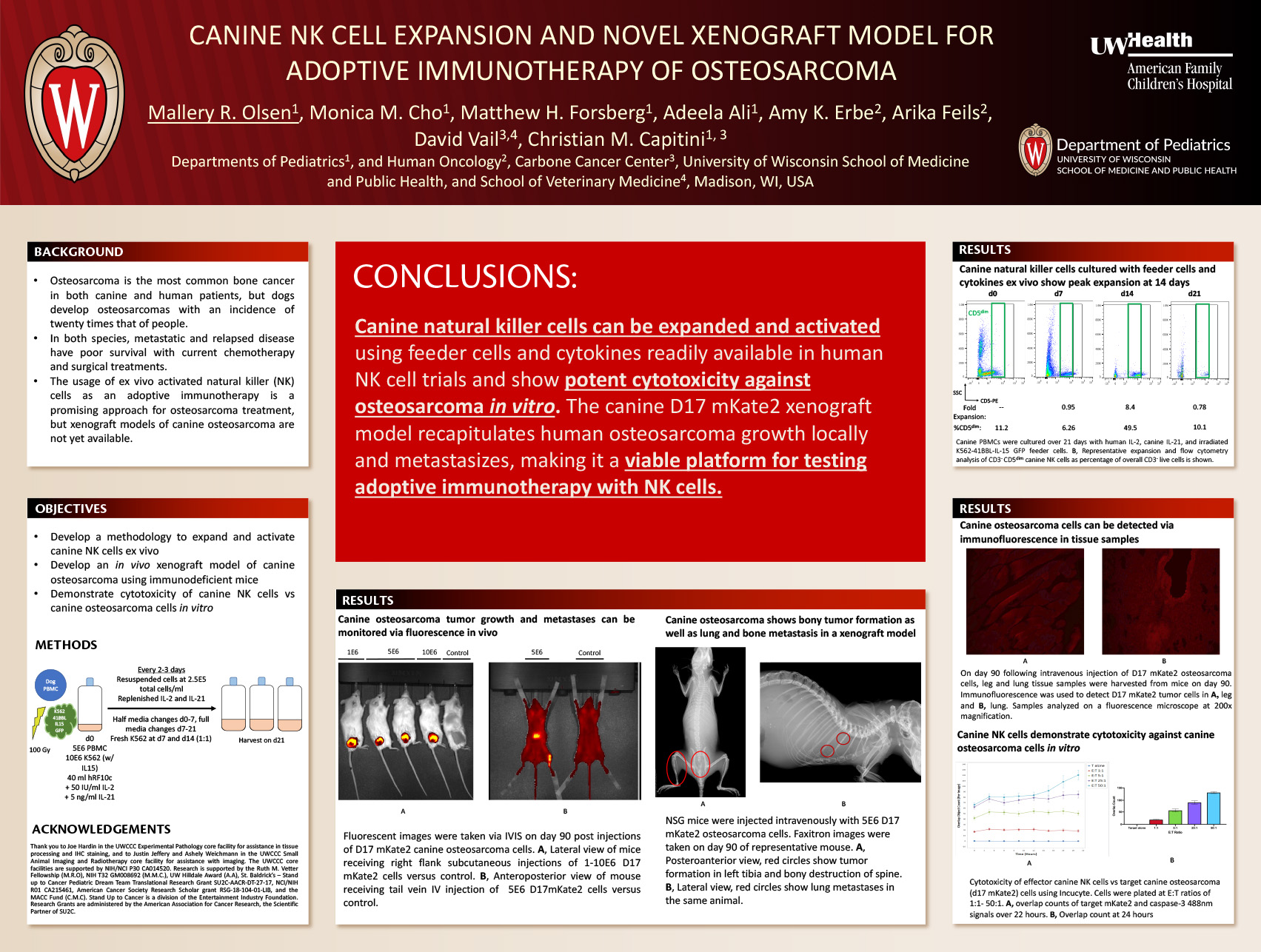
CANINE NK CELL EXPANSION AND NOVEL XENOGRAFT MODEL FOR ADOPTIVE IMMUNOTHERAPY OF OSTEOSARCOMA
Click here for .pdf version of poster
Authors: Mallery R. Olsen1, Monica M. Cho1, Matthew H. Forsberg1, Adeela Ali1, Amy K. Erbe2, Arika Feils2, David Vail3,4, Christian M. Capitini1,4
Departments of Pediatrics1, and Human Oncology2, Carbone Cancer Center3, University of Wisconsin School of Medicine and Public Health, and School of Veterinary Medicine4, Madison, WI, USA
Background:
Osteosarcoma is the most common bone cancer in both canine and human patients, but dogs develop osteosarcomas with an incidence of twenty times that of people; thus dogs are an ideal model for studying therapies for pediatric osteosarcoma treatment. In both species, metastatic and relapsed disease have poor survival with current chemotherapy and surgical treatments. The usage of ex vivo activated natural killer (NK) cells as an adoptive immunotherapy is a promising approach for osteosarcoma treatment, but xenograft models of canine osteosarcoma are not yet available.
Objectives:
The objective of this study was to develop a methodology to expand and activate canine NK cells ex vivo, characterize their function against a canine osteosarcoma cell line in vitro, and develop an in vivo xenograft model of canine osteosarcoma using immunodeficient mice.
Design/Methods:
Peripheral blood from healthy dogs was collected, and peripheral blood mononuclear cells (PBMCs) were isolated by Ficoll. PBMCs were co-cultured with irradiated K562-41BBL-IL15 GFP feeder cells. Human IL-2 and canine IL-21 were added to NK cultures and repleted with fresh media every 2-3 days. Every 7 days, irradiated feeder cells were added. Flow cytometry was done every 7 days to enumerate CD3-CD5dim canine NK cells. Following 14-21 days of culture, cells were isolated by fluorescence activated cell sorting. The canine osteosarcoma cell line D17 was transduced to express mKate2 (D17 mKate2) and evaluated in an NK cytotoxicity assay using Incucyte. D17 mKate2 cells were also injected subcutaneously as a xenograft into NSG mice, and tumors were followed by digital caliper as well as immunohistochemistry (IHC), IVIS, X-ray, and CT imaging.
Results:
While canine NK cells only were expanded up to 8.6 fold using 41BBL/IL15/IL21/IL2 stimulation over 21 days, they showed high cytotoxicity in vitro at 25-50:1 ratios against D17 mKate2 osteosarcoma cells within 24 hours. In vivo, for the first time we show a dose response curve of establishing D17 mKate2 osteosarcoma in NSG mice using 1 x 106 – 10 x 106 cells. Tumor growth was confirmed by both IVIS and IHC. Metastatic disease was confirmed using x-ray and micro computerized tomography (microCT).
Conclusion:
Canine NK cells can be expanded and activated using feeder cells and cytokines that are readily available for human NK cell trials, and show potent cytotoxicity against osteosarcoma in vitro. The canine D17 mKate2 xenograft model recapitulates human osteosarcoma growth locally and metastasizes, making it a viable platform for testing adoptive immunotherapy with NK cells.
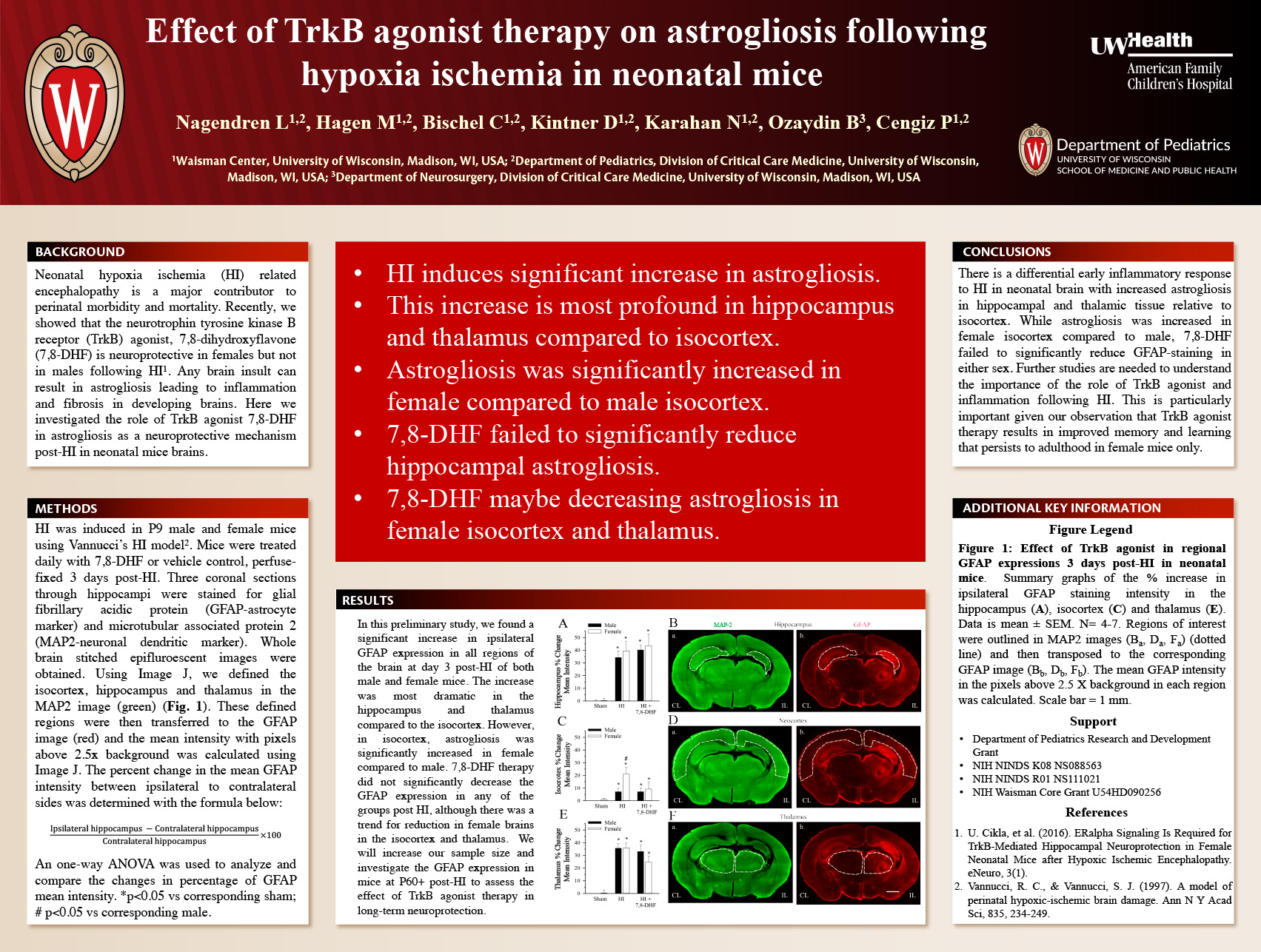
Effect of TrkB agonist therapy on astrogliosis following HIE in mice
Click here for .pdf version of poster
Nagendren L1,2, Hagen M1,2, Bischel C1,2, Kintner D1,2, Karahan N1,2, Ozaydin B3, Cengiz P1,2
1Waisman Center, University of Wisconsin, Madison, WI, USA; 2Department of Pediatrics, Division of Critical Care Medicine, University of Wisconsin, Madison, WI, USA; 3Department of Neurosurgery, Division of Critical Care Medicine, University of Wisconsin, Madison, WI, USA
Background: Neonatal hypoxic-ischemic encephalopathy (HIE) is a major contributor to perinatal morbidity and mortality. Following HIE, astrocytes undergo morphological changes, and secrete proteins that modulate the neuroinflammatory process. Recently, we showed that the nerve growth factor tyrosine kinase receptor (TrkB) agonist, 7,8-dihydroxyflavone (7,8-DHF) following neonatal HIE provides long-term neuroprotection to females but not males. However, the mechanism of this neuroprotection through glia or neuron is unknown.
Objective: To determine whether the TrkB agonist-7,8-DHF mediated neuroprotection following HIE is due to modulation of astrogliosis.
Methods: HIE was induced in P9 C57BL/6J male and female mice by using Vannucci’s HI model. Mice were treated either with the TrkB agonist-7,8-DHF or vehicle control following HIE. Three days following HIE, mice were perfusion fixed, and the brains were sliced and stained using immunohistochemistry for glial fibrillary acid protein (GFAP)-reactive astrocyte marker and microtubular associated protein (MAP-2)-dendritic marker. The MAP2 image was used to define the isocortex, hippocampus and thalamus regions (Fig. 1). The percent change in mean GFAP intensity of ipsilateral (IL) to contralateral (CL) sides was quantified using ImageJ.
Results: Despite an increase in hippocampal GFAP expression post-HI of both male and female mice, 7,8-DHF therapy did not reduce the GFAP expression in the hippocampus of wither sex (Fig 1). 7,8-DHF therapy reduced the HIE-induced GFAP expression in female isocortex. GFAP expression equally increased post-HI in the thalamus of males and females, however, the 7,8- DHF treatment reduced GFAP expression more in female than the male mice.
Conclusion: TrkB agonist therapy might be decreasing the astrogliosis in certain regions of the brain following HIE in a sexually differential way. Further studies are needed to understand the importance of the role of TrkB agonist in decreasing astrogliosis. This is particularly important given our observation that TrkB agonist therapy results in improved memory and learning only in female mice that persists to adulthood.
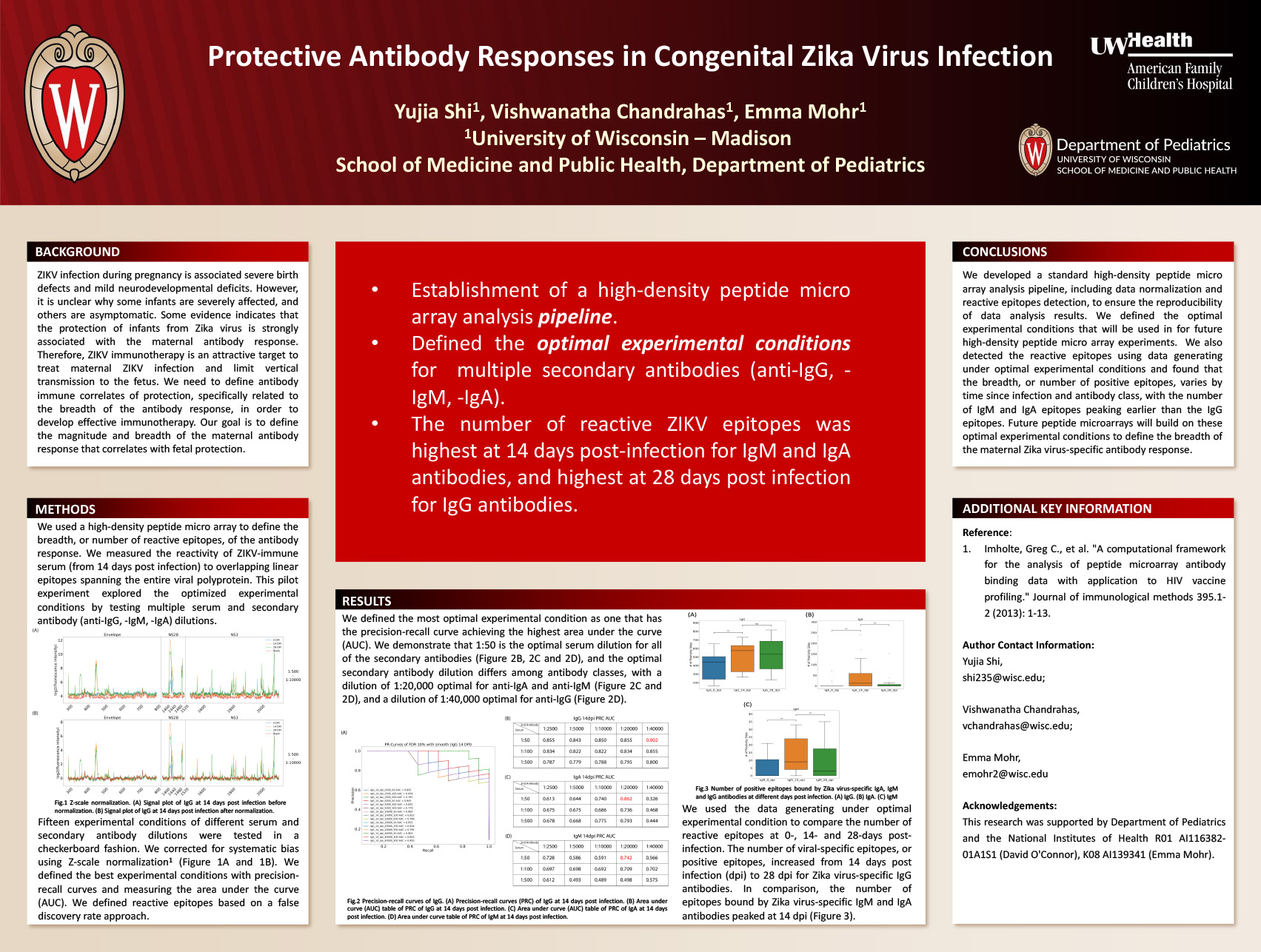
Protective Antibody Responses in Congenital Zika Virus Infection
Click here for .pdf version of poster
Yujia Shi1, Vishwanatha Chandrahas2, Emma Mohr2
1Department of Biostatistics & Medical Informatics
2Department of Pediatrics
Background
Zika virus infection during pregnancy is associated severe birth defects and mild neurodevelopmental deficits. It is unclear why some infants are severely affected and others are asymptomatic. Because the maternal antibody response is associated with protection, we must define characteristics of a protective antibody response for future development of ZIKV immunotherapy.
Objective
Define how the breadth of the maternal antibody response is associated with control of viral infection, specific duration of maternal viremia during pregnancy. Our first objective is to develop a high throughput assay to measure the number of viral epitopes following Zika virus infection during pregnancy.
Design/Methods
We defined Zika virus specific linear epitopes spanning the entire viral polyprotein with a highdensity peptide micro array and serum from a Zika virus-infected macaque. In this pilot experiment, we defined the optimal experimental conditions, taking into consideration serum dilution and concentrations of secondary antibodies targeting multiple antibody classes (IgG, IgM, IgA). We tested 15 experimental conditions of different serum and secondary antibody dilutions in a checkerboard fashion. We defined the best experimental conditions with precision-recall curves and measuring the area under the curve (AUC). We defined reactive epitopes based on a false discovery rate approach.
Results
We validated the performance of Z-scale normalization with our data set (Fig.1). We demonstrate that the best experimental condition is a 1:50 serum dilution (Fig. 2). We also show that the optimal secondary antibody dilution differs between antibodies, with a dilution of 1:20,000 optimal for anti-IgG and anti-IgA (Fig. 2), and a dilution of 1:40,000 for anti-IgM (Fig. 3). The number of viral-specific epitopes, or positive epitopes, increased from 14 days post infection (dpi) to 28 dpi for Zika virus-specific IgG antibodies. In comparison, the number of epitopes bound by Zika virus-specific IgM and IgA antibodies peaked at 14 dpi (Fig.4).
Conclusion
We defined the optimal experiment conditions that will be used in for future high throughput peptide microarray experiments. We found that the breadth, or number of positive epitopes, varies by time since infection and antibody class, with the number of IgM and IgA epitopes peaking earlier than the IgG epitopes. Future peptide microarrays will build on these optimal experimental conditions to define the breadth of the maternal Zika virus-specific antibody response.
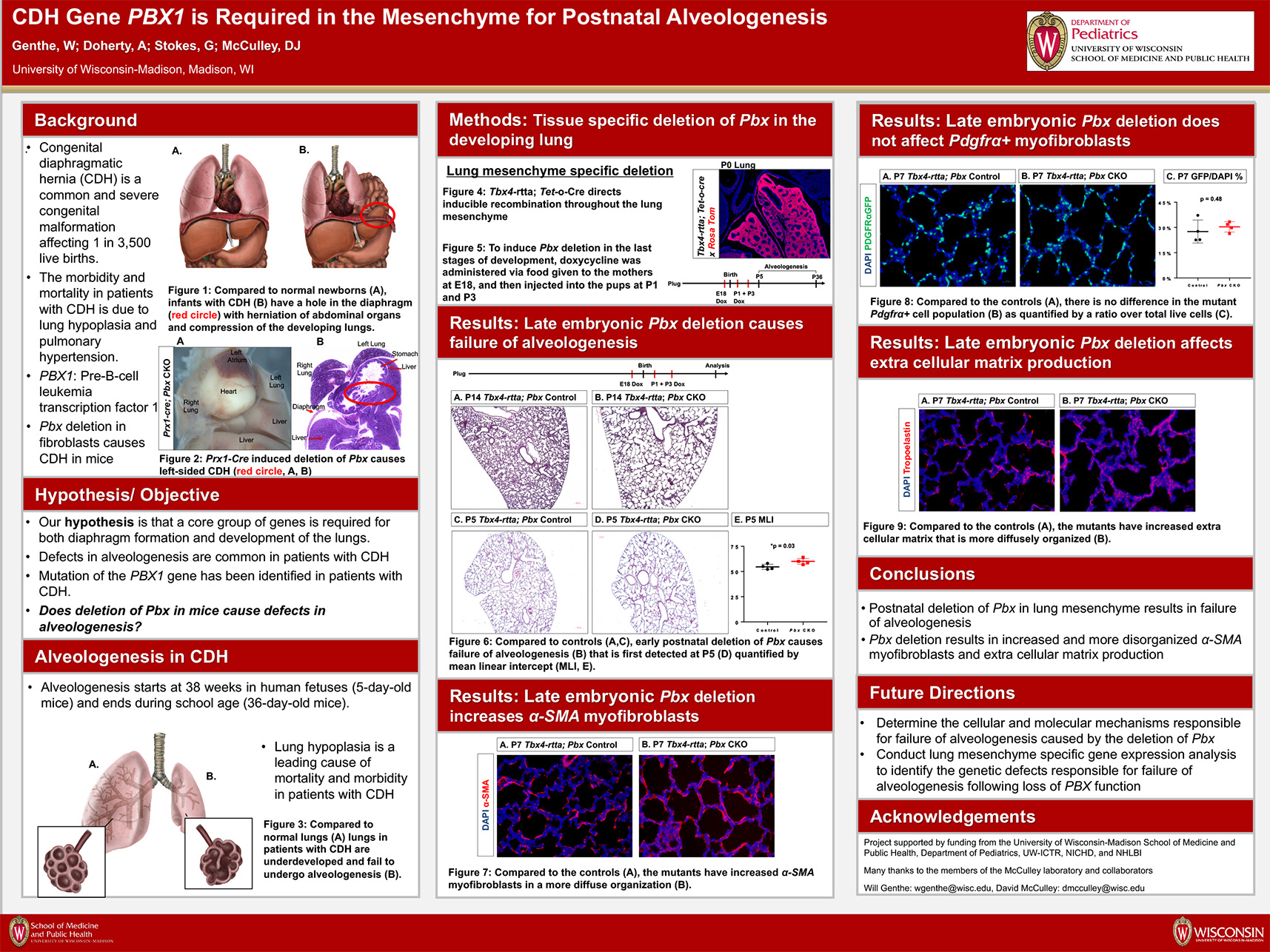
CDH Gene PBX1 is Required in the Mesenchyme for diaphragm formation and Postnatal Alveologenesis
Click here for .pdf version of poster
Authors: William H. Genthe; Ashley L. Doherty; Gia M. Stokes; David J. McCulley
Background: Congenital diaphragmatic hernia (CDH) is a common and severe congenital malformation, affecting 1 in 3500 live births with a mortality rate of 20-50%. The cause of the high mortality rate in patients with CDH is due to underdevelopment of the lungs. To improve the survival of patients and protect their lungs, great care is taken to reduce exposure to mechanical ventilation and supplemental oxygen in the newborn period. Although these measures have improved the survival of patients with CDH, postnatal lung development remains abnormal. The cause of this failure of postnatal lung development remains unclear. Our hypothesis is that mutations in genes that cause abnormal diaphragm development, seen in patients with CDH, also play a direct role in the cellular and molecular mechanisms required for postnatal alveologenesis. Mutations in the PBX1 gene were recently reported in patients with CDH. In mice, Pbx1 is required for diaphragm formation and lung-specific deletion of Pbx1 causes failure of postnatal alveologenesis. The cellular and molecular mechanisms responsible for these defects remain unclear.
Objective: To identify the molecular and cellular mechanisms responsible for failure of alveologenesis in Pbx1 mutant mice.
Design/Methods: Using a cell-specific, conditional gene deletion, we inactivated the expression of Pbx1 in the developing lung mesenchyme and myofibroblast progenitor cells. We used a combination of histology and gene expression analysis to analyze the mutant phenotype.
Results: Deletion of Pbx1 in the lung mesenchyme resulted in failure of alveologenesis, abnormal extracellular matrix formation, and impaired epithelial and endothelial cell populations. Deletion of Pbx1 in the alveolar myofibroblasts did not cause defects in alveologenesis.
Conclusion(s): Mutations in the PBX1 gene result in human CDH. Independent of its role in the diaphragm, Pbx1 is required in the lung for postnatal alveologenesis, alveolar capillary development, and organization of the extracellular matrix. Pbx1 is not required in the alveolar myofibroblasts suggesting that a different population of mesenchymal precursor cells require Pbx1 expression to direct alveologenesis.
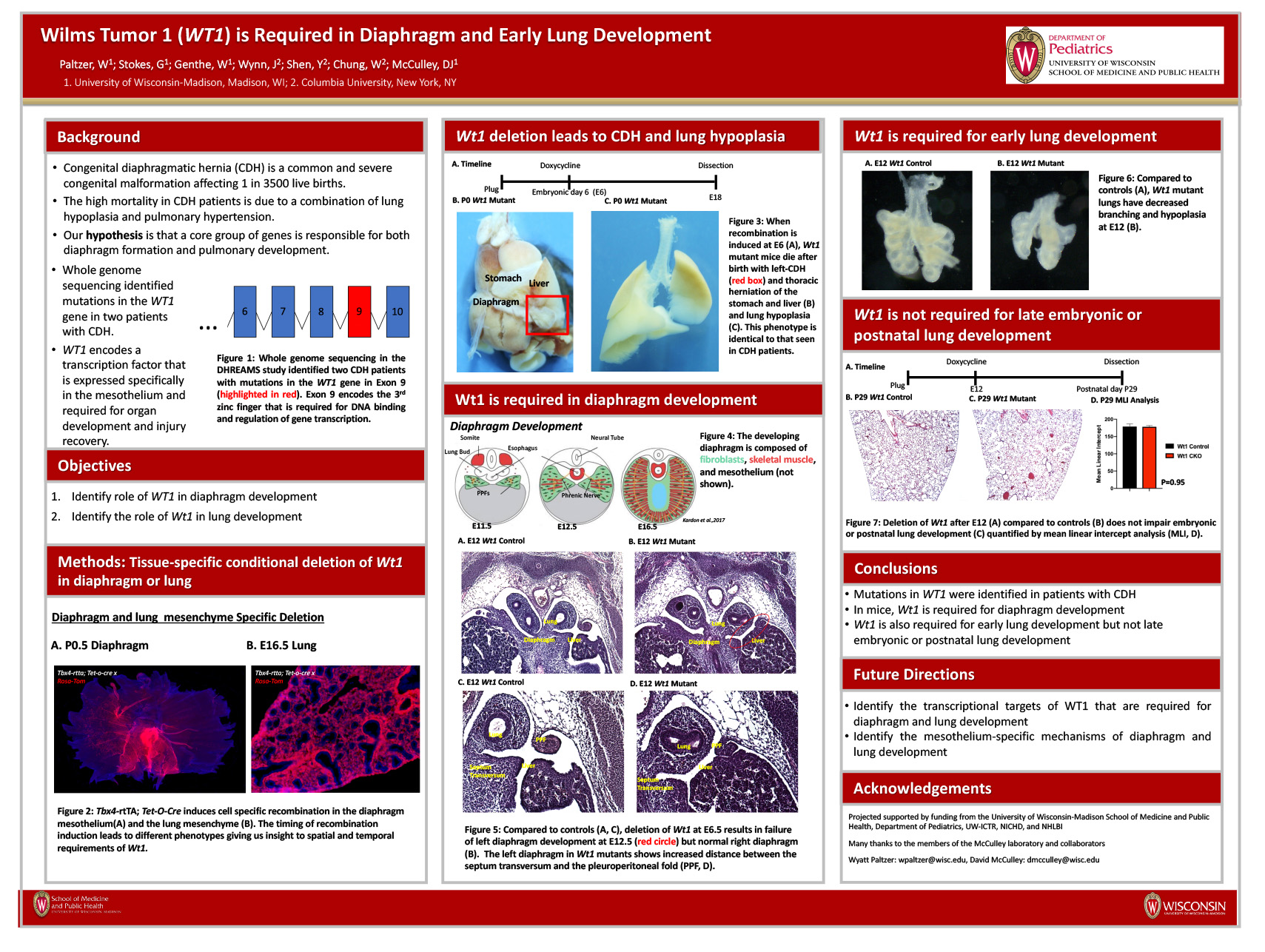
Wt1 mutations cause congenital diaphragmatic hernia and lung defects in humans and mice
Click here for .pdf version of poster
AUTHORS (Last name, First name): Paltzer, Wyatt G.1, Stokes, Giangela M.1, Genthe, William1, McCulley, David J.1
INSTITUTIONS:
- University of Wisconsin-Madison, Madison, WI, United States
Background: Congenital diaphragmatic hernia (CDH) is a common and severe congenital malformation, affecting 1 in 3500 live births with a mortality rate between 20-50%. The high mortality rate in CDH patients is due to improper lung development leading to decreased lung function. The severity of CDH varies from patient to patient and its developmental origins are unclear. We hypothesize that CDH is the result of genetic mutations that cause improper development of the diaphragm. The same genetic mutation may also impair lung development causing lung hypoplasia and pulmonary hypertension. Using whole genome sequencing in human patients, WT1 was recently implicated as a candidate CDH disease causing gene. Preliminary data in mice models supports this; however, the mechanism through which Wt1 mutations cause CDH is not yet understood.
Objective: To determine the role of Wt1 in the developing diaphragm and lung mesenchyme and elucidate the mechanisms through which CDH and lung phenotypes arise following Wt1 loss of function.
Design/Methods: Using cell-specific genetic recombination, we generated mice that lack Wt1 function in the developing diaphragm mesothelium and lung mesenchyme. We then used histological, immunofluorescent, and gene expression analysis to examine the requirement and function of Wt1.
Results: Deletion of Wt1 in the developing diaphragm mesothelium leads to CDH with failure of the left side of the diaphragm to close and herniation of the abdominal organs into the fetal thorax. This failure to close is due to the pleuroperitoneal fold and septum transversum failing to fuse. Additionally, Wt1 mutant mice have lung hypoplasia; however, it is unclear if this phenotype is due to the loss of function of Wt1 in the developing lung or due to a mechanical compression caused by the herniated abdominal organs.
Conclusions: Mutations in WT1 were identified in patients with CDH. Tissue-specific deletion of Wt1 in mice resulted in left-CDH and improper development of the pleuroperitoneal fold and septum transversum. These data demonstrate that normal development of the mesothelium is required for diaphragm formation.
Session B: Social Media and Advocacy – Blackboard Collaborate Session
This is an accordion element with a series of buttons that open and close related content panels.
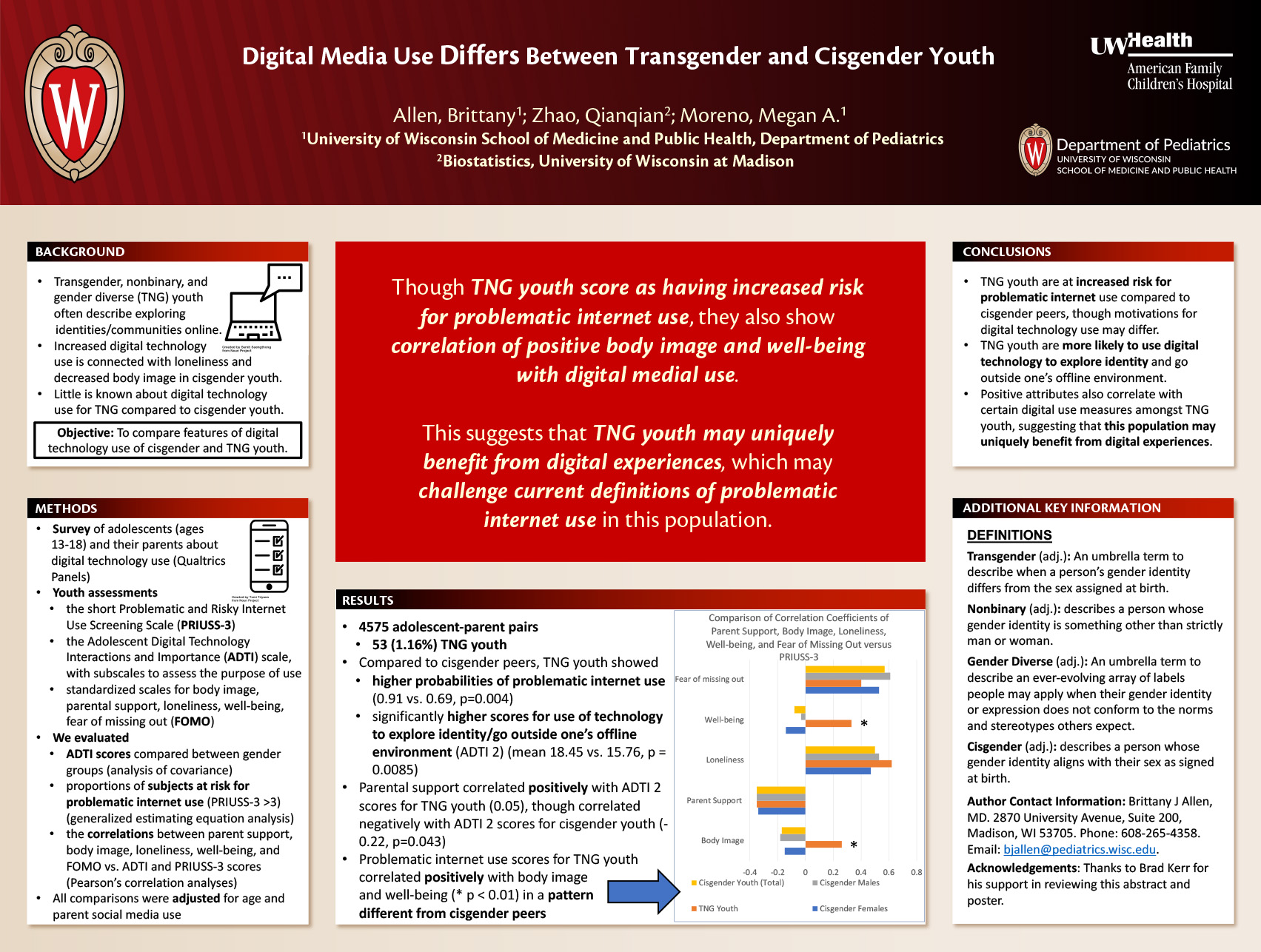
Digital Media Use Differs Between Transgender/Nonbinary Youth and Cisgender Peers
Click here for .pdf version of poster
AUTHORS: Allen, Brittany1; Zhao, Qianqian2; Moreno, Megan A.3
INSTITUTIONS:
1. Pediatrics, University of Wisconsin School of Medicine and Public Health, Madison, WI, United States.
2. Biostatistics, University of Wisconsin at Madison, Madison, WI, United States.
3. Pediatrics, University of Wisconsin Madison, Madison, WI, United States.
Background: Transgender, nonbinary, and gender diverse (TNG) youth often describe exploring identities and communities online. Studies of cisgender youth connect increased digital technology use with loneliness and decreased body image. Little is known about digital technology use for TNG compared to cisgender youth.
Objective: To compare features of digital technology use of cisgender and TNG youth.
Design/Methods: Using Qualtrics panels, we surveyed a nationally representative sample of adolescents (ages 13-18) and their parents about digital technology use. Youth assessment included the Adolescent Digital Technology Interactions and Importance (ADTI) scale, with subscales assessing the purpose of technology use, and the short Problematic and Risky Internet Use Screening Scale (PRIUSS-3).
Validated instruments also assessed body image, parental support, loneliness, well-being, fear of missing out (FOMO), and parent social media use. We compared ADTI scores between gender groups with analysis of covariance. Generalized estimating equation (GEE) analysis was conducted to compare the proportions of subjects at risk for problematic internet use (PRIUSS-3 >3). All comparisons were adjusted for age and parent social media use. Pearson’s correlation analyses evaluated the correlations between parent support, body image, loneliness, well-being, and FOMO vs. ADTI and PRIUSS-3 scores.
Results: Among 4575 adolescent-parent pairs, there were 53 (1.16%) TNG youth. TNG youth had significantly higher scores for use of technology to explore identity/go outside one’s offline environment (ADTI 2) compared to cisgender youth. Parent support correlated positively with ADTI 2 scores for TNG youth (0.05), though correlated negatively with ADTI 2 scores for cisgender youth (-0.22, p=0.043). TNG youth showed higher probabilities of problematic internet use than cisgender peers (0.91 vs. 0.69, p=0.004). Problematic internet use scores for TNG youth correlated positively with body image and well- being in a pattern different from cisgender peers.
Conclusion(s): TNG youth are at increased risk for problematic internet use compared to cisgender peers, though motivations for digital technology use may differ. TNG youth were more likely to use digital technology to explore identity and go outside one’s offline environment. Positive attributes also correlated with certain digital use measures amongst TNG youth, suggesting that this population may uniquely benefit from digital experiences.
Investigating differences in adolescent technology use and mental health outcomes
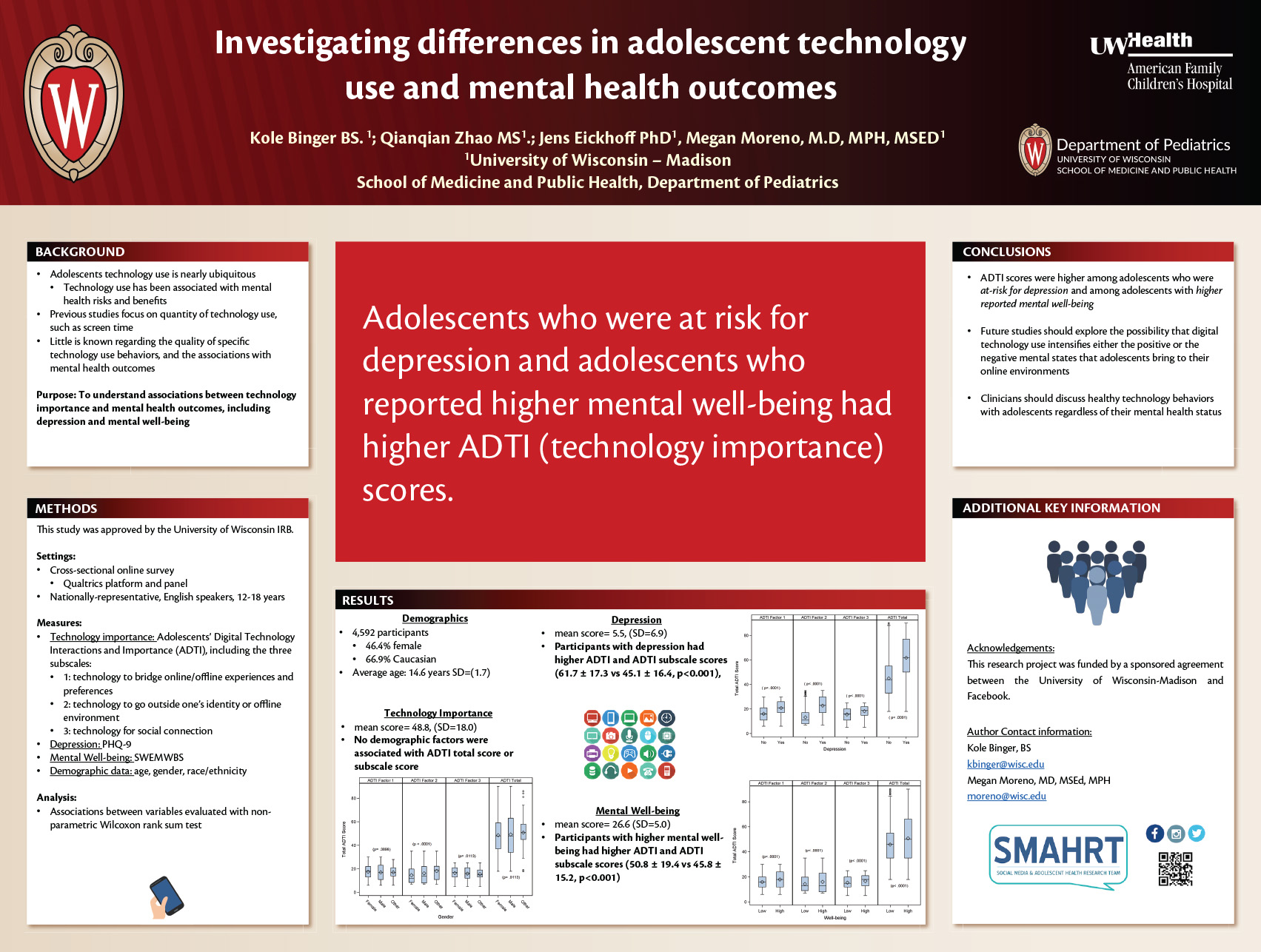
Authors: Kole Binger, Qianqian Zhao, Jens Eickhoff, Megan Moreno
Category: Social Media and Technology
Keywords: Adolescent Health, Mental Health, Well-being
Investigating differences in adolescent technology use and mental health outcomes
Adolescents’ technology use is associated with mental health risks, such as decreased mood, and benefits including social connection. Previous studies that assess technology use and mental health outcomes focus on quantity of technology use. However, little is known regarding the quality of specific technology use behaviors, and how they are associated with mental health outcomes.
The purpose of this study was to understand associations between technology use behaviors and mental health outcomes, including depression and mental well-being.
We recruited a nationally-representative sample of English speaking adolescents, aged 12-18 years, to a cross-sectional online survey using the Qualtrics platform and panels. Technology use behaviors were measured via Adolescents’ Digital Technology Interactions and Importance (ADTI) scale; the three ADTI subscales include: 1) technology to bridge online/offline experiences and preferences, 2) technology to go outside one’s identity or offline environment, 3) technology for social connection. Mental health measures included depression (via the Patient Health Questionnaire 9 [PHQ-9]) and mental well-being (via the Warwick-Edinburgh Mental Well-being Scale [WEMWBS]). Demographic data included age, gender and race. Associations between variables were evaluated using a non-parametric Wilcoxen Rank Sum test.
Of our 4,592 participants, 46.4% were female, 66.9% were Caucasian and the average age was 14.6 years (SD= 1.7). The mean ADTI total score was 48.8 (SD=18.0), mean PHQ-9 score was 5.5 (SD=6.9) and mean WEMWBS sum was 26.6 (SD=5.0). No demographic factors were associated with the ADTI total score. Participants who met criteria for depression had higher ADTI total scores (61.7 ± 17.3 vs 45.1 ± 16.4, p<0.001), as well as higher scores for each ADTI subscale. Participants with higher mental well-being also had higher total ADTI (50.8 ± 19.4 vs 45.8 ± 15.2, p<0.001), as well as higher ADTI subscale scores. Figures 1-3 illustrate these findings.
We found that ADTI scores were higher among adolescents who screened positive for depression. However, we found that ADTI scores were also higher among adolescents with higher reported well-being. Future studies should explore the possibility that digital technology use intensifies either the positive or the negative mental states that adolescents bring to their online environments.
Management of Pediatric Isolated Bicuspid Aortic Valve: Current Practice Survey
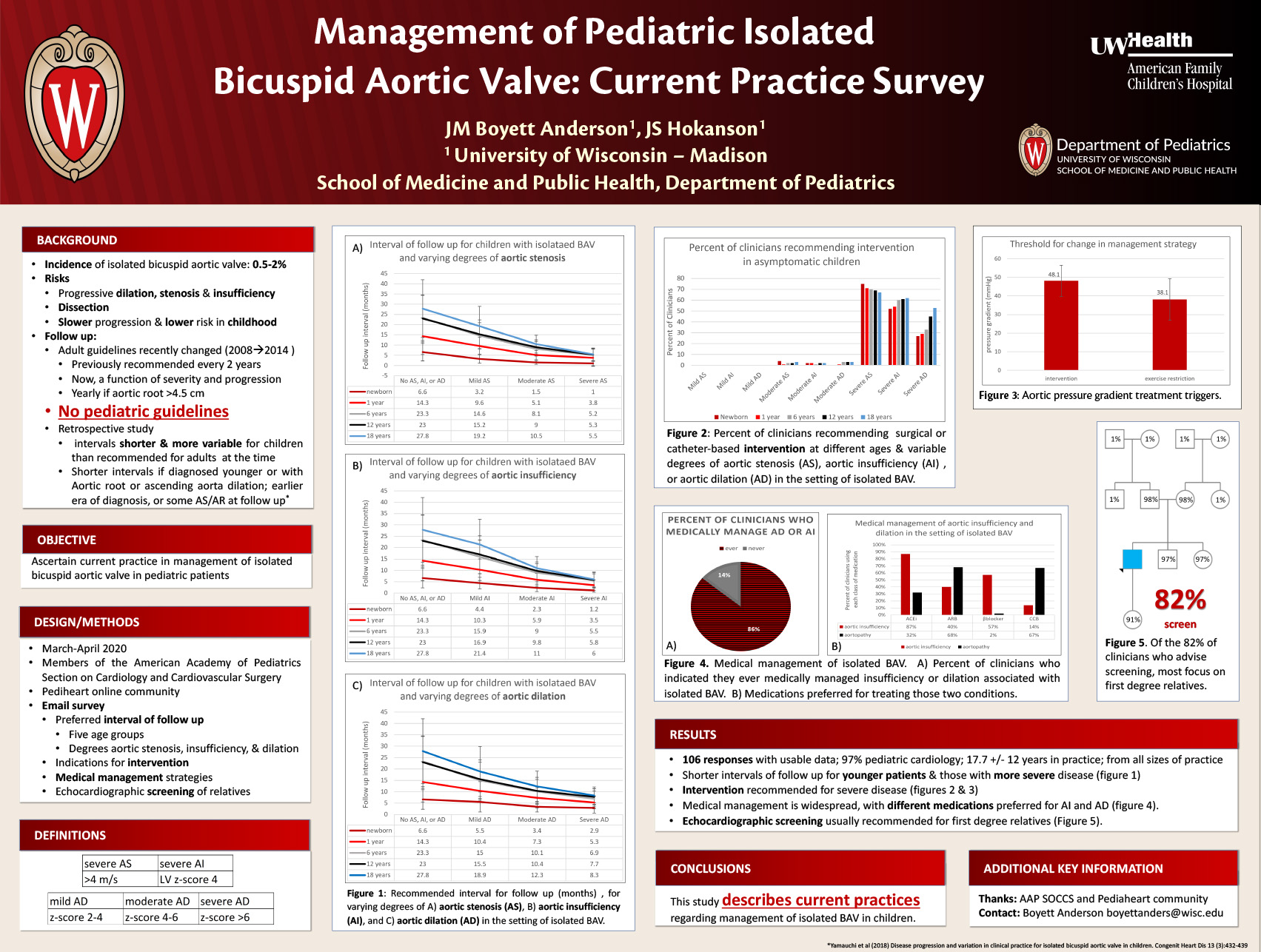
Click here for .pdf version of poster
Jesse Boyett Anderson, MD, John Smith Hokanson, MD
Background: Although formal guidelines exist for routine follow-up of adult patients with a bicuspid aortic valve (BAV), no such guidelines exist for children.
Objective: This survey was performed to determine current practice in the management of pediatric BAV.
Methods: Members of the American Academy of Pediatrics Section on Cardiology and Cardiovascular Surgery and the Pediheart online community were surveyed regarding their preferred interval of follow up and their management of patients under 18 years old with an isolated BAV and varying degrees of stenosis, regurgitation and aortic dilation. For simplicity, no combinations of stenosis, insufficiency and aortic dilation were included.
Results: We received 82 responses with interpretable data.
For patients with isolated BAV without stenosis, insufficiency, or aortic dilation, follow-up-intervals increased from an average of 7+/-4 months in the newborn period to 29 +/- 15 months at 18 years of age. Respondents recommended more frequent follow up for patients at younger ages and with greater disease severity (see tables 1-3). In general, intervention was recommended once stenosis or insufficiency became severe (stenosis of >4 m/s; LV Z score 4) regardless of age, but was not routinely recommended for younger children (newborn – age 6 years) with severe dilation (see table 4).
Respondents recommended intervention (either surgical or catheter) at an echo mean gradient of 49+/-9 mm Hg, with gradual increase from newborn to 18-years-of age, and recommended exercise restrictions at an echo mean gradient of 39+/-12 mm Hg. More than 80% of respondents treat aortic insufficiency or aortic dilation in the setting of bicuspid aortic valve medically, with angiotensin converting enzyme inhibitors (80%) being the preferred medication for insufficiency and angiotensin receptor blockers (70%) and beta blockers (65%) being preferred for aortic dilation.
81% of respondents recommended family members of patients (including parents (97%), siblings (97%), and children (94%), grandparents (2%) or aunts/uncles (2%)) have echocardiographic evaluation.
Conclusion:This study provides a snapshot of current practices regarding follow up of BAV in children. Although available data suggests limited progression of aortic stenosis, aortic regurgitation, and aortopathy through childhood and adolescence in children with an isolated BAV, current practice is to follow up with these children more frequently than recommended in adults.
Understanding adolescent and parent news media consumption patterns
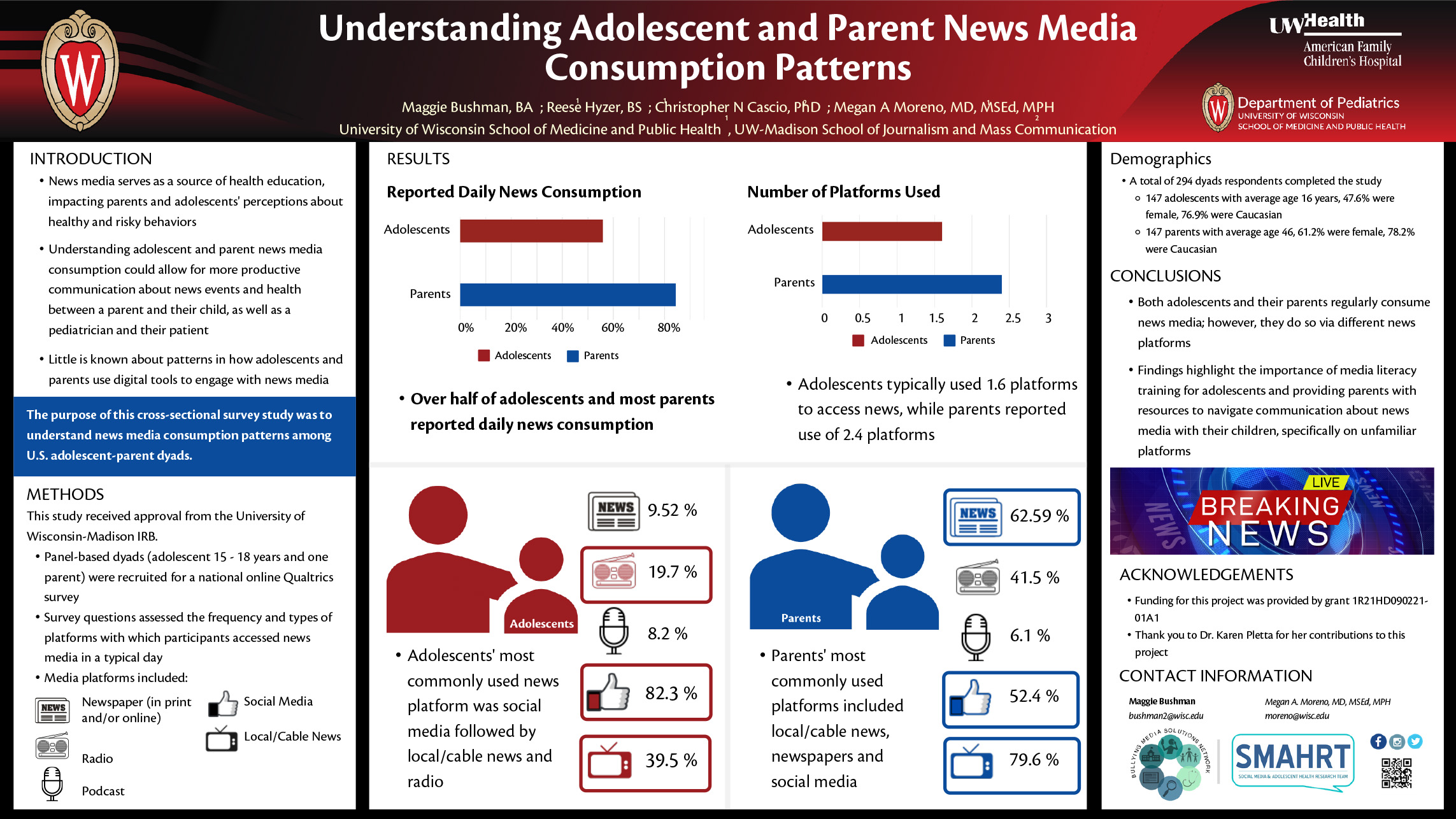
Click here for .pdf version of poster
AUTHORS: Maggie Bushman, BS; Reese Hyzer, BS;
Christopher N Cascio, PhD; Megan A Moreno, MD, MSEd, MPH
POSSIBLE CATEGORIES: Social Media and Technology
POSSIBLE KEY WORDS: news media, adolescent health, parents
_____________________________________________________________________________________
TITLE (67): Understanding adolescent and parent news media consumption patterns
BACKGROUND (476):
News media serves as a source of health education, impacting adolescents’ knowledge about healthy and risky behaviors such as exercise or vaping. Understanding adolescent and parent news media consumption could allow for more productive communication about news events and health between a parent and their child, as well as a pediatrician and their patient. Little is known about patterns in how adolescents and parents use digital tools to engage with news media.
OBJECTIVE (134):
The purpose of this cross-sectional survey study was to understand news media consumption patterns among U.S. adolescent-parent dyads.
METHODS (489):
We recruited panel-based dyads, including one adolescent age 15-18 years and one parent, for a national online Qualtrics survey. Survey questions assessed the frequency with which participants accessed news media in a typical day. Participants were asked to indicate all media platforms on which they accessed news media including newspaper (in print and/or online), radio, podcast, social media, and local/cable news. Descriptive statistics were summarized as frequencies and percentages.
RESULTS (744):
Among our 294 dyad respondents, adolescent participants’ (n=147) 47.6% were female and 76.9% were Caucasian; mean age was 16 (SD=0.99). Parent participants’ (n=147) 61.2% were female and 78.2% were Caucasian; mean age was 46 (SD=8.4). Over half of adolescents (55.7%) and most parents (85.5%) reported daily news consumption. Adolescents typically used 1.6 (SD=0.8) platforms to access news media, while parents reported use of 2.4 (SD=1) platforms. Adolescents’ most commonly used news platform was social media, with 82.3% of teens reporting this platform. Other news platforms included local/cable news (39.5%), and radio (19.7%). Parents’ most commonly used news platforms included local/cable news (79.6%), newspapers (62.59%), and social media (52.4%; see Table 1).
CONCLUSION (306):
Findings suggest both adolescents and their parents regularly consume news media, however, they do so via different news platforms. These findings highlight the importance of media literacy training for adolescents and providing parents with resources to navigate communication about news media with their children, specifically on unfamiliar news platforms.
Adolescents' and Parents' Perceptions of News Media and Bullying Experiences
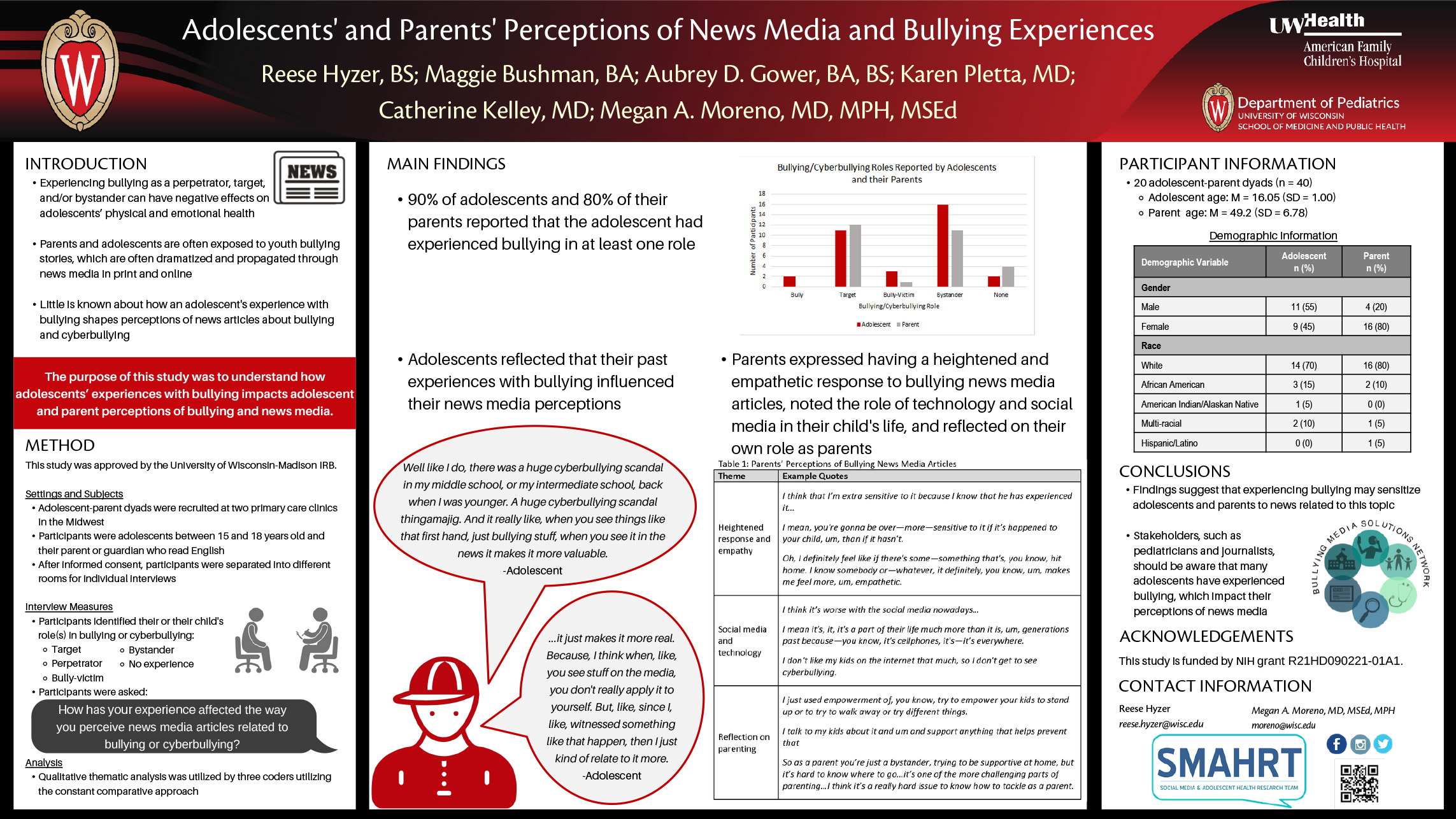
Click here for .pdf version of poster
AUTHORS: Reese H. Hyzer, Maggie E. Bushman, Aubrey D. Gower, Karen Pletta, Catherine Kelley, Megan A. Moreno
Experiencing bullying as a perpetrator, target, and/or bystander can have negative effects on adolescents’ physical and emotional health. Both adolescents and parents are often exposed to news media about youth bullying, often online including social media. However, little is known about how an adolescent’s previous experience with bullying shapes perceptions of news articles on bullying and cyberbullying.
The purpose of this study was to understand how adolescents’ experiences with bullying impacts adolescent and parent perceptions of bullying and news media.
Participants were recruited from two Midwest pediatric clinics; adolescents between the ages of 15 and 18 and their accompanying parents were eligible. Participant dyads completed private, semi-structured interviews in separate rooms, which assessed whether the adolescent had ever experienced bullying as a target, perpetrator, bully-victim (i.e., target and perpetrator), bystander, or had no experience with bullying. Participants were then asked about how these experiences impacted their perceptions of bullying and news media. Interviews were audio recorded and transcribed verbatim. Qualitative analysis used the constant comparative method with three researchers to identify themes.
A total of 20 adolescent-parent dyads were interviewed (n=40). Adolescents were 45% female, 70% Caucasian, with an average age of 16 (SD=0.9) years, and parents were 80% female, 80% Caucasian, with an average age of 49.2 (SD=6.7) years. The majority of adolescents (90%) endorsed experience with bullying, with 80% identifying as a bystander and 55% as a target. Most parents (87%) reported that their child had experience with bullying, with 41% identifying them as a target and 41% as a bystander. Adolescents reflected that their past experiences with bullying influenced their news media perceptions. One adolescent said, “It just makes it more real…Since I, like witnessed something like that happen, then I just kind of relate to it more.” Parents noted heightened sensitivity to news media related to this topic, as well as reflected on the role of technology and parenting. Example quotes from parents are in Table 1.
Findings suggest that experiencing bullying may sensitize adolescents and parents to news related to this topic. Stakeholders, such as pediatricians and journalists, should be aware that many adolescents have experienced bullying, which impact their perceptions of news media.
News Media Bullying Articles Impact Parent and Adolescent Emotions
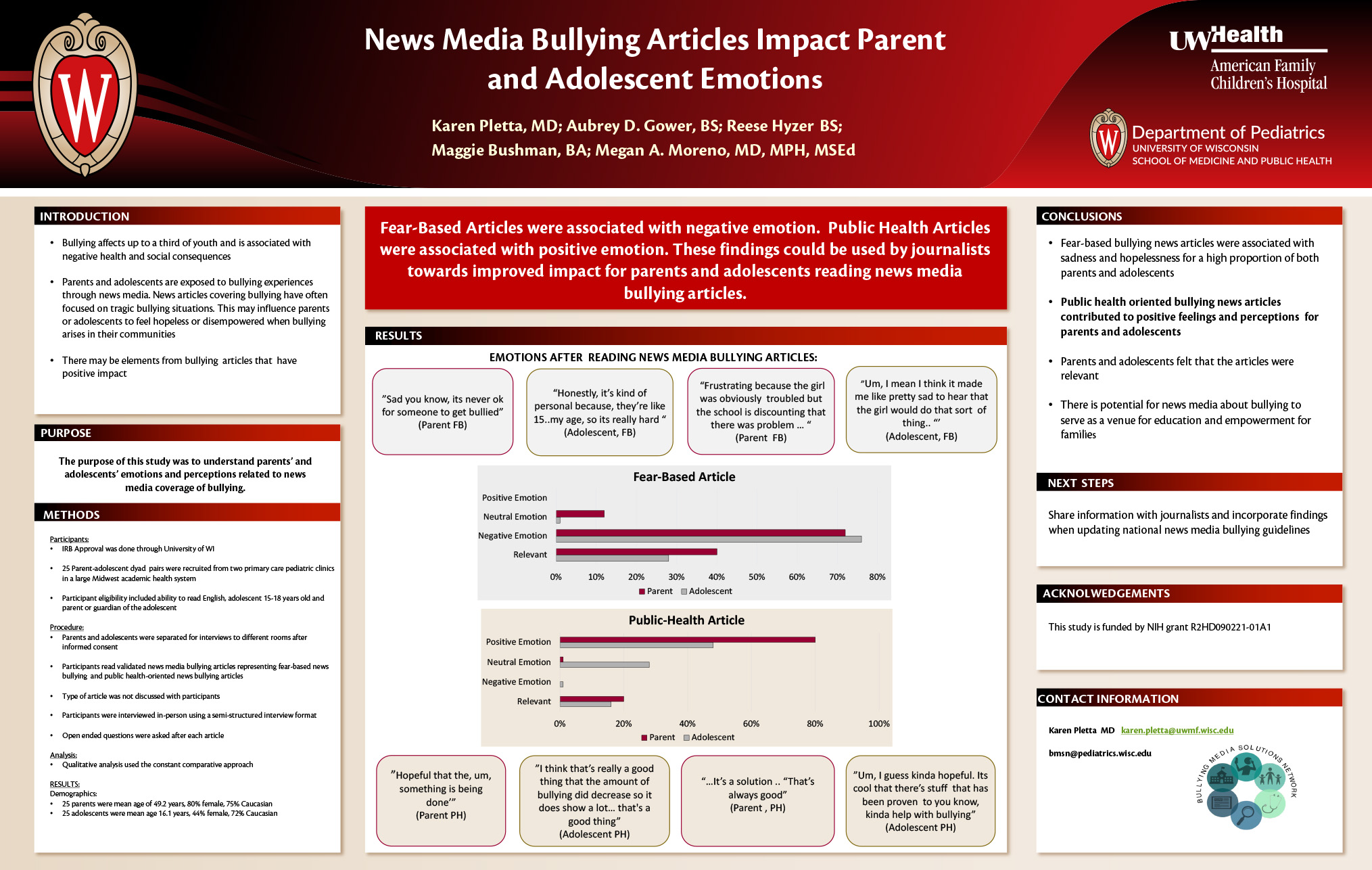
Click here for .pdf version of poster
AUTHORS (LAST NAME, FIRST NAME): Pletta, Karen1; Gower, Aubrey D.4; Hyzer, Reese2; Bushman, Maggie3; Moreno, Megan A.3
INSTITUTIONS (ALL): 1. University of Wisconsin Madison, Stoughton, WI, United States.
2. Pediatrics, University of Wisconsin-Madison, Madison, WI, United States.
3. Pediatrics, University of Wisconsin Madison, Madison, WI, United States.
4. School of Medicine, University of Washington , Seattle, WA, United States.
Background: Bullying affects up to a third of youth and is associated with negative health and social consequences. Parents and adolescents are exposed to bullying experiences through news media with approximately 84% of parents and 55% of adolescents reporting daily news consumption. News articles covering bullying have commonly focused on individual, often tragic bullying situations. These types of stories may influence parents and adolescents to feel hopeless or disempowered when bullying arises in their communities.
Objective: The purpose of this qualitative study was to understand parents’ and adolescents’ emotions and perceptions related to news media coverage of bullying and cyberbullying.
Design/Methods: Participants were recruited from two primary care pediatric clinics in a large Midwest academic health system. Participants were interviewed in-person using semi-structured interview format. During interviews, participants read two validated examples of news media bullying articles that represented a fear-based news bullying article and a public health-oriented news bullying article. Participants were asked open ended questions after reading each article. Qualitative analysis used the constant comparative approach.
Results: Our 50 participants included 25 parents with mean age of 49.2 years, were 80% female and 76% Caucasian. Our 25 adolescent participants had mean age of 16.1 years, were 44% female and 72% Caucasian. Both parents and adolescents described their emotions after reading the articles along a negative-positive spectrum. After reading fear-based articles, 18 parents (72%) and 19 adolescents (76%) responded that they felt negatively. An example quote of negative emotion was “honestly, it’s kind of personal because, they’re like 15..my age…so it’s really hard”. For public-health oriented articles, 20 parents (80%) and 12 adolescents (48%) felt positively. A positive emotion example quote was “I feel really good”. A total of 26 (51%) participants described the news articles as relatable to their lives or experience.
Conclusion: Our data support that reading fear-based bullying news articles was associated with feelings of sadness and hopelessness for a high proportion of both parents and adolescents. Parents and adolescent participants often described public health-oriented news articles as contributing to positive feelings and perceptions. These findings support the potential of news media about bullying to serve as a venue for education and empowerment for families.
Speaker Gender Representation at Pediatric Academic Society Meeting
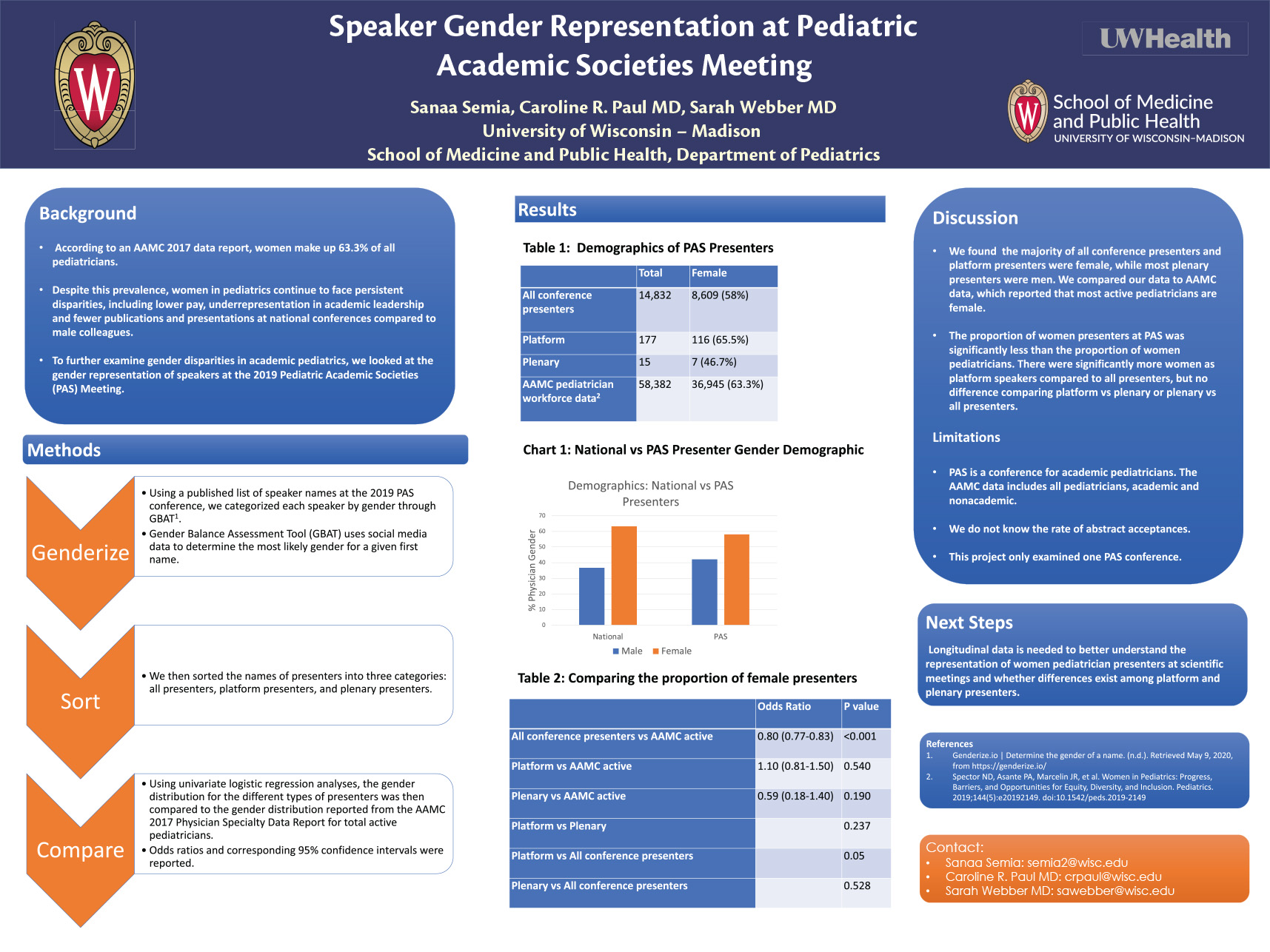
Authors: Sanaa Semia, Caroline R. Paul MD, Sarah Webber MD
Background
According to an AAMC 2017 data report, women make up 63.3% of all pediatricians. Despite this prevalence, women in pediatrics continue to face persistent disparities, including lower pay, underrepresentation in academic leadership and fewer publications and presentations at national conferences compared to male colleagues.
Objective
To identify the gender make up of speakers at the 2019 Pediatric Academic Societies (PAS) conference.
Methods
Using the published list of speakers at the Pediatric Academic Societies conference, we categorized speaker type by gender using the Gender Balance Assessment Tool (GBAT). GBAT is a validated web-based tool that uses the genderize.io algorithm and social media data to assign a first name a probability of belonging to a gender. The first name of the author was entered into the database, which provides the most likely gender (male or female) and the probability that the determination is correct. Next, we sorted the names of presenters to create three lists: all presenters, plenary presenters and platform presenters.
The gender distribution for the different types of presenters were compared to the gender distribution reported from the AAMC 2017 Physician Specialty Data Report for pediatric total active physicians using univariate logistic regression analyses. Odds ratios and the corresponding 95% confidence intervals were reported.
Results
Table 1 demonstrates the demographics of 2019 PAS presenters. There were 14,832 total PAS presenters (8609, 58% women), 177 platform presenters (n=116, 65.5% women) and 15 plenary presenters (n=7, 46.7% women). The proportion of women presenters was lower compared to total active pediatricians as defined by the AAMC (58% vs 65.5%, OR 0.8, p<0.001); there was no significant difference in the proportion of platform or plenary speakers compared to active pediatricians (Table 2). Comparing types of presenters, there were significantly more women as platform speakers compared to all presenters (p=0.05), but no difference comparing platform vs plenary or plenary vs all presenters.
Simplified Needs Assessment for Global School Health: A Pilot Approach
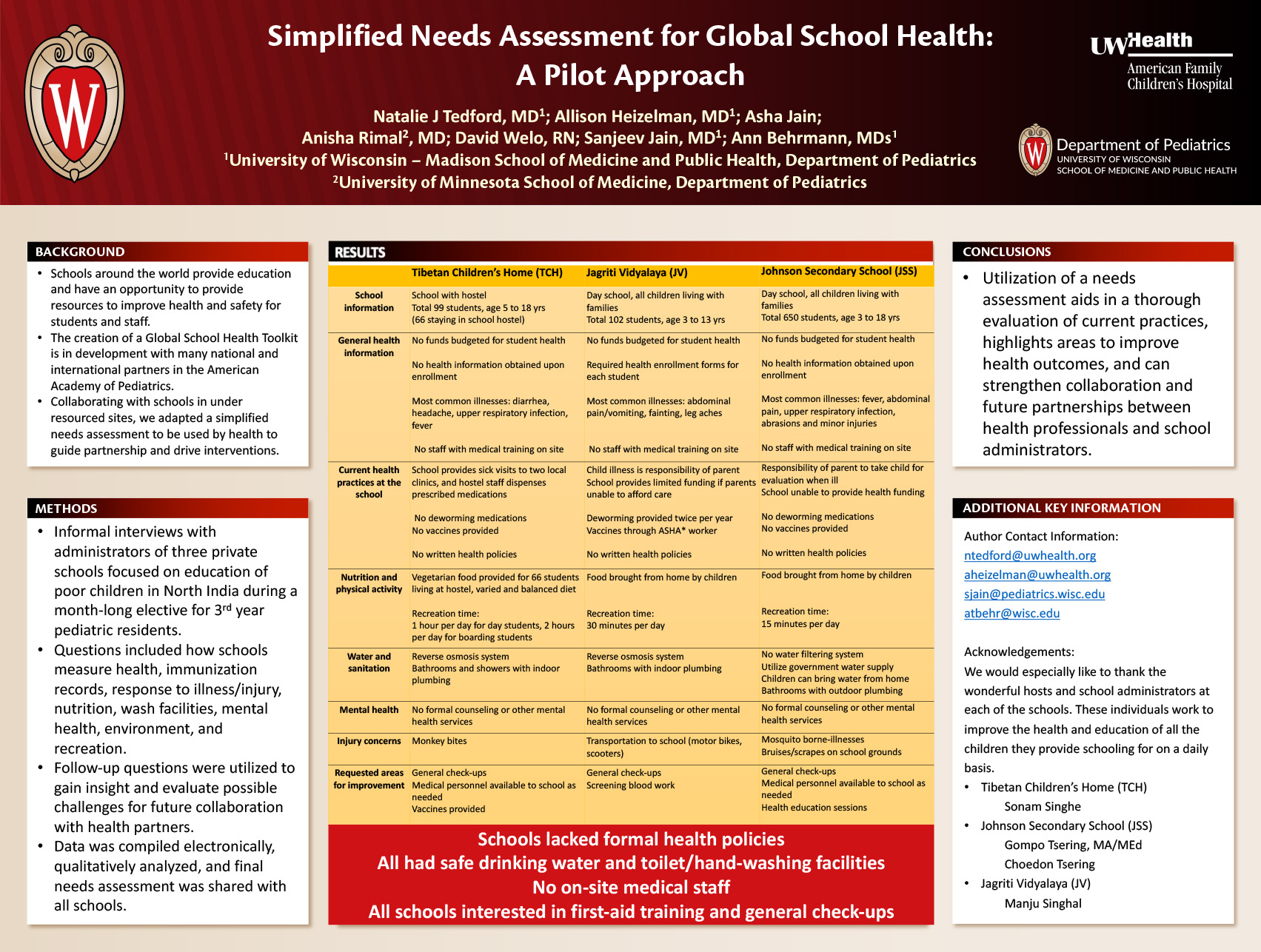
Click here for .pdf version of poster
Authors:
Tedford, Natalie J.; Heizelman, Allison; Jain, Asha; Rimal, Anisha; Welo, David; Jain, Sanjeev; Behrmann, Ann
Background:
In addition to education, schools around the world have an opportunity to provide resources to improve health and safety for students and staff. As part of the development of a Global School Health Toolkit, we adapted a simplified needs assessment to be used by health professionals collaborating with schools in under resourced sites to guide this partnership.
Objective:
Pilot a Global School Health needs assessment draft with school administrators by UWHealth pediatricians partnering with three schools in Uttarakhand, India.
Methods:
Informal interviews with administrators of three private schools focused on education of poor children in North India during a month-long elective for 3rd year pediatric residents. Questions included how schools measure health, immunization records, response to illness/injury, nutrition, wash facilities, mental health, environment, and recreation. Follow-up questions were utilized to gain insight and evaluate possible challenges for future collaboration with health partners. Data was compiled electronically, qualitatively analyzed, and final needs assessment was shared with all schools.
Results:
Schools differed in size (two at 100, one with 650 students) and grade levels. All included preschool up to grade 5, and the larger school to grade 10. One included a boarding component for 66 children with vegetarian meals. No school had a formal health policy, and only one collected immunization/health records on admission and provided antiparasitic on site. All had safe drinking water and toilet/hand-washing facilities. Abdominal pain, diarrhea/vomiting, upper respiratory infection, and minor injuries were common in all three. None had onsite medically trained staff but were interested in staff first aid training.
Conclusions:
Utilization of a needs assessment aids in a thorough evaluation of current practices, highlights areas to improve health outcomes, and can strengthen collaboration and future partnerships between health professionals and school administrators.
Mapping Advocacy Education with a CATCH Visiting Professorship
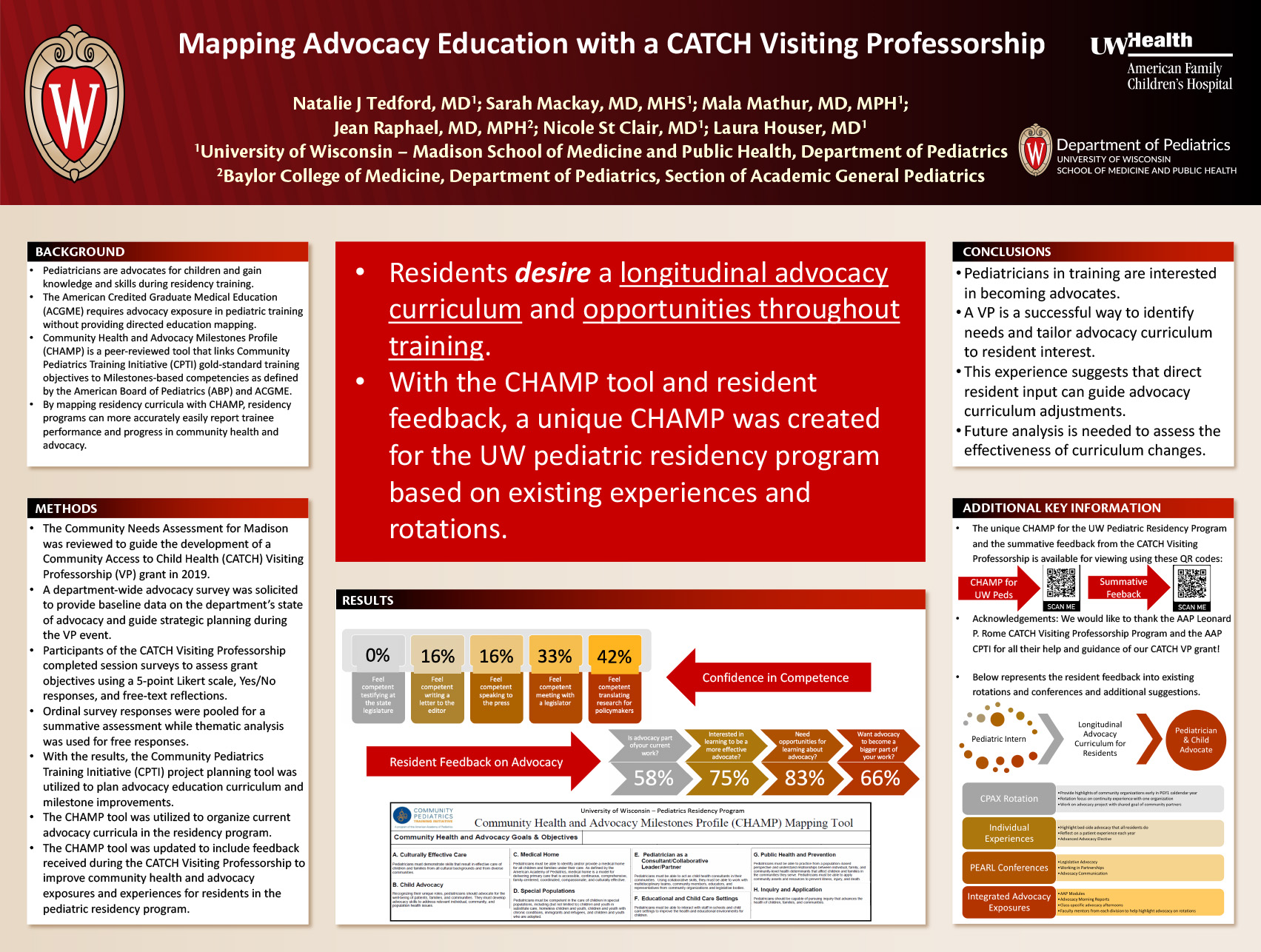
Click here for .pdf version of poster
Authors: Natalie Tedford, MD, Sarah MacKay, MD, MHS, Mala Mathur, MD, MPH, Nicole St Clair, MD, & Laura Houser, MD
Background:
Pediatricians are advocates for children and gain knowledge and skills during residency training. The American Credited Graduate Medical Education (ACGME) requires advocacy exposure in pediatric training without providing directed education mapping.
Objective:
Map advocacy education and incorporate resident feedback to promote sustainable, longitudinal engagement
Methods:
The Community Needs Assessment for a Midwest city served by a tertiary care university children’s hospital and mid-size pediatric residency program was reviewed to guide the development of a Community Access to Child Health (CATCH) Visiting Professorship (VP) grant in 2019. A department-wide advocacy survey was solicited to provide baseline data on the department’s state of advocacy and guide strategic planning during the VP event. Participants completed session surveys to assess grant objectives using a 5-point Likert scale, Yes/No responses, and free-text reflections. Ordinal survey responses were pooled for a summative assessment while thematic analysis was used for free responses. With the results, the Community Pediatrics Training Initiative (CPTI) project planning tool was utilized to plan advocacy education curriculum and milestone improvements.
Results:
Out of 45 pediatric residents, 27% completed the department advocacy survey with the majority incompetent in 5 various forms of advocacy and indicating the need/desire for additional advocacy training. With 62% of residents completing session evaluations during the CATCH VP, 96% were satisfied engaging with community partners during the VP to discuss advocacy education. The summative assessment of the described grant objective demonstrated 85% completeness. Qualitatively, residents enjoyed interacting with community partners and desire a longitudinal advocacy curriculum and opportunities throughout training. Three themes emerged: increased community connection, hopefulness for advocacy education, inspired advocacy efforts. With the CPTI Child Health and Advocacy Milestones Profile (CHAMP) mapping tool and resident feedback, a unique CHAMP was created for the program based on existing experiences and rotations.
Conclusions:
Pediatricians in training are interested in becoming advocates. A VP is a successful way to identify needs and tailor advocacy curriculum to resident interest. This experience suggests that direct resident input can guide advocacy curriculum adjustments. Future analysis is needed to assess the effectiveness of curriculum changes.
Does Rotation Service Assignment Affect the Teaching Experience and Knowledge Gained for Medical Students during their Core Pediatric Clerkship?
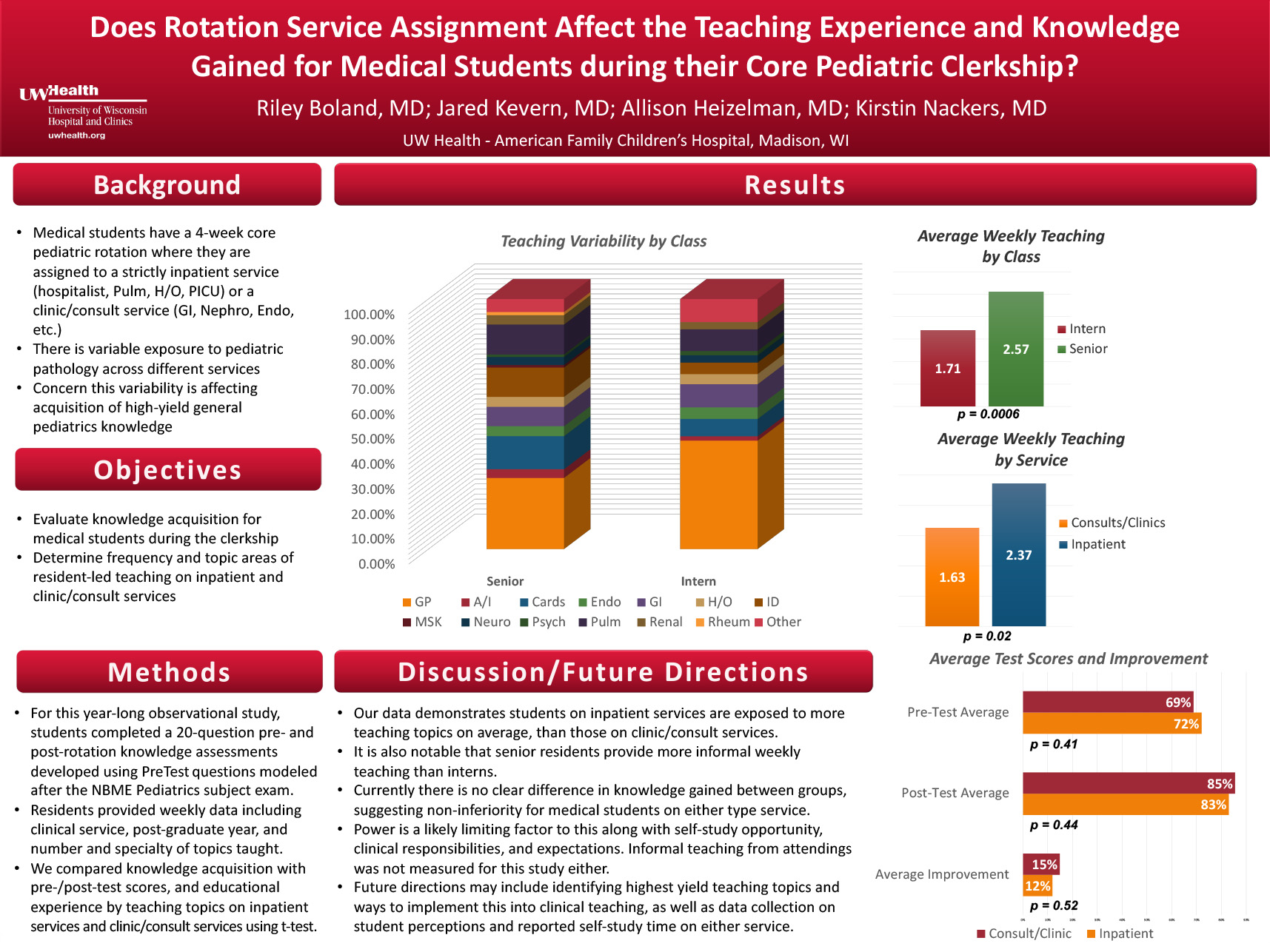
Click here for .pdf version of poster
Riley S Boland, MD; Jared Kevern, MD; Allison Heizelman, MD; Kirstin Knackers, MD
UW Health – American Family Children’s Hospital, Madison, WI
Background:
Medical students have a 4-week core pediatric rotation where they are assigned to a strictly inpatient service (Hospitalist, Pulm, H/O, PICU) or a clinic/consult service (GI, Nephro, Endo, etc.). There is variable exposure to pediatric pathology across different services. Therefore there is concern this variability is affecting acquisition of high-yield general pediatrics knowledge.
Objectives:
To evaluate knowledge acquisition for medical students during the clerkship, and to determine the frequency and topic areas of resident-led teaching on inpatient and clinic/consult services.
Methods:
For this year-long observational study, students completed a 20-question pre- and post-rotation knowledge assessments developed using PreTest questions modeled after the NBME Pediatrics subject exam. Residents provided weekly data including clinical service, post-graduate year, and number and specialty of topics taught. We compared knowledge acquisition with pre-/post-test scores, and educational experience by teaching topics on inpatient services and clinic/consult services using t-test.
Results:
Review of pre- and post-test data demonstrates no significance for score improvement when comparing inpatient services vs clinic/consult services (12% vs 15%, p=0.52). Residents on an inpatient service taught more on average per week than the residents on clinic/consult services (2.4 vs 1.6, p=0.0006). Senior residents also taught more than interns per week (2.6 vs 1.7, p=0.02).
Discussion:
Our data demonstrates students on inpatient services are exposed to more teaching topics on average, than those on clinic/consult services. It is also notable that senior residents provide more informal weekly teaching than interns. There is also a seemingly increased variability on topics taught between senior and intern residents. Currently there is no clear difference in knowledge gained between groups, suggesting non-inferiority for medical students on either type service. Power is a likely limiting factor to this along with self-study opportunity, clinical responsibilities, and expectations. Informal teaching from attendings was not measured for this study either. Future directions may include identifying highest yield teaching topics and ways to implement this into clinical teaching, as well as data collection on student perceptions and reported self-study time on either service.
Session C: Quality Improvement – Blackboard Collaborate Session
This is an accordion element with a series of buttons that open and close related content panels.
Identifying opportunities to improve the care of children with Kawasaki Disease in concordance with national guidelines
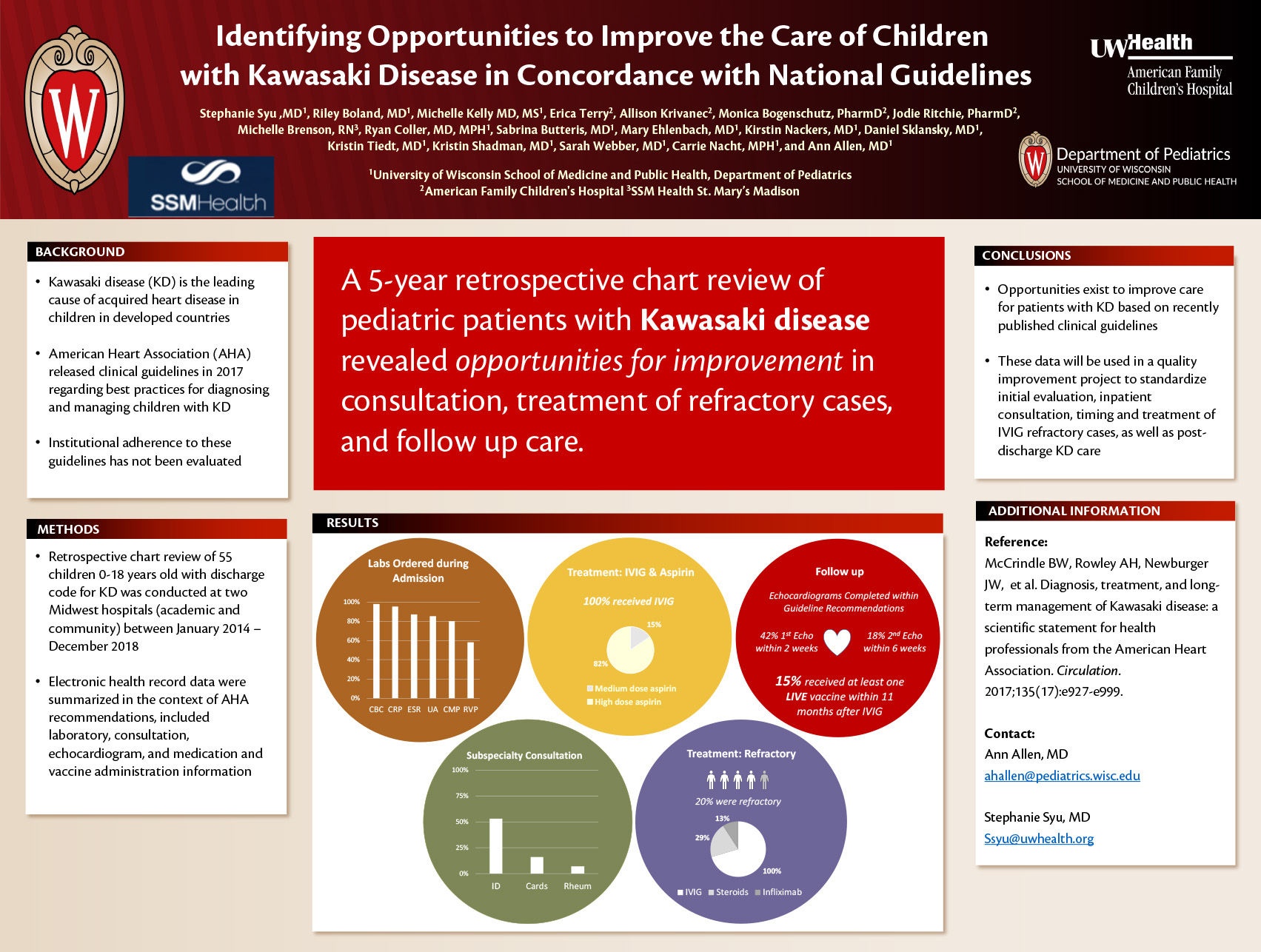
Click here for .pdf version of poster
Ann Allen MD1, Riley Boland MD1, Stephanie Syu MD1, Erica Terry2, Allison Krivanec2, Monica Bogenschutz PharmD2, Jodie Ritchie PharmD2, Michelle Brenson RN3, Ryan Coller MD, MPH1, Sabrina Butteris MD1, Mary Ehlenbach MD1, Kirstin Nackers MD1, Daniel Sklansky MD1, Kristin Tiedt MD1, Kristin Shadman MD1, Sarah Webber MD1, Carrie Nacht MPH1, and Michelle Kelly MD, MS1
1Department of Pediatrics, University of Wisconsin School of Medicine and Public Health
2UW Health – American Family Children’s Hospital
3SSM Health St. Mary’s Madison
Background: Kawasaki disease (KD) is the leading cause of acquired heart disease among children in developed countries. The American Heart Association (AHA) released clinical guidelines in 2017 regarding best practices for diagnosing and managing children with KD. Institutional adherence to these guidelines has not been evaluated.
Objective: Assess concordance with AHA guidelines regarding diagnostic evaluation, treatment and follow up for children admitted with KD.
Methods: Retrospective chart review of children 0-18 years old with discharge code for KD was conducted at two Midwest hospitals (academic and community) between January 2014-December 2018. Electronic health record data were summarized in the context of AHA recommendations, included laboratory, consultation, echocardiogram, and medication and vaccine administration information.
Results: During the five year period, 55 children were admitted with complete or incomplete KD with a median (IQR) age of 2.5 (1.5-4.0) years. In all, 54 (98%) had a complete blood cell count, 52 (95%) C-reactive protein, 48 (87%) erythrocyte sedimentation rate, 47 (85%) urinalysis, 44 (80%) complete metabolic panel and 32 (58%) a respiratory viral panel. Infectious disease, cardiology and rheumatology consults occurred in 53%, 16% and 7%, respectively. All received guideline-recommended 2g/kg Intravenous Immunoglobulin (IVIG) initial therapy and 53 (96%) received moderate to high dose aspirin during admission. Eleven (20%) were considered IVIG refractory and all received a second dose of IVIG; a small proportion received steroids (29%) or infliximab (13%). Median (IQR) time to discharge after IVIG completion was 33 (25-39) hours. After discharge, only 23 (42%) had their first follow up echocardiogram within the recommended 2 weeks and (18%) had their second within 6 weeks. Eight (15%) however received at least one live vaccine within 11 months of IVIG administration.
Conclusion: Opportunities exist to improve care for patients with KD based on recently published clinical guidelines. These data will be used in a quality improvement project to standardize initial evaluation, inpatient consultation, timing and treatment of IVIG refractory cases, as well as post-discharge KD care.
Improving Asthma Action Plan Completion Rates via Utilization of Epic Best Practice Advisory
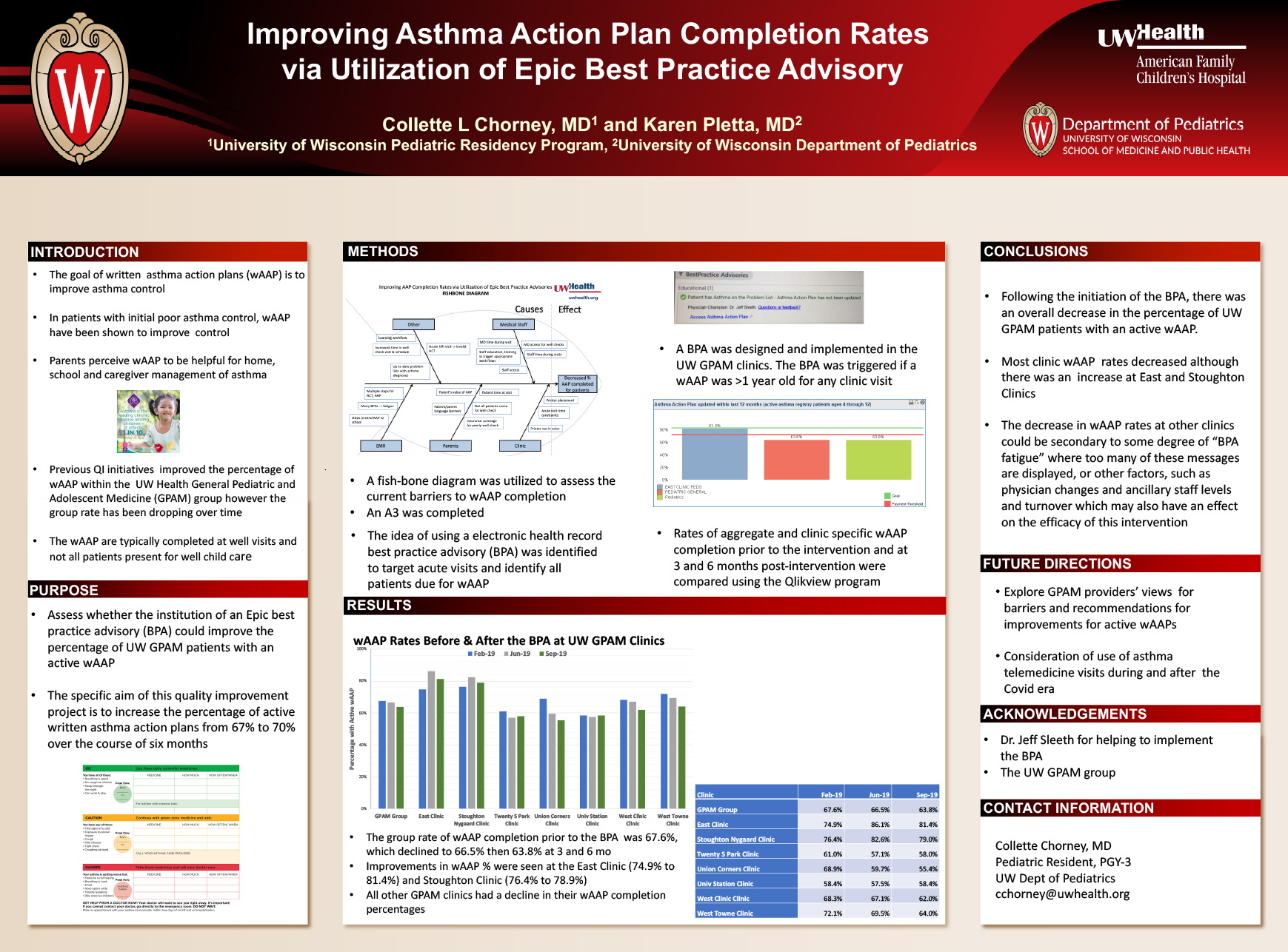
Click here for .pdf version of poster
Authors: Collette L. Chorney, MD1 and Karen L. Pletta, MD2
Affiliations: 1University of Wisconsin Pediatric Residency Program; 2University of Wisconsin Department of Pediatrics
Background: Written asthma action plans (wAAP) are recommended for pediatric patients with the goal of improving asthma control. In patients with initial poor asthma control, wAAP have been shown to improve asthma control. In addition, parents perceive wAAP to be helpful for home, school and caregiver management of asthma. Previous quality improvement initiatives have improved the percentage of wAAP within the General Pediatric and Adolescent Medicine (GPAM) group. As of 9/2018, wAAP levels levels had decreased and had been stable for three months, suggesting there is room for further improvement. The wAAP are typically completed at well visits and not all patients present for well child care.
Objectives: This quality improvement project was to assess whether the institution of an Epic best practice advisory (BPA) could improve the percentage of UW GPAM patients with an active wAAP. The specific aim of this quality improvement project is to increase the percentage of written asthma action plans from 67% to 70% over the course of six months.
Methods: As part of the quality improvement process, a fish-bone diagram was utilized to assess the current barriers to wAAP completion. The idea of using a BPA to target acute visits and identify those due for wAAP at well checks was identified. An A3 was completed. A BPA was designed and implemented in the UW GPAM clinics. The BPA was triggered if a wAAP was >1 year old. Rates of aggregate and clinic specific wAAP completion prior to the intervention and at 3 and 6 months post-intervention were compared.
Results: The aggregate rate of wAAP completion prior to the BPA intervention was 67.6%, which declined to 66.5% then 63.8% at three and six months respectively. Improvements in wAAP percentages were seen at the East Clinic (74.9% to 81.4%) and Stoughton Clinic (76.4% to 78.9%). However, all other GPAM clinics had a decline in their wAAP completion percentages.
Conclusions: Following the initiation of the BPA, there was an overall decrease in the percentage of UW GPAM patients with an active wAAP. It does appear that there was a correlation between this intervention and an increase in wAAP rates at East and Stoughton Clinics. The decrease at all other clinics could be secondary to some degree of “BPA fatigue” where too many of these messages are displayed, or other factors, such as physician changes and ancillary staff levels and turnover which may also have an effect on the efficacy of this intervention. Continued assessment of root causes affecting the wAAP completions and targeted interventions to increase the wAAP rate would be appropriate.
Assessing the Diagnostic Pathway in Pediatric Brain Tumors: Factors Associated with Longer Diagnostic Latency
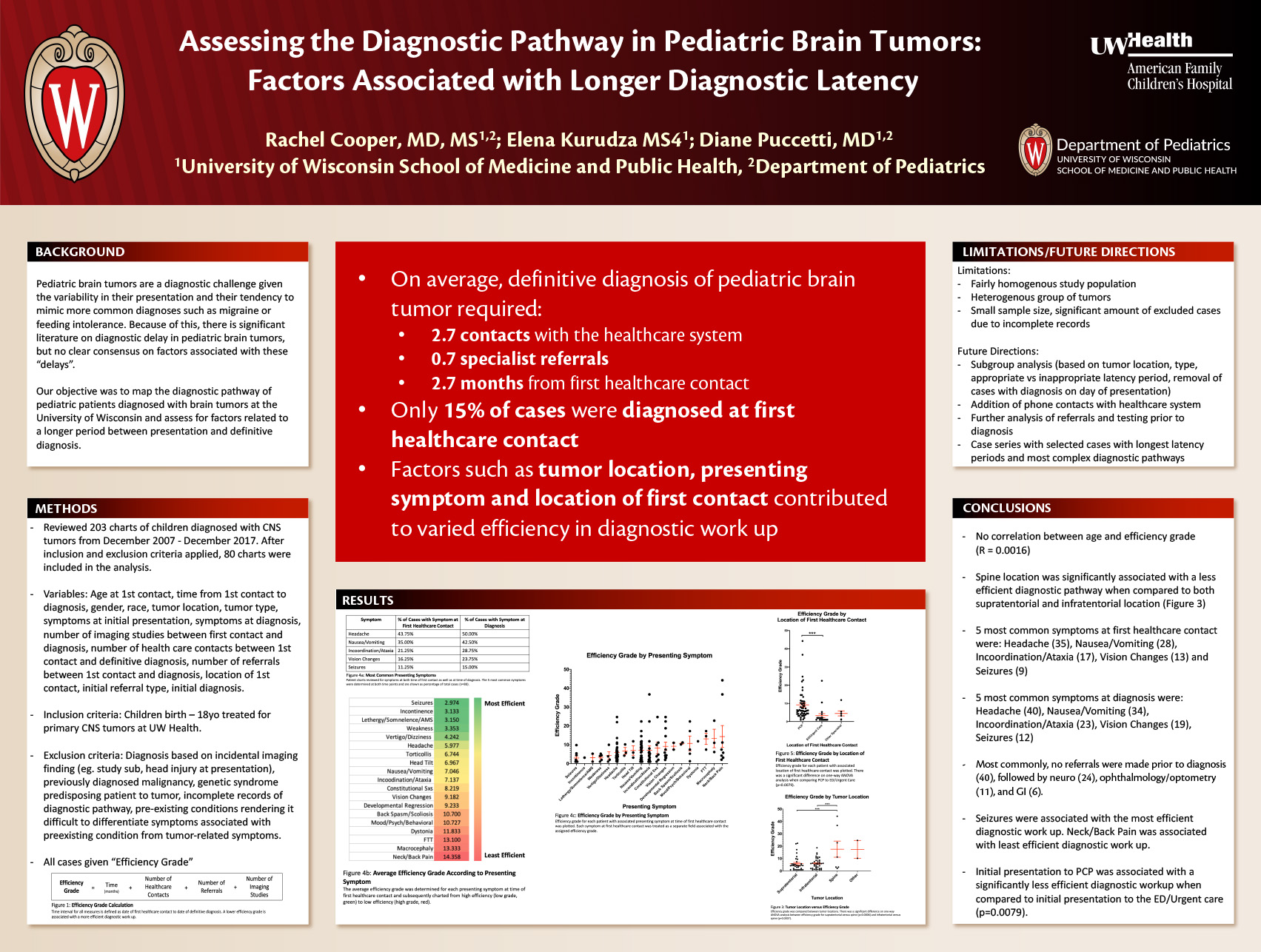
Click here for .pdf version of poster
Rachel Cooper, MD MS – University of Wisconsin Department of Pediatrics, PL3
Elena Kurudza MS4 – University of Wisconsin School of Medicine and Public Health
Diane Puccetti, MD – University of Wisconsin Department of Pediatrics
Background: Pediatric brain tumors remain a diagnostic challenge given the variability in their presentation and their tendency to mimic more common diagnoses such as migraine or feeding intolerance. Because of this, there is significant literature on diagnostic delay in pediatric brain tumors, though no clear consensus on factors associated with this delay or whether these delays have any impact on outcome.
Objective: To map the diagnostic pathway of patients diagnosed with brain tumors at the University of Wisconsin and assess for factors related to a longer period between presentation and definitive diagnosis.
Methods: In this study, we reviewed and analyzed the charts of all children treated for brain tumors at our institution between December 2007 and December 2017. The following variables were recorded in order to assess for common factors in cases with longer diagnostic latency: presenting symptoms, time between initial contact with the healthcare system and diagnostic brain imaging, number and type of healthcare visits, number and type of specialty referrals, and laboratory and imaging studies performed prior to brain imaging. Cases lacking documentation of initial contact with the healthcare system and subsequent workup leading to brain tumor diagnosis were eliminated from our analysis. We are also analyzing this data within subgroups of cases there was a potential delay versus a clear absence of delay (eg. child with headaches who requires several office visits prior to diagnosis vs. child who presents with first time seizure and is diagnosed at ED with brain mass).
Results: We anticipate completion of data analysis by early May.
Discussion: With this paper, we hope to identify factors that contribute to diagnostic delay in pediatric brain tumors such that, where possible, opportunities for earlier brain imaging can be identified. Furthermore, given that brain tumors are a rare cause of a number of common childhood symptoms, we hope to gain insight into the frequency of true diagnostic delay versus diagnostic latency that is to be expected with appropriate workup and referrals.
Antibiotic Prophylaxis for Infective Endocarditis: A Survey of Current Practice Amongst Pediatric Cardiology Provider
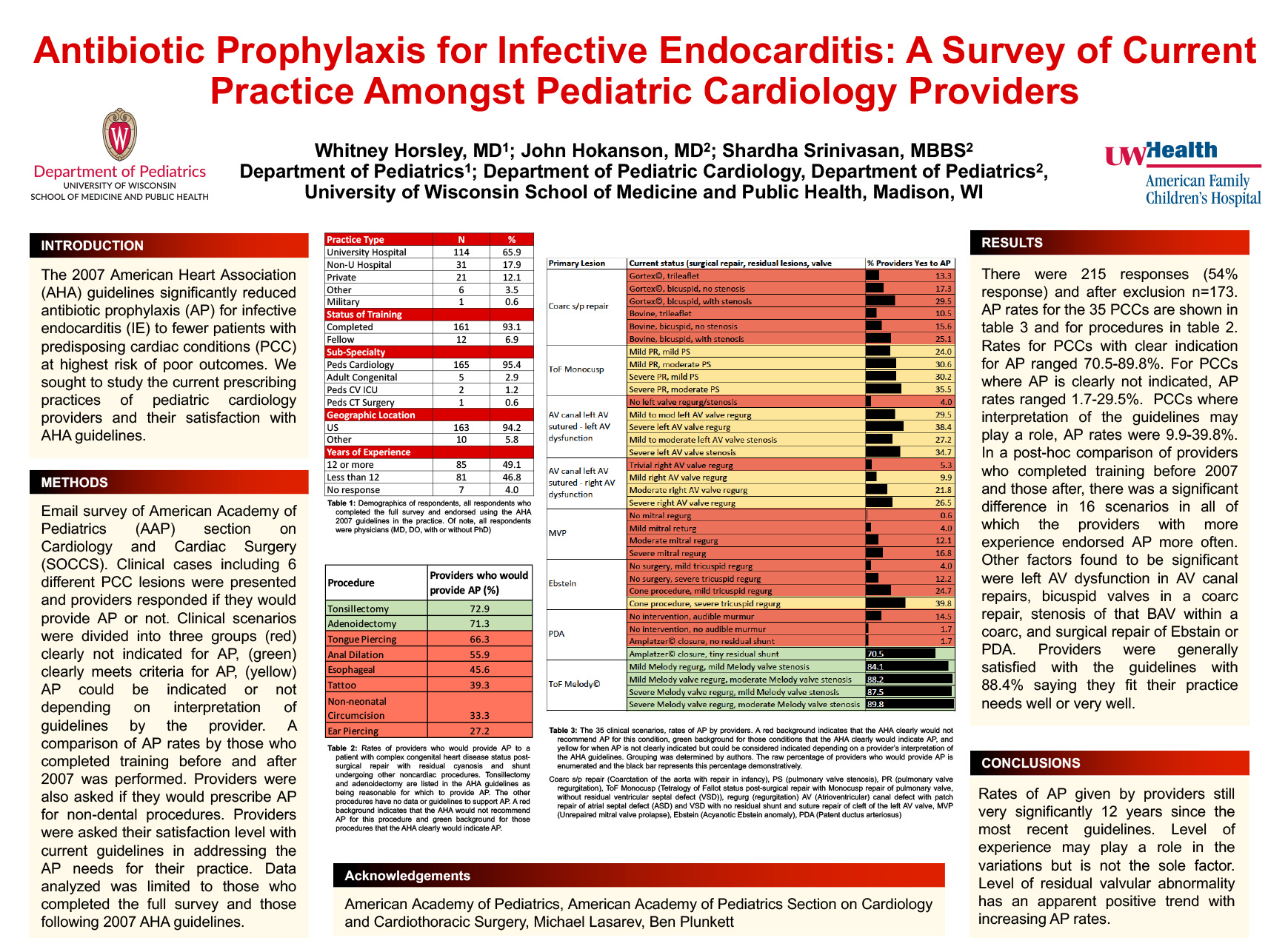
Click here for .pdf version of poster
Whitney Horsley1, MD; John Hokanson2, MD; Shardha Srinivasan, MBBS2
Affiliations:
Department of Pediatrics1
Department of Pediatric Cardiology, Department of Pediatrics2
University of Wisconsin School of Medicine and Public Health, Madison, WI
Background: The 2007 American Heart Association (AHA) guidelines significantly reduced antibiotic prophylaxis (AP) for infective endocarditis (IE) to fewer patients with predisposing cardiac conditions (PCC) at highest risk of poor outcomes.
Objective: We sought to study the current prescribing practices of pediatric cardiology providers.
Methods: A survey of pediatric cardiologists was conducted via emails sent to the American Academy of Pediatrics (AAP) section on Cardiology and Cardiac Surgery (SOCCS). The survey provided commonly encountered general cardiology scenarios and asked if the provider would or would-not prescribe AP. The cases included 6 different PCC lesions which fell into three broad categories: clearly high risk, clearly low risk and lastly those “open to interpretation” or unclear risk based on presence of residual defect or flow turbulence at or adjacent to repair site. All surgical cases were noted to be more than 6 months from surgery. A comparison of AP rates by those who completed training before and after 2007 was performed. They were also asked if they would prescribe AP for a patient with high-risk PCC undergoing 8 non-dental procedures which could risk bacteremia. Providers were asked their satisfaction level with current guidelines in addressing the AP needs for their practice. Percentages are presented for prescribing rates and satisfaction with current guidelines.
Results: There were 215 responses (54% response). Data analyzed was limited to those who completed the full survey and those following 2007 AHA guidelines (n = 173). Prophylaxis rates for PCCs clearly meeting criteria for AP ranged from 70.5-89.8%. Conversely, for PCCs which would not meet criteria for AP, prescribing rates varied from <1 to 29.5%. PCCs for which AP indication was unclear per guideline interpretation, AP rates varied from 9.9-39.8%. Similar variability in AP prescription in noted for procedures in setting of complex cyanotic heart defect. AP rates were higher by those with more experience when there was a difference. A majority of providers felt that the AHA guidelines met the needs of their practice well or very well.
Conclusions: These findings show that there is an inherent variability in AP prescribing practices within the AAP SOCCS based on both underlying PCC and various procedures. Further studies looking at AP prescribing rates with target questions to address the root cause of the variability shown here would be of benefit.
BAMO: Bronchiolitis Admissions Monitoring/Orders Revisiting Guideline Adherence and Order Accuracy
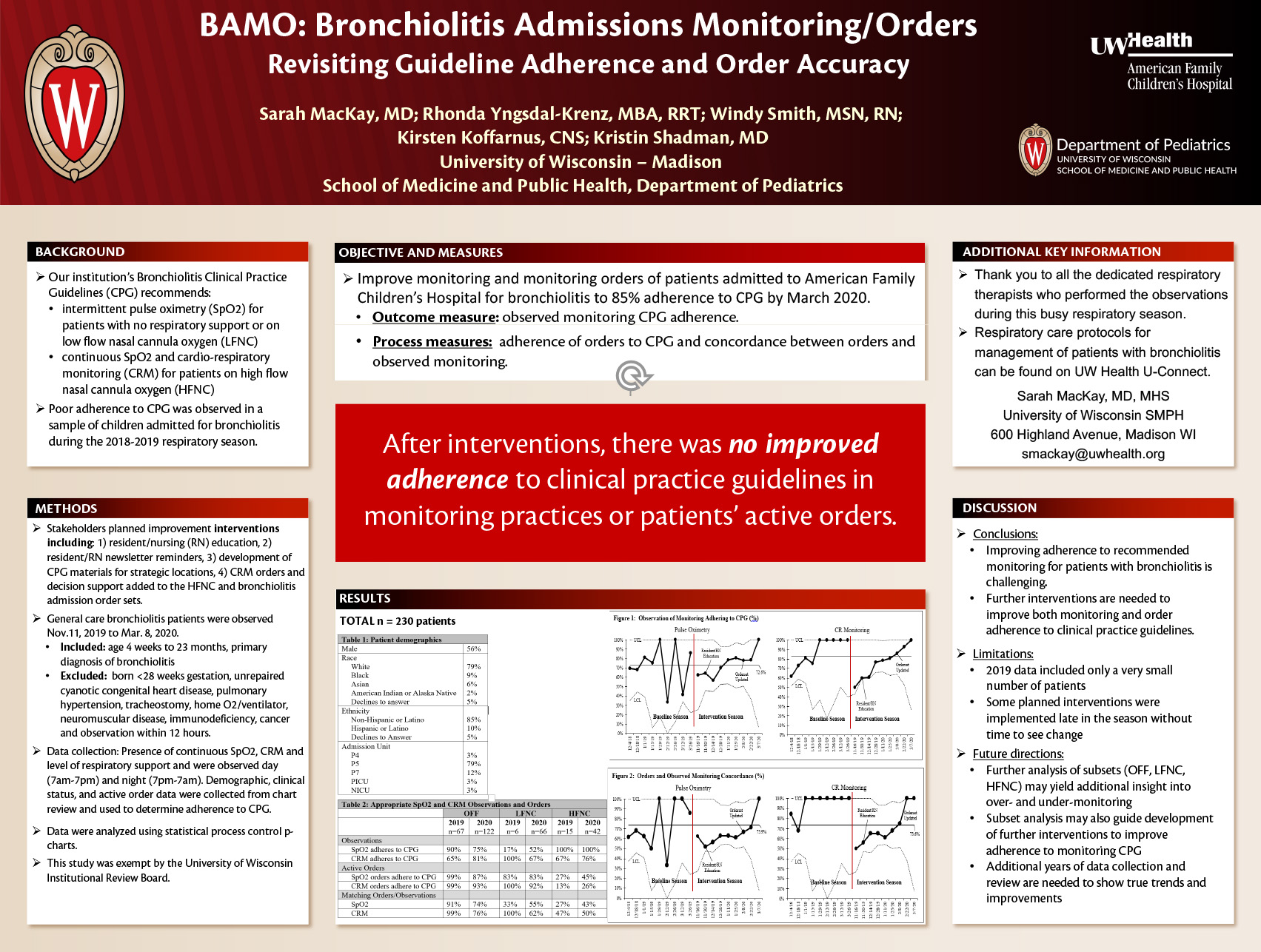
Click here for .pdf version of poster
Sarah MacKay, MD; Rhonda Yngsdal-Krenz, MBA, RRT; Windy Smith, MSN, RN; Kirsten Koffarnus, CNS; AFCH Respiratory Therapists; Kristin Shadman, MD
Background: Poor adherence to clinical practice guideline (CPG) recommendations for monitoring was observed in children admitted for bronchiolitis in 2018-2019. CPG recommends intermittent vitals and pulse oximetry (SpO2) for patients on no respiratory support (OFF) or low-flow nasal cannula (LFNC) and continuous SpO2 and cardio-respiratory monitoring (CRM) for those on high-flow nasal cannula (HFNC).
Objective: Improve monitoring and monitoring orders of patients admitted to American Family Children’s Hospital for bronchiolitis to 85% adherence to CPG by March 2020.
Method: Stakeholders reviewed monitoring practices and planned quality improvement interventions including resident/nursing (RN) education, resident/RN newsletter reminders, development of CPG materials for strategic locations, CRM orders and decision support added to the HFNC and bronchiolitis admission order sets. General care bronchiolitis patients were observed from November 11, 2019 to March 8, 2020. Inclusion criteria were children age 4 weeks to 23 months with a primary diagnosis of bronchiolitis; exclusions were children born <28 weeks gestation or with unrepaired cyanotic congenital heart disease, pulmonary hypertension, tracheostomy dependence, home oxygen/ventilator, neuromuscular disease, immunodeficiency, cancer and prior observation within 12 hours. Presence of continuous SpO2, CRM and level of respiratory support and were observed during the day (7am-7pm) and night (7pm-7am). Demographic, clinical status (stable/worsening), and active order data were collected from chart review and used to determine monitoring and order status adherence to CPG. Primary outcome measure was observed monitoring CPG adherence. Process measures were adherence of orders to CPG and concordance between orders and observed monitoring. Data were analyzed using statistical process control chart. This study was deemed exempt by the University of Wisconsin Institutional Review Board.
Results: 230 patients were observed; 42 on HFNC, 66 on LFNC, and 122 OFF. Demographics are summarized in Table 1. Monitoring and active orders adherence to CPG are in Table 2. SpO2 and CRM observed monitoring did not improve overall (Figure 1). Concordance of monitoring and orders did not improve overall (Figure 2).
Conclusion: Improving adherence to recommended monitoring for patients with bronchiolitis is challenging. Further strategies to address over-monitoring are necessary.
Depression screening in adolescents with type 1 diabetes: a project to improve mental health assessment and care in a pediatric diabetes clinic
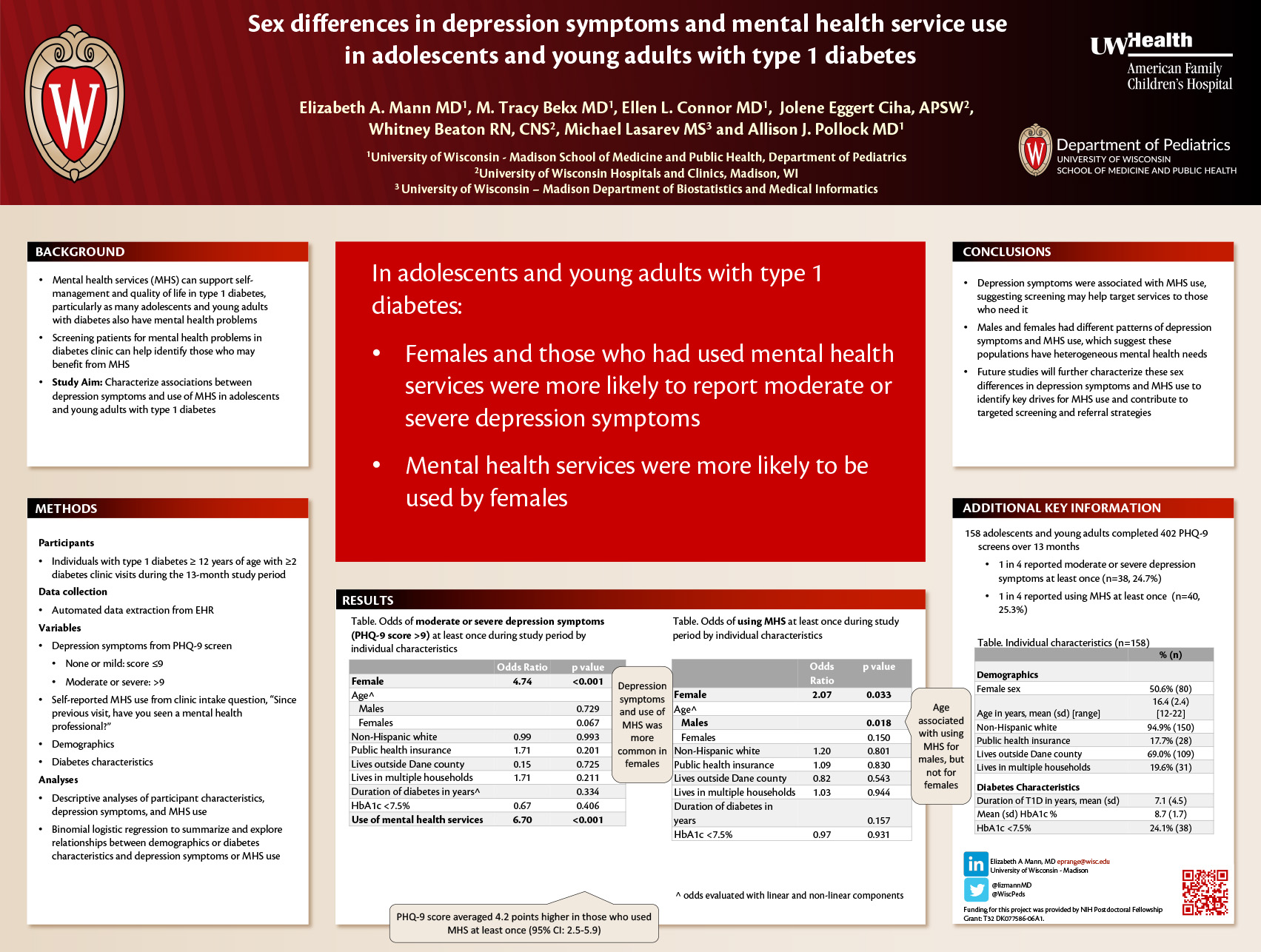
Click here for .pdf version of poster
Authors: Elizabeth A. Mann, MD1, Allison J. Pollock, MD1, M. Tracy Bekx, MD1, Jolene Ciha, CSW2, Whitney Beaton, RN, CNS2, and Ellen L. Connor, MD1
1 University of Wisconsin, Department of Pediatrics. Madison, Wisconsin.
2 University of Wisconsin Hospitals and Clinics. Madison, Wisconsin.
Purpose
Adolescents with type 1 diabetes (T1D) should routinely be screened for mental illness and referred to mental health providers as appropriate. At our pediatric diabetes center, screening rates were 24% and mental health referral outcomes were unknown. We hypothesized that improvement could be achieved through implementing a mental illness screening and referral program. We describe a quality improvement project aimed to improve screening and monitor outcomes of mental health referrals.
Methods
Key stakeholders informed the planning, implementation and evaluation of this project and met monthly to review data and discuss improvement steps. Individuals ages 12 years with T1D were screened with the Patient Health Questionnaire 9 (PHQ-9) at each of their four annually recommended clinic visits. Individuals were referred to mental health providers if their PHQ-9 was positive (e.g. score >9) or if there was a concern for mental illness regardless of score. Data from the electronic health record were monitored from all clinic visits September 2018 through October 2019. Our process measure was the proportion of eligible individuals who completed a PHQ-9. Our outcome measure was the proportion of those with positive PHQ-9 who subsequently received mental health services.
Results
Screening rate data are presented in Figure 1. A subset of patients seen at least twice during the study period were further analyzed and included 158 unique patients and 495 clinic visits (Table 1). 25% reported a positive PHQ-9 at least once (38 of 158). 25% reported using mental health services at least once during the study period (40 of 158). Positive PHQ-9 was more likely in females (p<0.001), but positive screen rates did not differ based on other characteristics (Table 1).
During 78% of visits when a positive PHQ-9 was reported (50 of 64), a referral for mental health services was placed (n = 18) or the individual was already seeing a mental health provider (n = 32). Of the individuals with positive a PHQ-9 who were not already seeing a mental health provider, 39% (7 of 18) subsequently received services. Therefore, mental health services were not pursued for 36% of the visits with positive screen (23 of 64).
Conclusion
Implementing a depression screening and referral program at a pediatric diabetes clinic improved screening rates in adolescents with T1D. A large proportion of patients were subsequently seen by a mental health provider. In addition to improving our referral rates following positive screen, additional work is needed to understand and improve rates of mental health service use in this population.
Adaptation of a Clinical Decision Support Tool for Child Abuse Detection and Evaluation in the Emergency Department
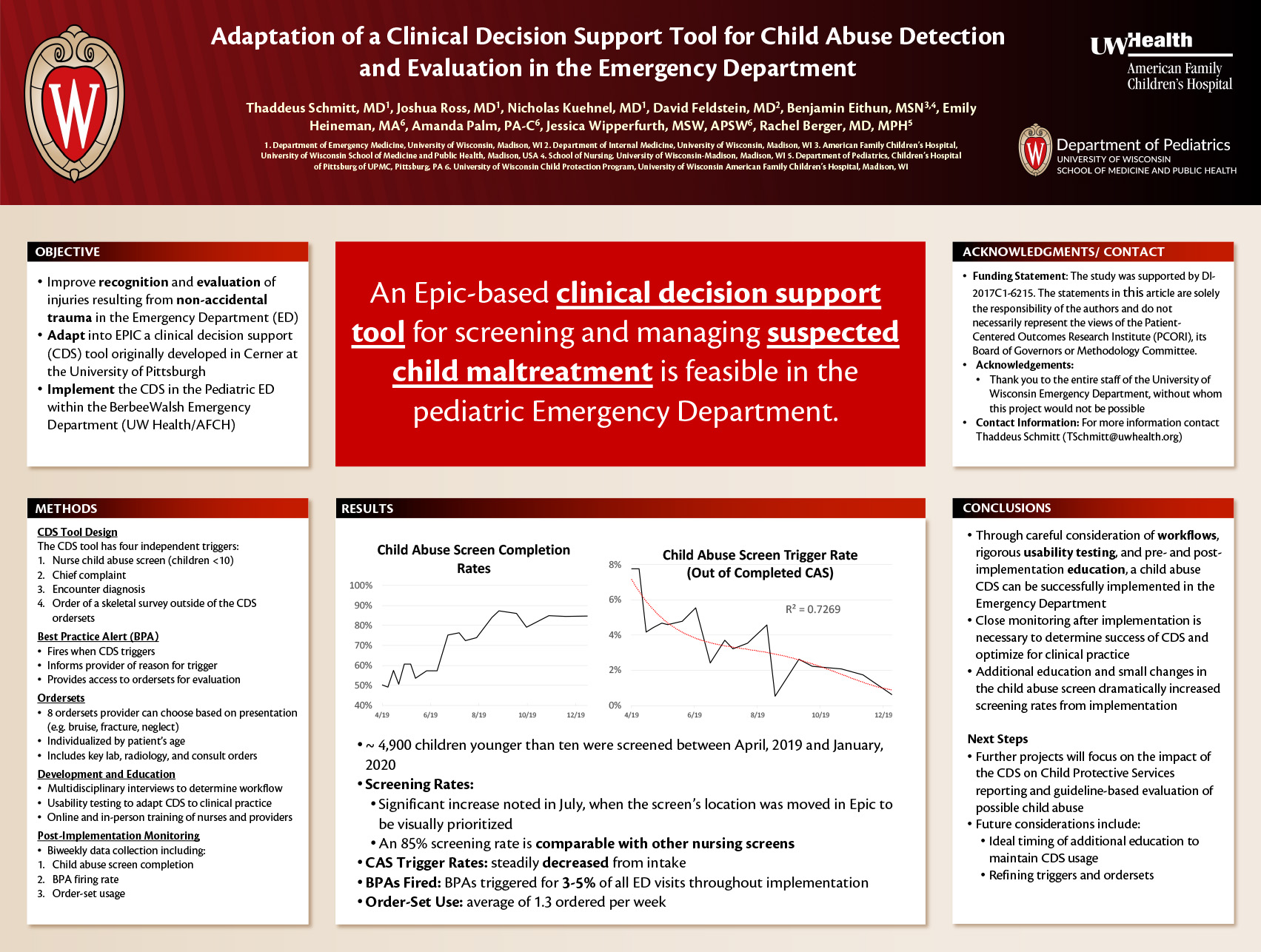
Click here for .pdf version of poster
Authors: Thaddeus Schmitt, MD1, Joshua Ross, MD1, Nicholas Kuehnel, MD1, David Feldstein, MD2, Benjamin Eithun, MSN, CRNP, RN, CRNP-AC, CCRN, TCRN3,4, Emily Heineman6, Amanda Palm, PA-C, LCSW6, Jessica Wipperfurth, SW6, Rachel Berger, MD, MPH5
- Department of Emergency Medicine, School of Medicine and Public Health, University of Wisconsin, Madison, WI
- Department of Internal Medicine, School of Medicine and Public Health, University of Wisconsin, Madison, WI
- American Family Children’s Hospital, University of Wisconsin School of Medicine and Public Health, Madison, USA
- School of Nursing, University of Wisconsin-Madison, Madison, WI
- Department of Pediatrics, Children’s Hospital of Pittsburg of UPMC, Pittsburg, PA
- University of Wisconsin Child Protection Program, University of Wisconsin American Family Children’s Hospital, Madison, WI
Objective
Adapt, implement, and evaluate an Epic-based clinical decision support (CDS) tool to aid in the standardization of detection and management of potential child maltreatment in the UW Pediatric Emergency Department (ED).
Methods
We adapted a CDS tool to address the under-recognition of injuries that potentially resulted from non-accidental trauma in the ED. The tool, which was originally developed in Cerner at the University of Pittsburgh Medical Center (UPMC), has four independent triggers: a nurse child abuse screen, chief complaint, encounter diagnosis, and the order of a skeletal survey outside of the CDS ordersets. Each trigger fires a best practice alert (BPA), which alerts providers to the possible risk of child abuse and provides access to standardized ordersets individualized to the patient’s age and clinical presentation to help guide further evaluation.
The tool was designed to incorporate into existing workflows, based on multidisciplinary pre-development interviews and two rounds of subsequent usability testing. Prior to implementation, nurses received online training and in-person review of the new screening questionnaire, and physicians were provided with live demonstrations and emailed reminders. Data has been collected biweekly regarding child abuse screen completion, BPA firing rate, and orderset usage.
Results
Approximately 4,900 children younger than ten years old were screened with the new CDS between launch in April, 2019 through January, 2020. Screen completion rates increased from 55% in the first month after launch to 85% in December, with a significant increase noted after moving the screens’ location in Epic. This higher rate is comparable to the completion rate of other nursing screens. Positive screens decreased from 7% of completed screens at launch to 1-2% in the last three months. BPAs triggered for 3-5% of all ED visits throughout implementation, with a gradual decrease noted since launch. Each orderset has been used, with an average of 1.3 ordered per week.
Conclusion
Careful consideration of workflows, rigorous usability testing, and provision of post-implementation education and optimizations allowed a child abuse CDS to be successfully implemented in the ED.
Correlation between Pediatric Intern Inpatient Volume and Milestones-Based Clinical Competency
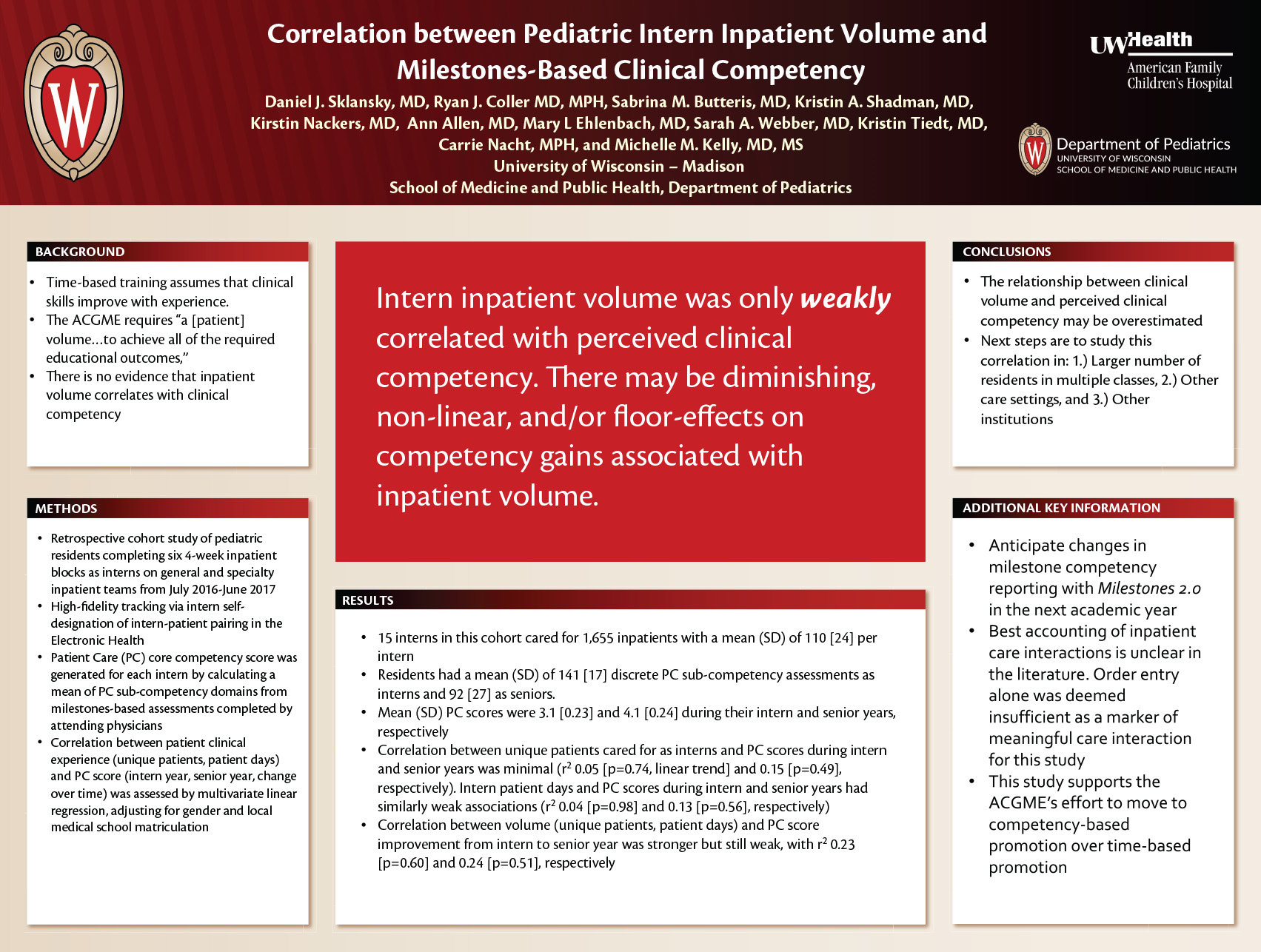
Click here for .pdf version of poster
Daniel J. Sklansky, MD1, Ryan J. Coller MD, MPH1, Sabrina M. Butteris, MD1, Kristin A. Shadman, MD1, Kirstin Nackers, MD1, Ann Allen, MD1, Mary L Ehlenbach, MD1, Sarah A. Webber, MD1, Kristin Tiedt, MD1, Carrie Nacht, MPH1, and Michelle M. Kelly, MD, MS1
1Department of Pediatrics, University of Wisconsin School of Medicine and Public Health
Background: The U.S. clinical training paradigm assumes that residents’ clinical skills improve with experience. Although the ACGME requires “a [patient] volume…to achieve all of the required educational outcomes,” it is unclear how volume correlates with clinical competency.
Objective: Determine the correlation between pediatric interns’ clinical volume and their clinical competency as measured by patient care (PC) milestones-based assessments.
Methods: This retrospective study followed one cohort of pediatric residents at a tertiary care children’s hospital completing six 4-week inpatient blocks as interns on general and specialty inpatient teams from July 2016-June 2017. High-fidelity tracking of intern-patient pairings was made possible by requiring interns to designate themselves as primary inpatient caregivers for their patients in the electronic health record (EHR) in order to print rounding lists. A PC core competency score was generated for each intern by calculating a frequency weighted mean of PC sub-competency domains from milestones-based assessment forms completed by attending physicians. Correlation between patient clinical experience (unique patients, patient days) and PC score (intern year, senior year, change over time) was assessed by multivariate linear regression, adjusting for gender and local medical school matriculation.
Results: The 15 interns in this cohort cared for 1,655 inpatients with a mean (SD) of 110 [24] per intern. The residents had a mean (SD) of 141 [17] discrete PC sub-competency assessments as interns and 92 [27] as seniors. Their mean (SD) PC scores were 3.1 [0.23] and 4.1 [0.24] during their intern and senior years, respectively. The correlation between unique patients cared for as interns and PC scores during intern and senior years was minimal (r2 0.05 [p=0.74, linear trend] and 0.15 [p=0.49], respectively). Intern patient days and PC scores during intern and senior years had similarly weak associations (r2 0.04 [p=0.98] and 0.13 [p=0.56], respectively). Correlation between volume (unique patients, patient days) and PC score improvement from intern to senior year was stronger but still weak, with r2 0.23 [p=0.60] and 0.24 [p=0.51], respectively.
Conclusion: This pilot study suggests that the relationship between clinical volume and perceived clinical competency may be overestimated. Next steps include studying a larger number of residents and incorporating other care settings and degrees of medical complexity in our measure of clinical volume.
Guidance for the Use of Pediatric PROMIS Measures in Ambulatory Clinics
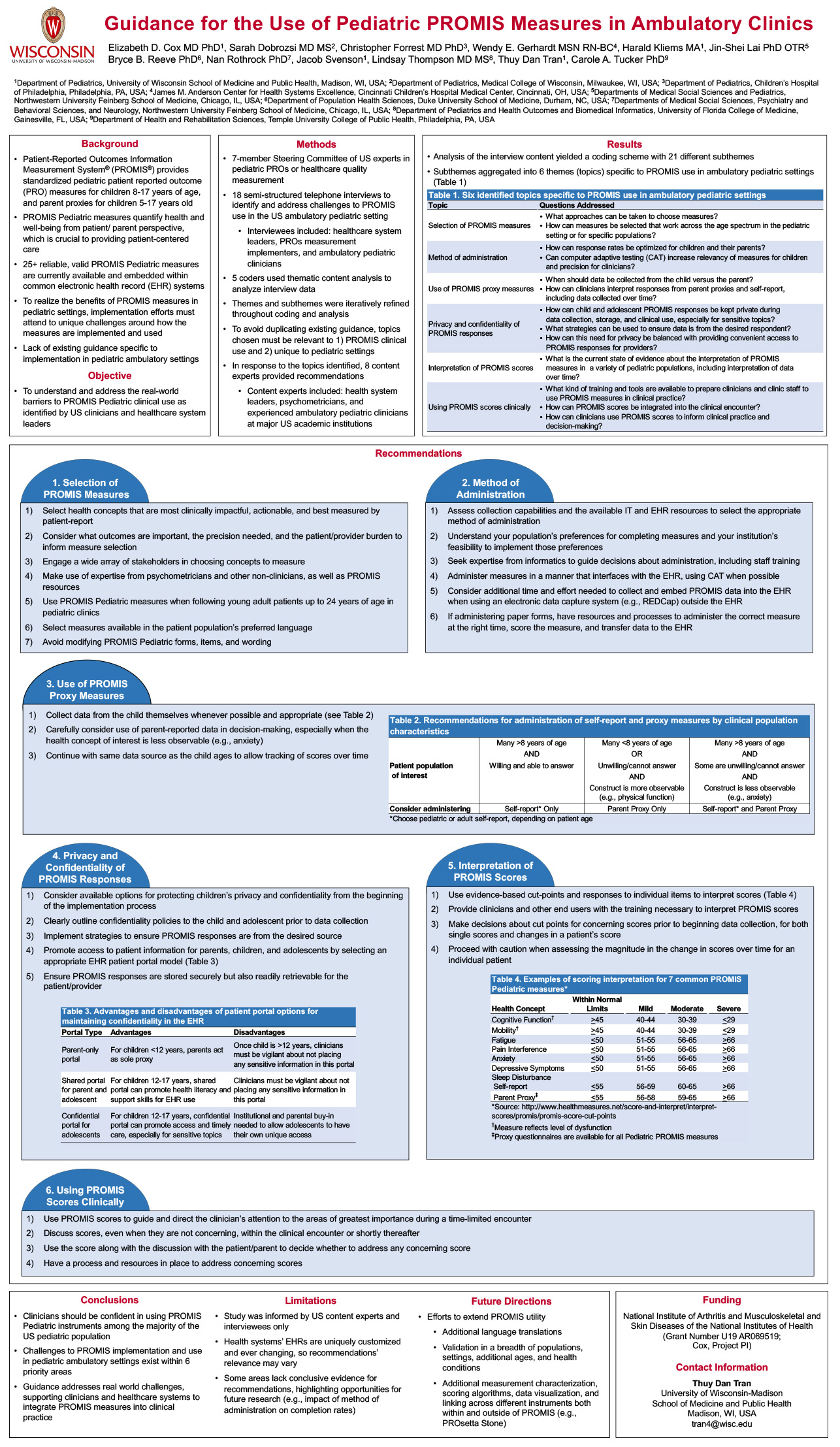
Click here for .pdf version of poster
Elizabeth D. Cox MD PhDa, Harald Kliems MSa, Jacob Svensona, Thuy Dan Trana
aDepartment of Pediatrics, University of Wisconsin School of Medicine and Public Health, Madison, WI
Abstract
Background: Clinical practice requires efficient assessments of health to enhance clinical decision-making and optimize patient outcomes. Patient-reported outcome measures quantify health from the patient perspective, which is crucial to patient-centered care. The Patient-Reported Outcomes Measurement System® (PROMIS®) provides standardized measures of patient-reported outcomes for use in clinical practice, with specific measures available for children from 8-17 years of age and parent proxies for children 5-17 years old. To realize the benefits of PROMIS measures, healthcare system and clinician leaders must attend to how the measures are implemented and used.
Objective: To advance patient-centered care, we identify challenges and potential solutions to support PROMIS use in the ambulatory pediatric setting,
Study design: 18 semi-structured telephone interviews of health system leaders, measurement implementers, and ambulatory pediatric clinicians were conducted. Five trained coders used thematic content analysis to iteratively identify and refine themes and subthemes in the interview data.
Results: Analysis of the interview content yielded a coding scheme with 21 different subthemes, which were further distilled into six themes specific to PROMIS use in ambulatory pediatric settings: 1) selection of PROMIS measures, 2) method of administration, 3) use of PROMIS Parent Proxy measures, 4) privacy and confidentiality of PROMIS responses, 5) interpretation of PROMIS scores, and 6) using PROMIS scores clinically. For example, interviewees recommended engaging a wide array of stakeholders to choose measures that are meaningful, actionable, and best assessed by patient-report; having the child respond themselves whenever possible; and considering different options for protecting children’s privacy. Training for clinicians was recommended to support score interpretation and timely discussion of both normal and concerning scores with patients.
Conclusions: To realize the benefits of PROMIS measures, healthcare system and clinician leaders must attend to how the measures are implemented and used.
Family centered care for patients with congenital heart defects: enhancing the role of palliative care
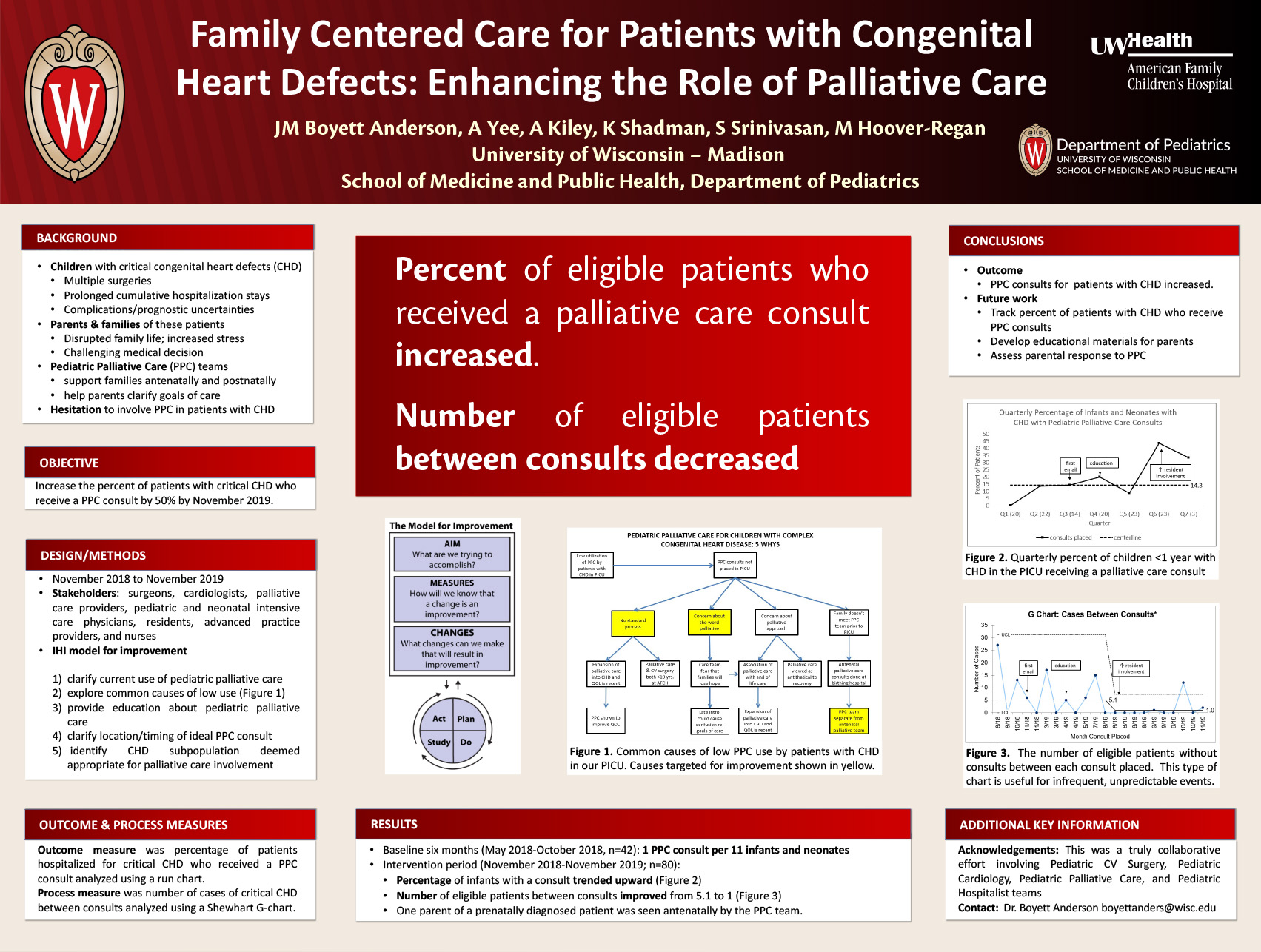
Click here for .pdf version of poster
AUTHORS: Boyett Anderson1, Jesse; Yee3, Alida ; Kiley2, Allie; Shadman4, Kristin; Srinivasan1, Shardha; Hoover-Regan2, Margo
INSTITUTIONS: Department of Pediatrics1 Divisions of Pediatric Cardiology2, Pediatric Palliative Care3 , and Hospital Medicine4; University of Wisconsin Hospital and Clinics, Madison, WI, United States.
Background: Children with critical congenital heart defects (CHD) require multiple surgeries and spend
substantial amounts of time hospitalized in the first year of life. Long hospital stays, complications, and slow recoveries disrupt family life and increase parental stress. Concurrently, parents make difficult decisions about their child’s care. Pediatric Palliative Care (PPC) teams can support families antenatally and postnatally, and help parents clarify goals of care. Some cardiac providers hesitate to involve PPC in the care of patients.
Objective: Increase the percentage of patients with critical CHD who receive a PPC consult by 50% by
November 2019.
Design/Methods: This study occurred November 2018 to November 2019. A team of stakeholders at our midsized cardiac surgery program consisting of surgeons, cardiologists, PPC, pediatric and neonatal intensive care physicians, residents, advanced practice providers, and nurses used the IHI model for improvement to 1) clarify current use of PPC services by the Heart Care Program; 2) explore common causes of low utilization of PPC services using five whys methodology (Figure 1); 3) provide education to Heart Care Program providers regarding PPC scope of services; 4) clarify location/timing of ideal PPC consult; and(5) identify CHD subpopulation of patients for whom PPC team involvement was deemed appropriate by providers . Outcome measure was percentage of patients hospitalized for critical CHD who received a PPC consult analyzed using a run chart. Process measure was number of cases of critical CHD between consults analyzed using a Shewhart G-chart.
Results: During the baseline six months (May 2018-October 2019), an average of 1 PPC consult was placed per 11 infants and neonates hospitalized for cardiac surgery (n=42). During the intervention period (n=80), median percentage of infants with a consult trended upward (Figure 2), and the number of eligible patients between consults improved from 5.1 to 1 (Figure 3). Additionally, one parent of a prenatally diagnosed patient was seen antenatally by the PPC team.
Conclusion(s): This initiative increased PPC involvement in the care of patients with critical CHD. Future work includes further assessment of percent of patients who receive PPC consults, development of educational materials regarding PPC for parents of children prenatally diagnosed with critical CHD, and assessment of parental response to PPC.
Session D: Care Delivery – Blackboard Collaborate Session
This is an accordion element with a series of buttons that open and close related content panels.
GME Action Learning: Supporting New Program Directors: A Needs Assessment
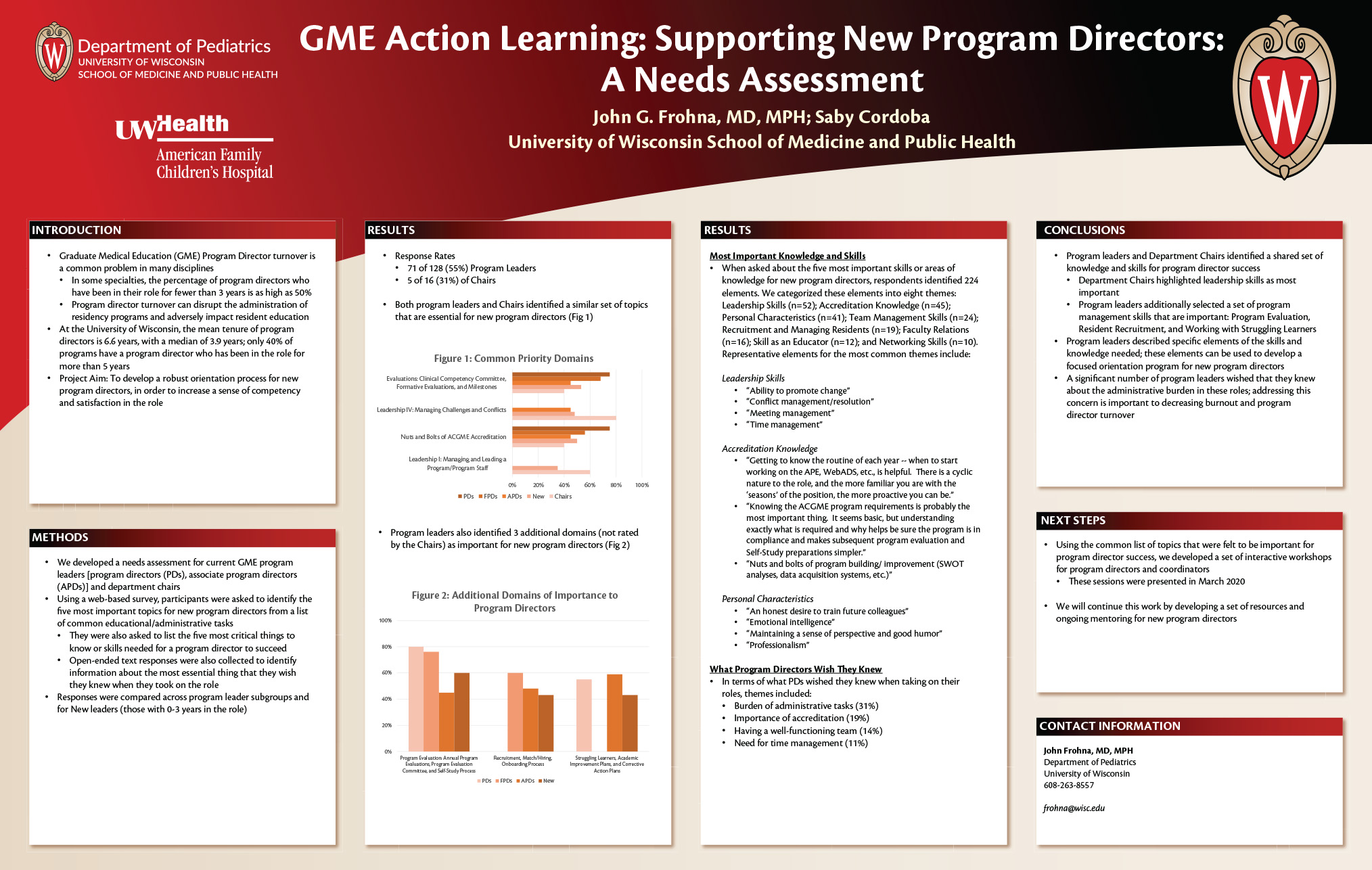
Click here for .pdf version of poster
John G. Frohna, MD, MPH University of Wisconsin School of Medicine and Public Health; Saby Cordoba
Background: Graduate Medical Education (GME) Program Director turnover is a common problem in many disciplines. In some specialties, the percentage of program directors who have been in their role for fewer than 3 years is as high as 50%. Program director turnover can disrupt the administration of residency programs and adversely impact resident education.
Problem Statement: At the University of Wisconsin, the mean tenure of program directors is 6.6 years, with a median of 3.9 years; only 40% of programs have a program director who has been in the role for more than 5 years. Our organization has averaged 10% annual turnover. The goal of this project was to develop a robust orientation process for new program directors, in order to increase a sense of competency and satisfaction in the role.
Intervention: We developed a needs assessment of existing program directors (PDs), associate program directors (APDs), and department chairs. Using a web-based survey, participants were asked to identify the five most important topics for new program directors from a list of common educational/administrative tasks. They were also asked to list the five most critical things to know or skills needed for a program director to succeed. Open-ended text responses were also collected to identify information about the most essential thing that they wish they knew when they took on the role.
Outcomes: Responses were obtained from 71 of 128 (55%) PDs and APDs and 5 of 16 (31%) of Chairs. Both groups identified a similar set of topics that are essential for new program directors: 1) Evaluations: Clinical Competency Committee, Formative Evaluations, and Milestones (63% of PDs, 40% of Chairs); 2) Managing Challenges and Conflicts (55% PDs, 80% Chairs); 3) Nuts and Bolts of ACGME Accreditation (59% PDs, 40% Chairs); 4) Managing and Leading a Program/Program Staff (39% PDs, 60% Chairs). In terms of what they wished they knew when taking on their roles, program director responses were grouped into several themes: burden of paperwork/accreditation, the importance of having a well-functioning team, and time management.
Barriers and Lessons Learned: Despite the low response rate from our department chairs, there is a shared understanding of the knowledge and skills needed for program directors to be successful. The number of current program directors who lament the amount of administrative work required to run a successful residency program is striking and remains an important consideration for burnout and program director turnover.
Conclusions: Using the common list of topics that were felt to be important for program director success, we developed a set of interactive workshops for program directors and coordinators; these sessions were presented in March 2020. The next steps for this project will include an ongoing set of resources and mentoring for new program directors.
Implementation and Evaluation of a Pediatric Observation Unit Using Condition Specific Guidelines
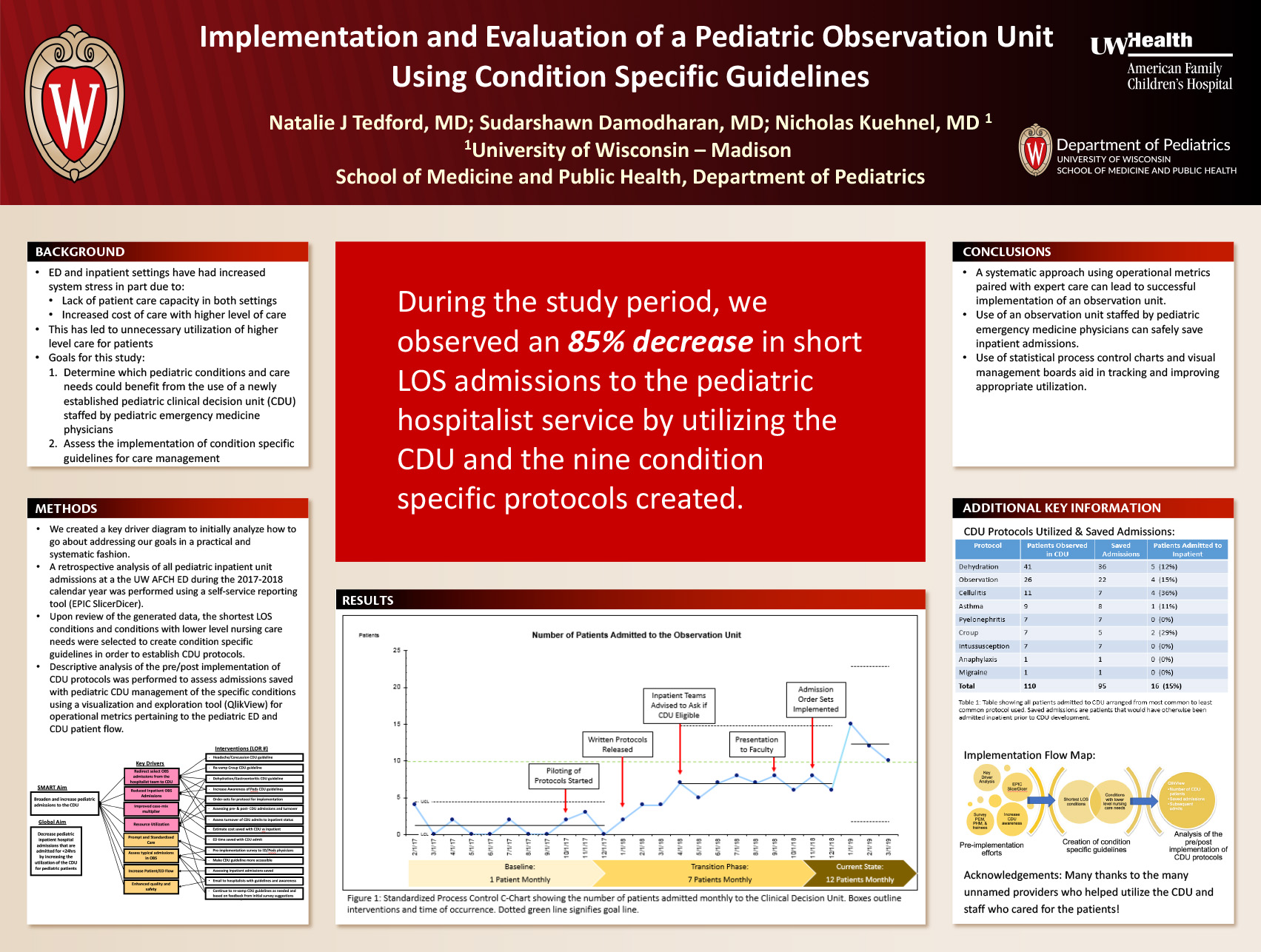
Click here for .pdf version of poster
Authors:
Natalie J Tedford; Sudarshawn Damodharan; Nicholas Kuehnel
Background
In recent years, inpatient units and emergency departments are seeing increased system stress due to capacity and cost constraints. As a solution, observation units have been a successful operational tool to address these concerns. In multiple tertiary care children’s hospitals, these units have resulted in reduced length of stay (LOS) and reduced costs of care. Unfortunately, there are no universal standardized parameters to follow in the operation of a new observation unit, such as the most appropriate patients, staffing, location, or process of implementation.
Goal
To determine which pediatric conditions and care needs could benefit from the use of a newly established pediatric clinical decision unit (CDU) staffed by pediatric emergency medicine physicians along with the implementation of condition specific guidelines for care management.
Methodology
A retrospective analysis of all pediatric inpatient unit admissions at a Midwest, tertiary care children’s hospital during the 2017-2018 calendar year was performed using a self-service reporting tool (EPIC SlicerDicer). Upon review of the generated data, the shortest LOS conditions and conditions with lower level nursing care needs were selected to create condition specific guidelines in order to establish CDU protocols. Descriptive analysis of the pre/post implementation of CDU protocols was performed to assess admissions saved with pediatric CDU management of the specific conditions using a visualization and exploration tool (QlikView) for operational metrics pertaining to the pediatric ED and CDU patient flow.
Results
After a review of short-stay inpatient observation admissions, nine CDU protocols were developed. Of protocols developed, dehydration was the most commonly used protocol accounting for 37% (41/110) of admissions (Table 1). Of all CDU admissions, 15% required inpatient admission for observation beyond 24 hours, with cellulitis having the highest percentage of observed patients requiring inpatient transfer. CDU admissions have increased from a baseline of approximately 1 patient monthly to current state 12 patients monthly (Figure 1).
Discussion
A systematic approach using operational metrics paired with expert can lead to successful implementation of an observation unit. Use of an observation unit staffed by pediatric emergency medicine physicians can safely save inpatient admissions. Use of statistical process control charts and visual management boards aid in tracking and improving appropriate utilization.
Insurance Coverage Impacts the Clinical Use of Prenatal Chromosomal Aneuploidy Screening: Implications for Health Equity
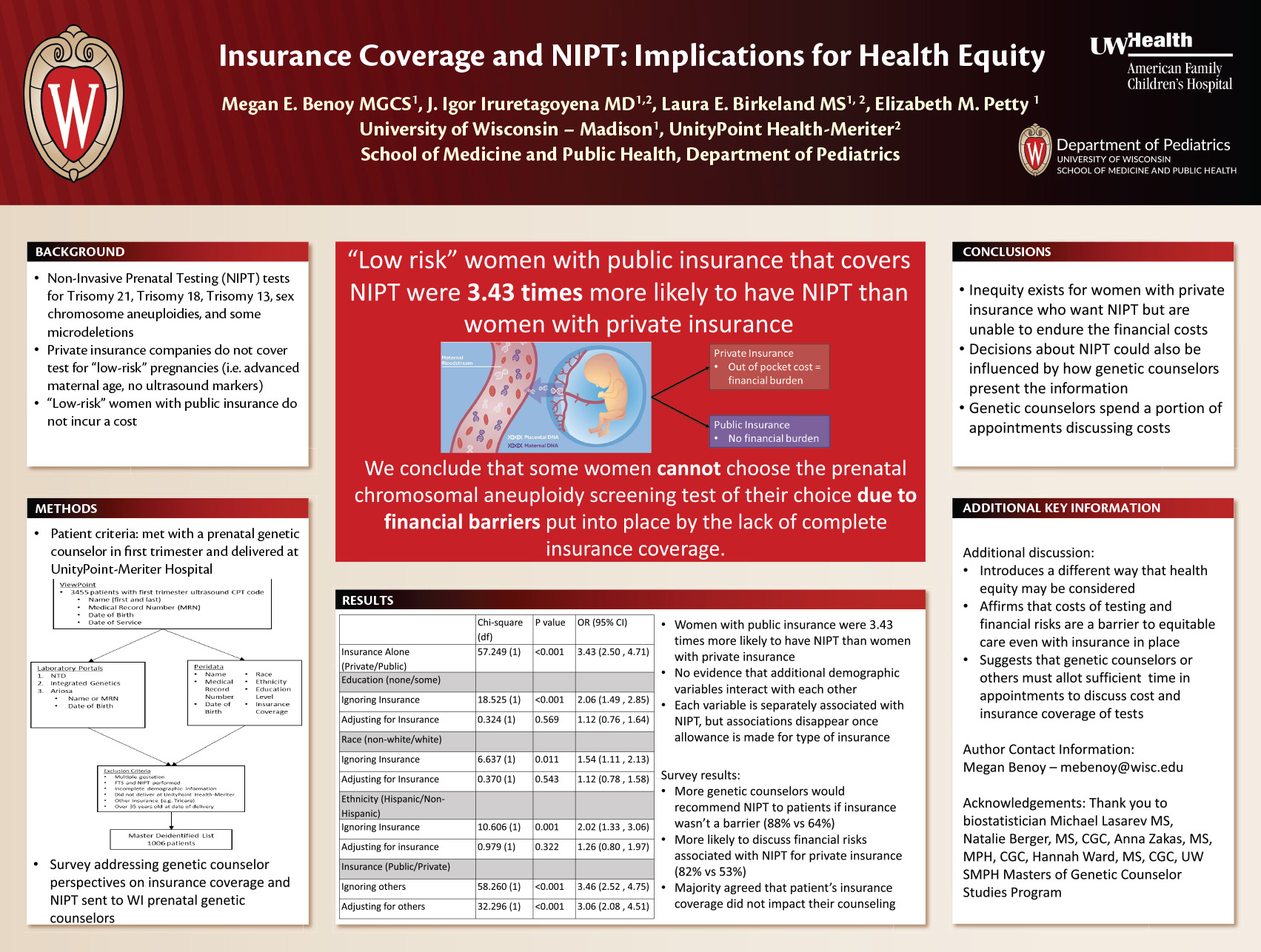
Click here for .pdf version of poster
Megan E. Benoy, BA1, J. Igor Iruretagoyena, MD2,4, Laura E. Birkeland, MS3,4, Elizabeth M. Petty, MD1
1School of Medicine and Public Health – University of Wisconsin, Madison, WI. 2 School of Medicine and Public Health (Department of Obstetrics and Gynecology) – University of Wisconsin, Madison, WI. 3School of Medicine and Public Health (Department of Pediatrics) – University of Wisconsin, Madison, WI. 4UnityPoint Health-Meriter Hospital, Madison, WI.
Non-Invasive Prenatal Testing (NIPT), also known as cell-free fetal DNA testing, is a prenatal screening test for chromosomal aneuploidy conditions where there is an extra copy of a chromosome, such as trisomy 21 (Down Syndrome), trisomy 18, and trisomy 13. A pregnancy is considered “low risk” for aneuploidy when a woman is under 35 years old with no other risk factors such as suggestive ultrasound findings. In Wisconsin, many private insurance companies do not cover initial NIPT for “low risk” women, but ”low risk” women with public insurance do not incur a financial burden if the clinician orders testing. The goal of this study was to determine if insurance coverage for NIPT impacts whether a “low risk” pregnant woman undergoes NIPT during the first trimester of pregnancy via a retrospective chart review during the 2018 calendar year. It also explored genetic counselor perspectives on how insurance coverage for NIPT is addressed with patients through a survey sent to prenatal genetic counselors in the state of Wisconsin. We found that women with public insurance were 3.43 times more likely to have NIPT than women with private insurance, indicating that insurance coverage may present a barrier to care. Additionally, our analysis showed no evidence that different demographic variables interact with each other after the allowance was made for type of insurance (X214=14.301, p=0.428) Our data suggests that more genetic counselors would recommend NIPT to their patients if insurance coverage was not a barrier and were more likely to discuss financial risks associated with NIPT when a patient had private insurance; a majority of genetic counselors disagreed that a patient’s insurance coverage impacted their counseling. We conclude that some women cannot choose the prenatal chromosomal aneuploidy screening test of their choice even when given the option due to financial barriers put into place by the lack of insurance coverage.
Use of the Independent Medical Spotter in Identifying Head/Neck Injuries in Division I Football Players
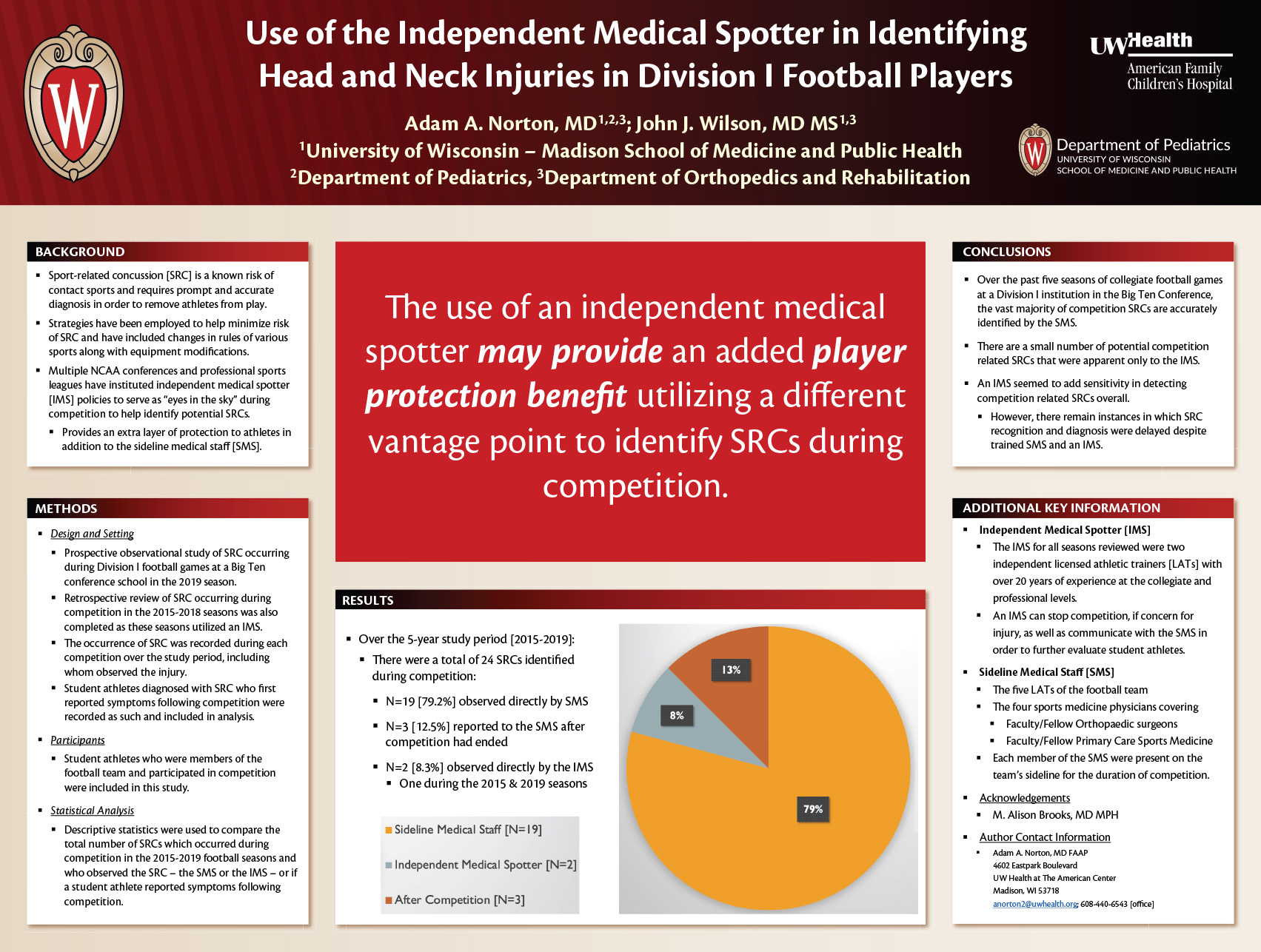
Click here for .pdf version of poster
Adam A. Norton, MD; John J. Wilson, MD, MS
University of Wisconsin School of Medicine and Public Health
Madison, Wisconsin
PURPOSE
Sport-related concussion (SRC) is a known risk of contact sports and strategies have been employed to help minimize risk. Multiple NCAA conferences and professional sports leagues have instituted independent medical spotters (IMS) to serve as “eyes in the sky” during events to help identify SRCs. We aimed to determine if the IMS identified more SRCs than would otherwise be detected by the trained sideline medical staff (SMS).
METHODS/STUDY DESIGN
We prospectively reviewed SRCs identified during Division I football games in 2019 at a Big Ten conference school. A new video review system (VRS) was also utilized. We retrospectively reviewed SRCs in the 2015-2018 seasons which utilized the IMS. The SMS included five licensed athletic trainers and four physicians. The IMS was the same licensed athletic trainer over all seasons reviewed. Descriptive statistics were used to compare SRCs identified by SMS [LAT/MD] versus IMS over these five seasons.
RESULTS
Over the 5-year study period there were a total of 24 SRCs during competition. Of those, 19 (79%) were observed directly by the sideline staff and 2 (8.3%) by the IMS. Both of the concussions identified by the IMS occurred during the 2019 season. A total of 3 (12.5%) SRCs were reported to the SMS after competition had ended.
CONCLUSIONS
In the five seasons of collegiate football games at a Division 1 university, the vast majority of SRCs are accurately identified by the SMS, but there are a small number of potential SRCs that were apparent only to the IMS which were later confirmed to be SRC by the trained medical staff. An IMS seemed to add sensitivity to detect SRC overall, there remain instances in which SRC recognition and diagnosis were delayed despite trained SMS and IMS.
Inter-rater reliability of pediatric point-of-care lung ultrasound in the PICU
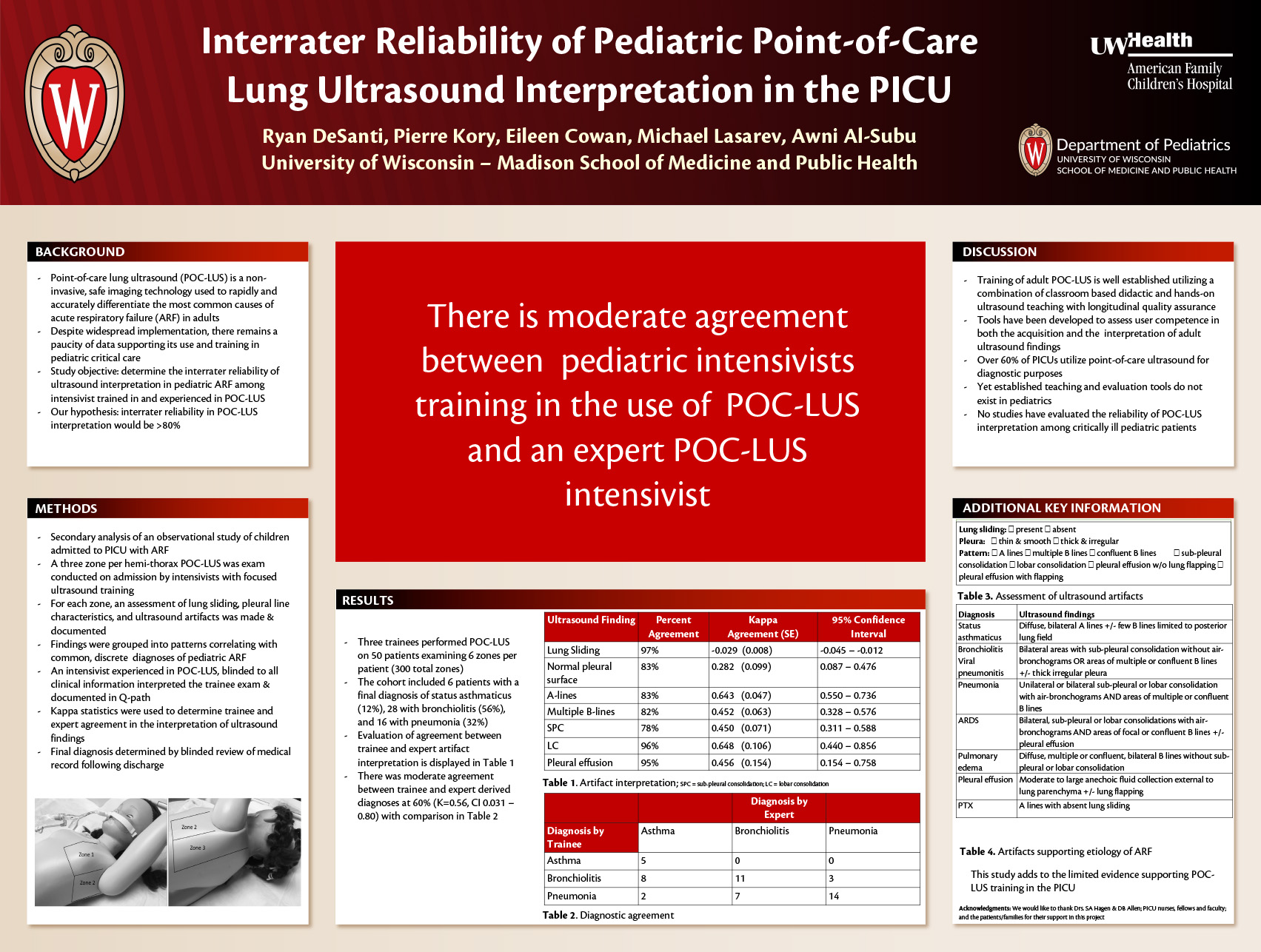
Click here for .pdf version of poster
Authors: Ryan L DeSanti, Pierre Kory, Eileen Cowan, Michael Lasarev, Awni M Al-Subu
Background: Point-of-care lung ultrasound (POC-LUS) is a non-invasive, safe imaging technology that can be used to rapidly and accurately differentiate the most common causes of acute respiratory failure (ARF) in adults. Despite widespread implementation, there remains a paucity of data supporting its use and training in pediatric critical care. Our objective was to determine the inter-rater reliability of ultrasound interpretation in pediatric ARF among intensivists trained and experienced in POC-LUS.
Methods: This was a planned secondary analysis of an observational study of children admitted to a 21-bed PICU undergoing POC-LUS for the evaluation of ARF. A three zone per hemi-thorax POC-LUS exam was conducted on admission by intensivists with focused ultrasound training. For each zone, an assessment of lung sliding, pleural line characteristics, and ultrasound artifacts was made. Findings were grouped into patterns correlating with discrete diagnoses of pediatric ARF. An intensivist experienced in POC-LUS, blinded to all clinical information, interpreted the trainee examination. Kappa statistics were used to determine provider agreement in the interpretation of ultrasound findings. Final patient diagnosis was determined by a blinded review of the chart following hospital discharge.
Results: Three trainees performed POC-LUS on 50 patients examining 6 zones per patient (300 total). The cohort included 6 (12%) patients with status asthmaticus, 28 (56%) with bronchiolitis, and 16 (32%) with pneumonia. There was moderate agreement between trainee and expert derived diagnoses at 60% (K=0.56, CI 0.031 – 0.80). Evaluation of the presence of lung sliding (K=-0.029; CI -0.045 – -0.012) and the presence of a normal pleural line (K=0.282; CI 0.087 – 0.476) was low. Interpretation of ultrasound artifacts ranged from moderate to high (K=0.452; CI 0.154 – 0.758 for pleural effusions to K=0.648; CI 0.550 – 0.736 for presence of A-lines).
Conclusions: There is moderate agreement between pediatric intensivists training in POC-LUS and an expert intensivist. While the body of data supporting the evaluation of adult patients with POC-LUS should not be extrapolated to pediatrics, this study adds to the limited evidence supporting point-of-care ultrasound training in the PICU.
Parents’ Knowledge and Acceptability of Mindfulness for Pediatric Asthma Care
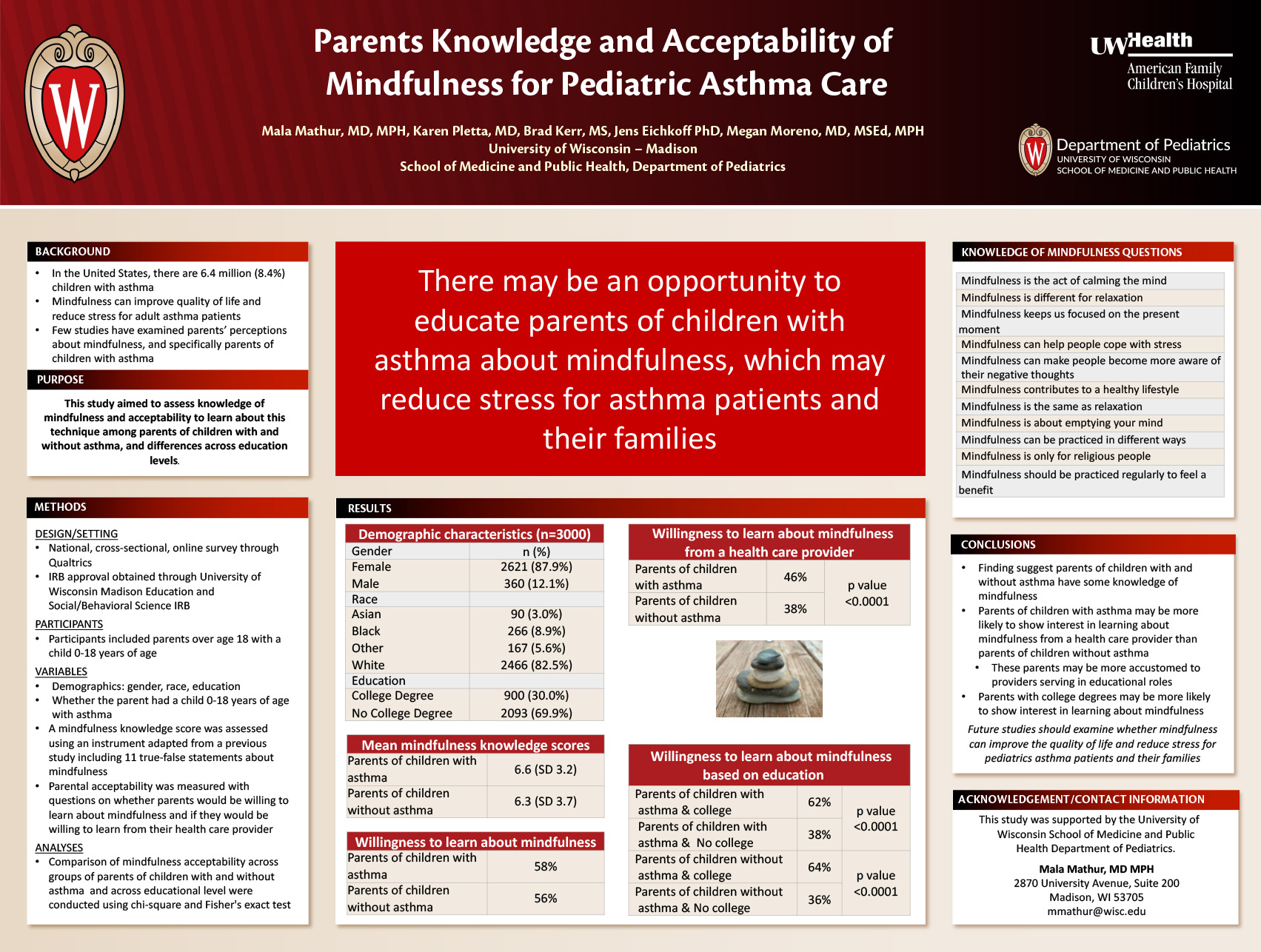
Click here for .pdf version of poster
Mala Mathur MD, MPH, Karen Pletta MD, Brad Kerr MS; Jens Eickhoff PhD, Megan Moreno MD, MSEd, MPH
Background: In the United States, there are 6.4 million (8.4%) children with asthma. Mindfulness has been shown to improve quality of life and reduce stress for adult asthma patients, but use of this technique has not yet been explored in pediatric asthma patients.
Objective: This study aimed to assess knowledge of mindfulness and perceived acceptability to learn about this technique from a health care provider among parents of children with and without asthma, and differences across demographic factors.
Methods: We conducted a national, cross-sectional, online survey. Parents of children 0-18 years were recruited from Qualtrics panels. Participants indicated whether at least one child had asthma. Knowledge of mindfulness was assessed using an instrument adapted from a previous study including 11 true-false statements about mindfulness (e.g., “Mindfulness can contribute to a healthy lifestyle”). Acceptability was measured with questions on whether parents would be willing to learn about mindfulness and if they would be willing to learn from their health care provider. All responses used a 5-point Likert scale. Comparisons of mindfulness acceptability between demographic groups were conducted using chi-square and Fisher’s exact test.
Results: Participants included 3000 parents; most were female (87%) and white (82%) with an average age of 37.1 years (SD=10.2). Participants averaged 6.3 (SD=3.2) out of 11 correctly labeled knowledge statements. Over a quarter of participants (n=797, 27%) had children with asthma; they had an average of 6.6 (SD=3.07) out of 11 correctly labeled knowledge statements. Parents of children with asthma were more likely to be willing to learn about mindfulness from their health care provider compared to those without asthma (46% vs. 38%, p<0.0001). College educated parents were more willing to learn about mindfulness compared to parents without a college education (p<0.05). College educated parents of children with and without asthma (p=0.47) did not differ in their likelihood to show interest in learning about mindfulness techniques.
Conclusion: Findings suggest an opportunity to incorporate mindfulness teaching into asthma care for pediatric patients with the goal to reduce stress and improve quality of life for asthma patients. Next steps include evaluating effects of mindfulness on asthma care for children.
Treatment of a 16-year-old with Clostridium septicum Myonecrosis
Click here for .pdf version of poster
Matthew E Naumann, MD, PGY-3 Resident, Department of Pediatrics, University of Wisconsin, Madison, WI
Sheryl L Henderson, MD, PhD, Assistant Professor, Department of Pediatrics, Division of Infectious Diseases, University of Wisconsin, Madison, WI
Background:
Clostridium septicum myonecrosis is a process that has rarely been reported in children, and is often found to be secondary to significant gastrointestinal pathology or neutropenia. It is notoriously difficult to treat and has a high mortality rate, with rates thought to be at least 50% in previously healthy patients. Ideal treatment is thought to be a combination of parenteral antibiotics and surgical debridement. Hyperbaric oxygen therapy is a treatment that is not standard of care and is infrequently used; however, literature has suggested its potential usefulness.
Case History:
This case describes a 16-year-old girl with a history of small cell ovarian cancer s/p resection and cycle 1 of chemotherapy who was admitted for abdominal pain and unrevealing abdominal imaging. On the day of admission, she rapidly progressed to septic shock secondary to neutropenic colitis requiring total colectomy and delayed abdominal closure. Her blood cultures were found to be growing C septicum. Throughout her hospital course, she remained on a wide range of broad-spectrum antibiotics, many of which should have appropriately treated her infection. On hospital day #8, she developed left hip pain and redness. Imaging at the time showed some muscle edema. When her pain persisted, she was taken to the OR out of concern for necrotizing fasciitis; what the surgeons found instead was extensive muscle necrosis. Biopsies of the muscle demonstrated gram-positive rods (presumed C septicum). Given the extent of the necrosis, surgical debridement was not an option. At this point, the use of hyperbaric oxygen was explored. Given that our institution does not have ready access to a hyperbaric oxygen chamber, and given that the patient was too unstable for transport, the decision was made to try hyperoxia utilizing her endotracheal tube. This trial took place on hospital day #21 and consisted of 24 hours of 100% FiO2 followed by a 24 hour period of alternating 6 hour segments of 100% FiO2 and 21% FiO2. Two days following completion of this trial, the patient reported resolution of her hip pain, and her clinical course continued to slowly improve until discharge.
Discussion:
This case demonstrates two important points. First, it describes myonecrosis—a rare complication of C septicum bacteremia in a pediatric patient. Second, it describes the successful use of hyperoxia as an adjunct treatment modality in a patient with a severe anaerobic soft tissue infection.
Division of admissions among pediatric hospitalist teams
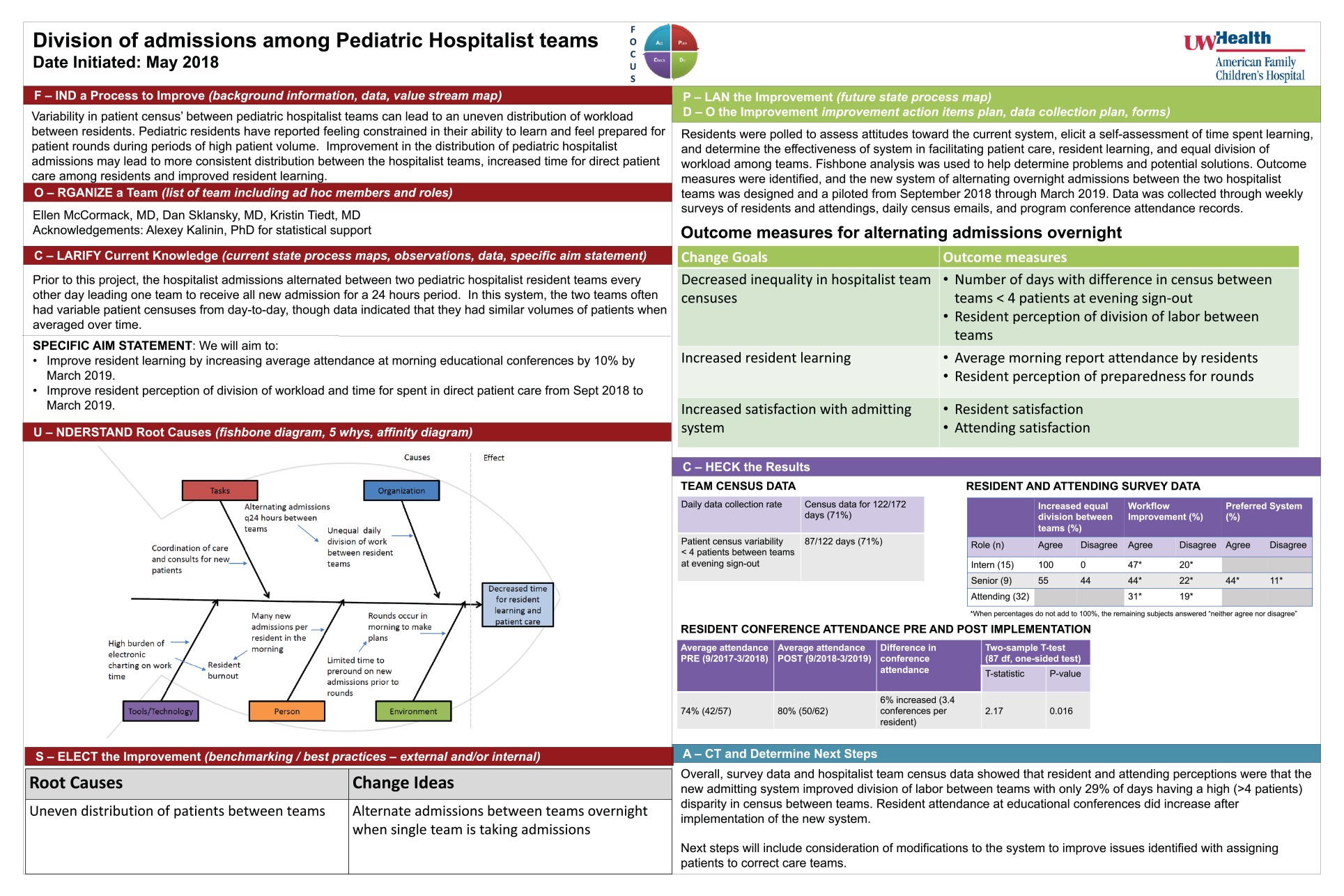
Click here for .pdf version of poster
Authors: Ellen McCormack, MD1; Dan Sklansky, MD2; Kristin Tiedt, MD2
1University of Wisconsin Hospitals and Clinics Pediatric Residency
2University of Wisconsin Department of Pediatrics Hospitalist Medicine
Background
Alternating admissions between pediatric inpatient teams based on the date may lead to excessive variability in team census and workload, particularly due to the substantial work required to care for patients on the first day of hospitalization. Teams that are too busy or not busy enough due to the nature of alternating daily admissions may not function ideally in a system designed for an average daily census.
Objective
Design and implement a new admitting system and assess its effect on 1.) Team census disparity, 2.) Resident learning opportunity as indicated by conference attendance, and 3.) Resident and attending perception of workload consistency and time for direct patient care.
Design
Residents were surveyed to assess attitudes toward the current admitting system. Fishbone analysis was used to help determine problems and potential solutions. Outcome measures were identified, and a new system of alternating overnight admissions between the two hospitalist teams was designed and piloted for 6 months starting Sept 15, 2018. Data were collected through daily census logs, program conference attendance records, and weekly surveys of resident and attending physicians using questions on a Likert scale to assess the effect of the new system on workload consistency and time for direct patient care (Table 1).
Results
Over the 6-month study period, census data were collected on 71% of days (122/177) during which inpatient teams had a census disparity of < 4 patients on 71% (87/122) of days. Morning report attendance among residents on a program level increased from 74% to 80% (6% increase, p= 0.016) when compared with the same 6 months from the previous year. Weekly survey data from residents and attendings showed that more residents preferred the new system than did not, and that few residents and attendings disagreed with the statement that the new system improved workflow. (Table 2)
Conclusion
A change to the admitting system resulted in decreased team census disparity and was correlated with increased conference attendance while garnering substantial support from resident and attending physicians. Next steps include honing the admitting system to further decrease team disparities that result in systems stresses and studying outcomes via quality improvement methodology.
Ethical Justification of Heart Donation after Circulatory Death and Implications for the Future of Organ Transplantation
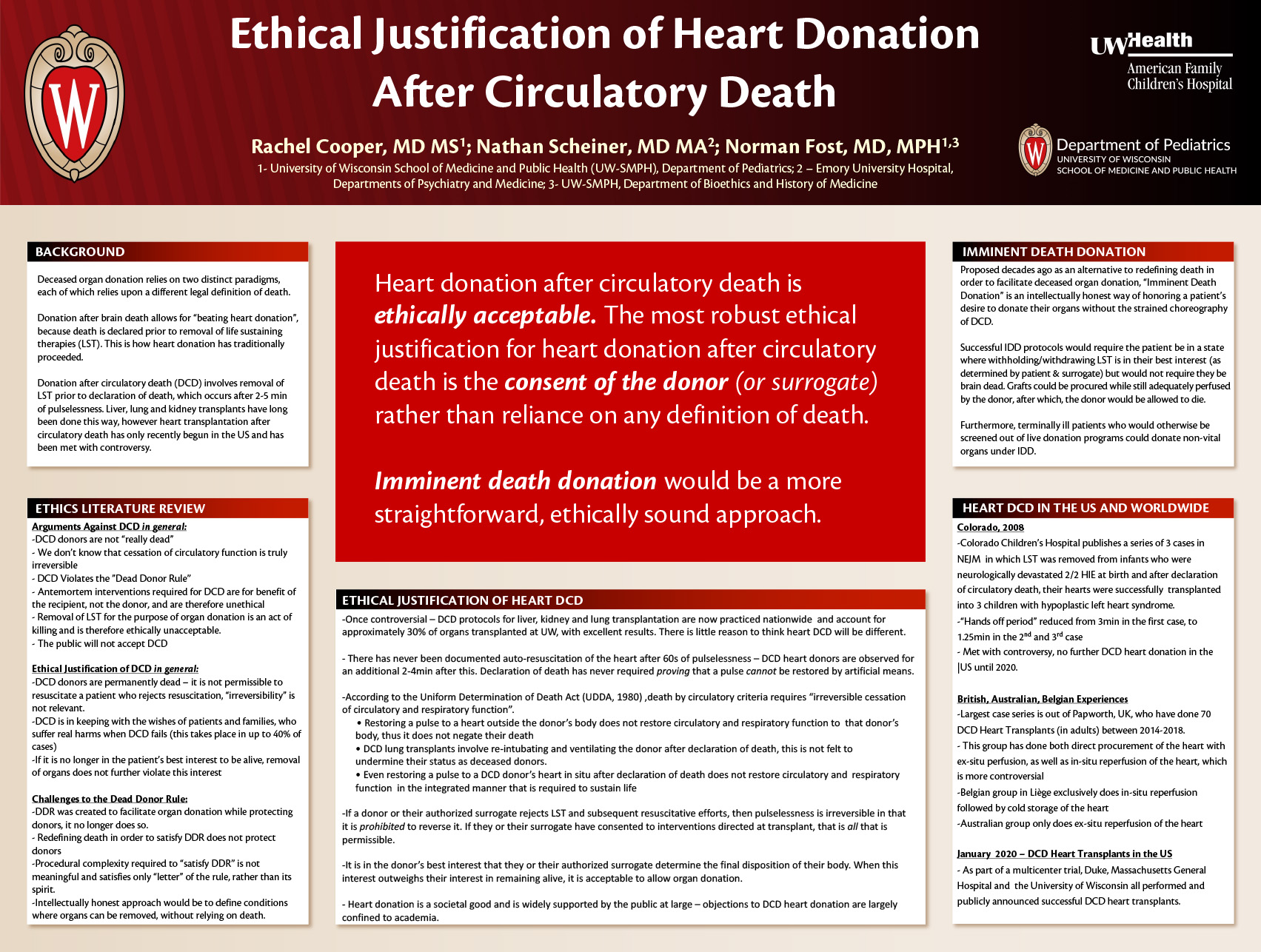
Click here for .pdf version of poster
Rachel Cooper, MD MS; Nathan Scheiner, MD MA; Norman Fost, MD MPH
Background: The creation of “Death by Neurological Criteria” (“brain death”) and delineation of the “Dead Donor Rule” (DDR) were both instruments for advancing the practice of organ transplantation without endangering public trust. More recently, liver, lung and kidney donation after circulatory death (“DCD donation”) has gone from engendering controversy to being widely practiced and thereby greatly expanding the pool of eligible organ donors worldwide. Previous DCD protocols have not included heart donation due to concern about ischemic damage to the graft during the dying process and medicolegal concern that restarting a donor heart, even in another body, negates the declaration of death by circulatory criteria and therefore violates the DDR. In recent years, successful DCD heart transplants have taken place in England, Belgium and Australia and in January 2020, three US transplant centers began doing DCD heart transplants. While physicians and ethicists have long debated the merits and shortcomings of brain death and the DDR, the recent success of DCD heart transplantation, highlights the conceptual, ethical and intellectual inadequacy of both current legal definitions of death and the DDR. One alternative that has long been proposed is “Imminent Death Donation” (IDD), a practice wherein patients are allowed to donate organs prior to declaration of death, which would be a more straightforward, intellectually honest approach to organ donation.
Objective: To assess the ethical and medicolegal arguments for and against heart DCD, as well as preliminary public reactions to the practice and the potential impact of this practice on transplant practice and policy.
Design/Methods: We performed critical literature review of ethics, medical and legal literature pertaining to liver, lung and kidney DCD, as well as emerging literature on heart DCD. In addition to this, we reviewed bioethics literature on the Dead Donor Rule, the Uniform Determination of Death Act and the concept of Imminent Death Donation (IDD). Lastly, this paper looks at media and social media reactions to the announcement of successful heart DCD transplants that took place at Duke, Massachusetts General Hospital and the University of Wisconsin in January 2020.
Conclusion: Heart DCD is ethically justified, however not by appealing to either the DDR or the legal definition of circulatory death, but rather by basing this justification on informed consent and bodily autonomy of the donor. Furthermore, the more intellectually honest approach to organ donation by DCD candidates would be “Imminent Death Donation” which would also minimize failed DCD attempts and help preserve graft function. Lastly, public reactions to recent DCD heart transplants do not indicate that this practice will cause widespread controversy, nor that that the public even perceives a substantive difference between donation after brain death and DCD.
Care Management of Non-emergent Echocardiographic Diagnosis in Newborns
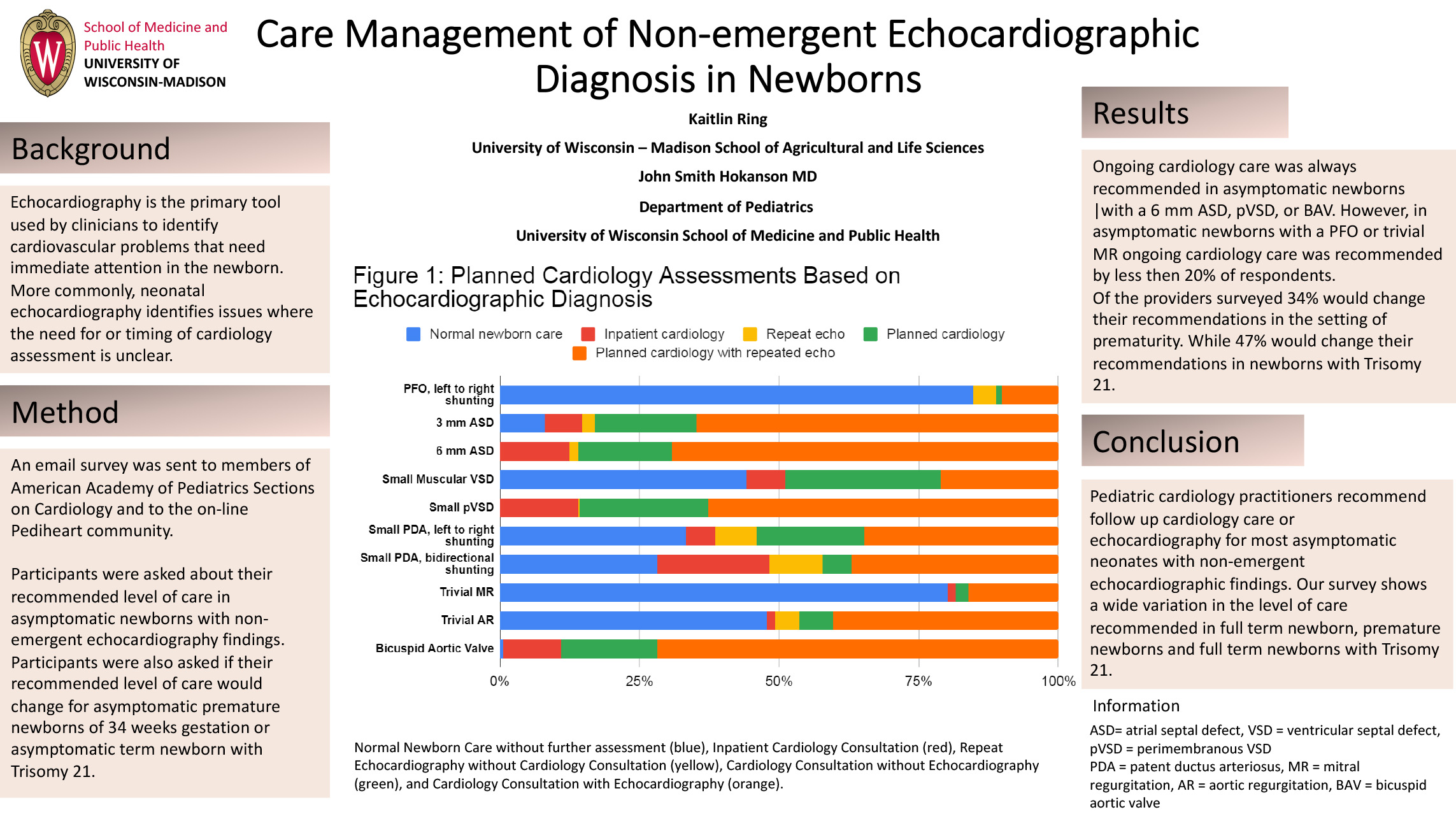
Click here for .pdf version of poster
Authors:
John Smith Hokanson MD
Department of Pediatrics
University of Wisconsin School of Medicine and Public Health
Kaitlin Ring
Department of Agricultural Sciences
University of Wisconsin- Madison
Care Management of Non-emergent Echocardiographic Diagnosis in Newborns
Background: Echocardiography is the primary tool used by clinicians to identify cardiovascular problems that need immediate attention in the newborn. More commonly, neonatal echocardiography identifies issues where the need for or timing of cardiology assessment is unclear.
Objective: The aim of this study is to identify the current practices of pediatric cardiologists regarding non-emergent findings on echocardiograms performed in the standard normal newborn nursery.
Methods: An e-mail invitation to participate in a survey on management of non-emergent neonatal echocardiographic findings was sent to the members of American Academy of Pediatrics Section on Cardiology and Cardiac Surgery and to the Pediheart on-line community. Participants were asked for their recommendation of care regarding ten non-emergent echocardiographic findings in an asymptomatic normal newborns,term newborn and whether their recommendations would change for an asymptomatic premature newborns born at 34 weeks gestation or an asymptomatic term baby , and newborns with trisomy 21. Options for follow-up included: Normal Newborn Care without further assessment (blue), Inpatient Cardiology Consultation (red), Repeat Echocardiography without Cardiology Consultation (yellow), Cardiology Consultation without Echocardiography (green), and Cardiology Consultation with Echocardiography
Results: We received 137 responses with interpretable data. This data for term newborns is shown in figure 1. 34% of providers would change their recommendations in the setting of prematurity and 47% would change their recommendations in the setting of trisomy 21 (Figures 2&3). In all settings, ongoing cardiology care was typically recommended for newborns with a 6 mm atrial septal defect, a ventricular septal defect or a bicuspid aortic valve. Ongoing care was rarely recommended for newborns with a patent foramen ovale or trivial mitral valve regurgitation.
Conclusion:
The overall findings of this survey shows variation in practitioners’ recommended level care in asymptomatic-newborns. With the exception of a patent foramen ovale or trivial mitral valve regurgitation, most practitioners feel that a follow up cardiology and echocardiography are appropriate.
Closing the Gap in Standardization of EMR Documentation in Children with Adrenal Insufficiency: 18 Month Follow Up
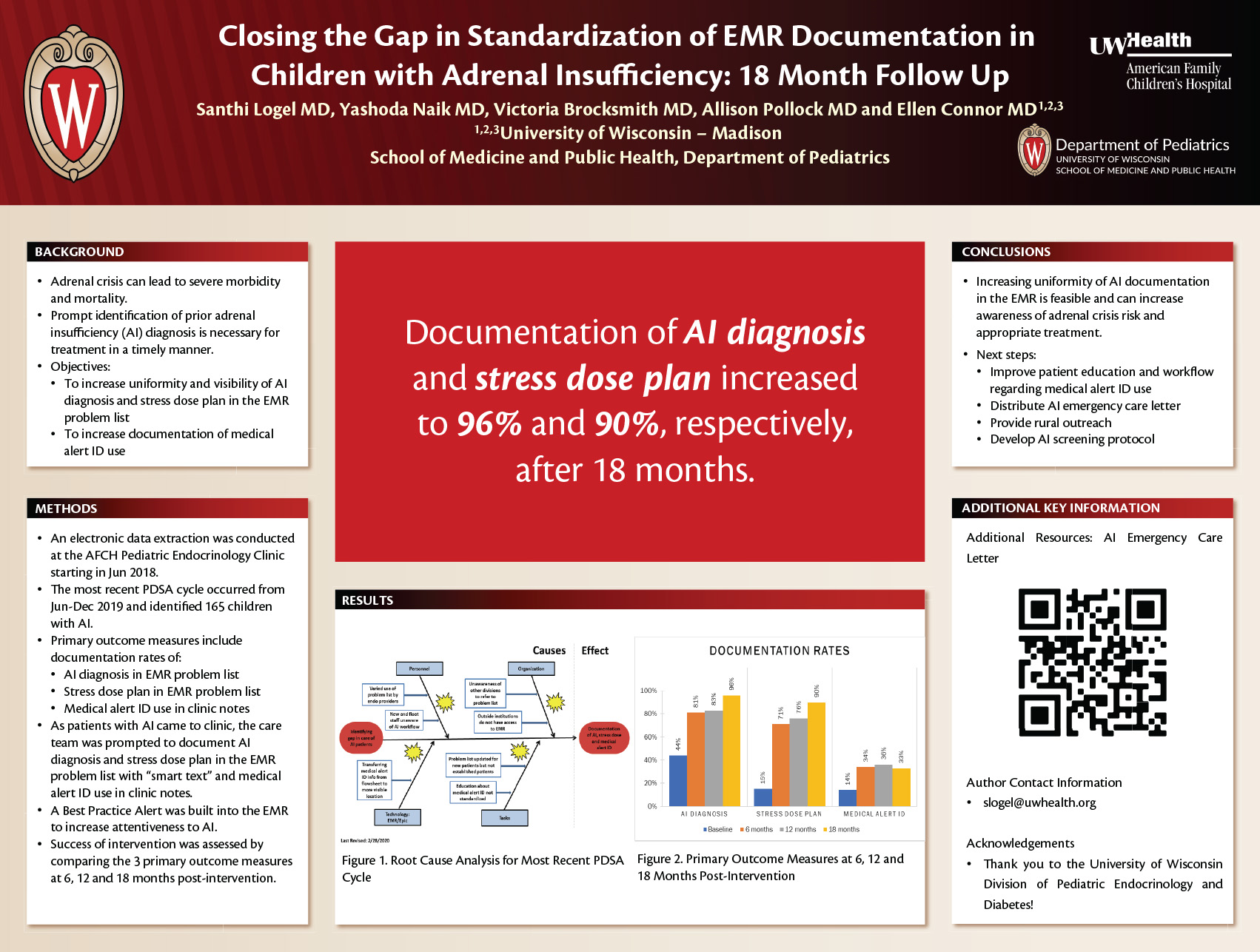
Click here for .pdf version of poster
Santhi Logel, MD, University of Wisconsin-Madison School of Medicine and Public Health, Madison, WI, United States; Yashoda Naik, MD, Marshfield Clinic Health Systems, Marshfield, WI, United States; Victoria Brocksmith, MD; Allison Pollock, MD; Ellen Connor, MD, University of Wisconsin-Madison School of Medicine and Public Health, Madison, WI, United States
Background
Adrenal crisis can lead to severe morbidity and mortality, particularly when treatment is delayed by lack of awareness of prior adrenal insufficiency (AI) diagnosis. Early recognition of AI is aided by clarity and uniformity of AI diagnosis documentation in the electronic medical record (EMR), a readily available stress dose plan for illness/injury and medical alert identification (ID).
Objective
This quality improvement (QI) project aimed to increase uniformity and visibility of AI diagnosis and stress dose plan in the EMR problem list and documentation of medical alert ID use.
Design/Methods
An electronic data extraction was conducted at the American Family Children’s Hospital Pediatric Endocrinology Clinic in Madison, WI from June-December 2019 and identified 165 children with AI. For those with AI, documentation rates of AI diagnosis and stress dose plan in the EMR problem list as well as medical alert ID use in clinic notes were collected and used as the 3 primary outcome measures. Root cause analysis was mapped (Figure 1) and metrics were determined to impact a change. As patients with AI came to clinic, the care team was prompted to document AI diagnosis and stress dose plan in the EMR problem list with “smart text” and medical alert ID use in clinic notes. Success of intervention was assessed by comparing the 3 primary outcome measures at 6, 12 and 18 months post-intervention.
Results
At baseline, 44% of patients with AI had documentation of this diagnosis and 15% had a stress dose plan in the EMR problem list. Documentation of medical alert ID use was present in 14% of patient charts. Documentation of AI diagnosis, stress dose plan in EMR problem list and medical alert ID use increased to 96%, 90% and 33% by 18 months, respectively (Figure 2).
Conclusion
Increasing uniformity of AI documentation in the EMR is feasible and can improve care for children with AI by increasing awareness of adrenal crisis risk and appropriate treatment. This QI project has now added a Best Practice Alert in the EMR and as a next step, education will be provided to patients regarding medical alert ID use and providers regarding documentation as part of our AI workflow. We have also created an AI emergency care letter to more easily identify and improve visibility of at-risk patients in outlying areas not able to access our EMR. Another next step of this QI project will involve geographic mapping of our patient population to better assess rural needs.
Session E: Translational Research – Blackboard Collaborate Session
This is an accordion element with a series of buttons that open and close related content panels.
Inflammatory and Iron-Related Indices Relate to Neonatal White Matter Microstructure
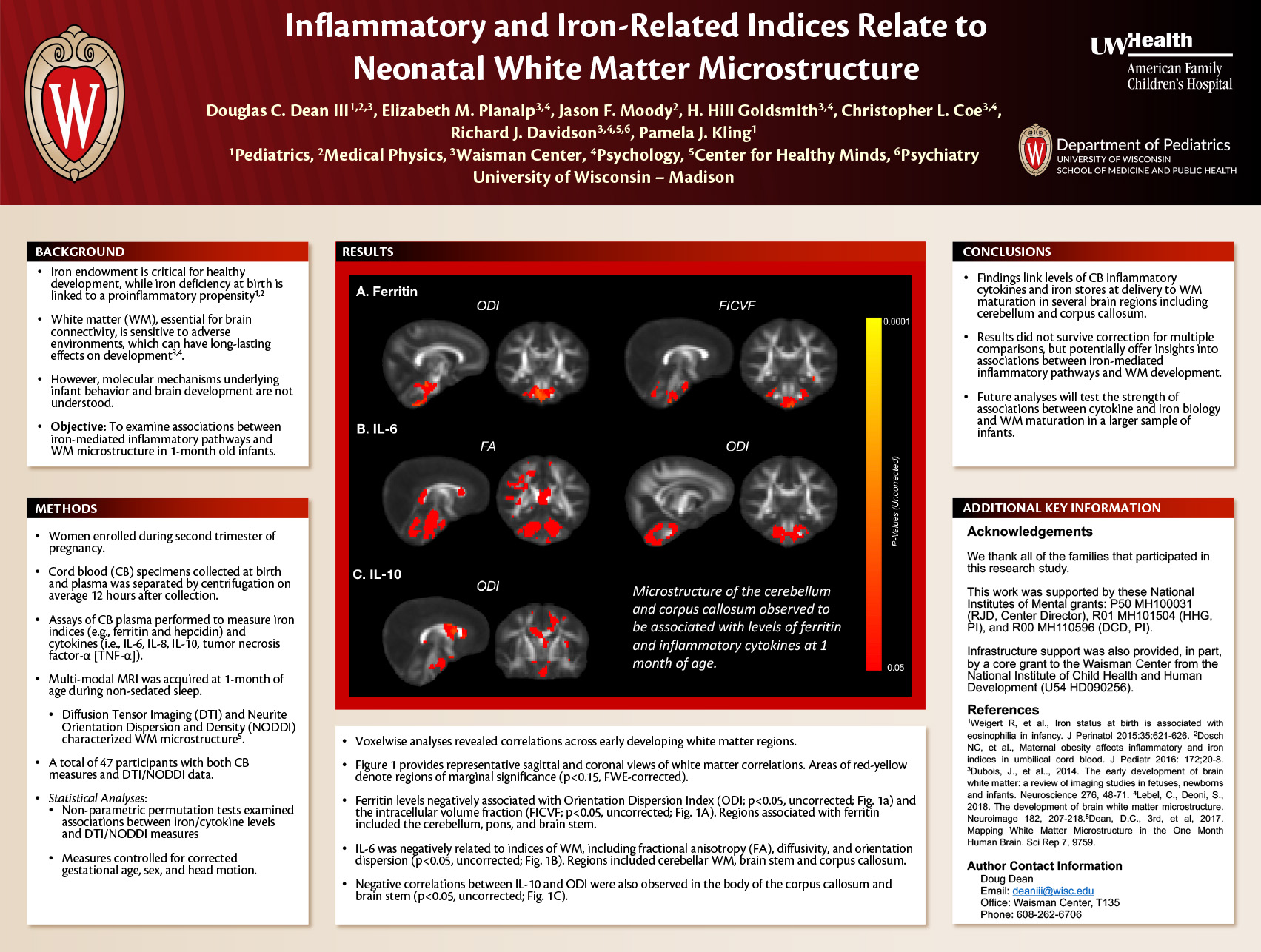
Click for .pdf version of poster
Authors: Douglas C. Dean III1,2,3, Elizabeth M Planalp3,4, Jason F. Moody2, HH Goldsmith3,4, Christopher L Coe3,4, Richard J Davidson3,4,5,6, Pamela J Kling1
1Department of Pediatrics, University of Wisconsin–Madison School of Medicine and Public Health, Madison, WI, USA
2Department of Medical Physics, University of Wisconsin–Madison School of Medicine and Public Health, Madison, WI, USA
3Waisman Center, University of Wisconsin–Madison, Madison, WI, USA
4Department of Psychology, University of Wisconsin–Madison, Madison, Wisconsin, USA.
5Center for Healthy Minds, University of Wisconsin–Madison, Madison, WI, USA
6Department of Psychiatry, University of Wisconsin–Madison School of Medicine and Public Health, Madison, WI, USA
Background: The prenatal environment plays a critical role in shaping infants’ early brain maturation. White matter (WM), essential for brain connectivity and function, undergoes rapid growth during the late stages of gestation and is sensitive to adverse prenatal environments, which can have long-lasting effects on subsequent neural and behavioral development. Inflammatory processes in the placenta and fetal compartment can influence early neurodevelopment; however, the extent of this influence on postnatal WM development still needs to be investigated further.
Objective: To investigate, for the first time, relations between inflammatory cytokines and iron-related indices at delivery and WM microstructure in 1-month old infants.
Design/Methods: We enrolled women during the second trimester of pregnancy and collected cord blood (CB) specimens at birth. Leukocytes and plasma were isolated on average 12 hours after collection. Assays of CB plasma were performed to measure iron indices (e.g., ferritin and hepcidin) and cytokines (i.e., IL-6, IL-8, IL-10, tumor necrosis factor-α [TNF-α]). Multi-modal MRI was acquired at 1-month of age during non-sedated sleep. Diffusion Tensor Imaging (DTI) and Neurite Orientation Dispersion and Density (NODDI) characterized WM microstructure. 47 participants usable CB measures and DTI/NODDI data. Non-parametric permutation tests examined associations between iron/cytokine levels and DTI/NODDI measures, controlling for gestational corrected age, sex, and head motion.
Results: Ferritin levels were negatively associated with WM measures of orientation dispersion and neurite density in the brain stem and cerebellum (p<0.05, uncorrected; Fig. 1a). IL6 was negatively related to indices of WM, including fractional anisotropy (FA), diffusivity, and orientation dispersion (p<0.05, uncorrected; Fig. 1b). Negative correlations between IL10 and orientation dispersion were also observed in the body of the corpus callosum (p<0.05, uncorrected; Fig. 1c).
Conclusion: Our preliminary findings suggest that the levels of CB inflammatory cytokines and iron stores at delivery are associated with WM maturation in several brain regions, including the cerebellum and corpus callosum. These results did not survive correction for multiple comparisons, but potentially offer new insights into prenatal factors that can influence early WM development. Future analyses will test the strength of these associations between cytokine and iron biology and WM maturation in a larger sample of infants.
Antitumor mechanisms of local radiation and combination immunotherapy in an immunologically cold model of neuroblastoma
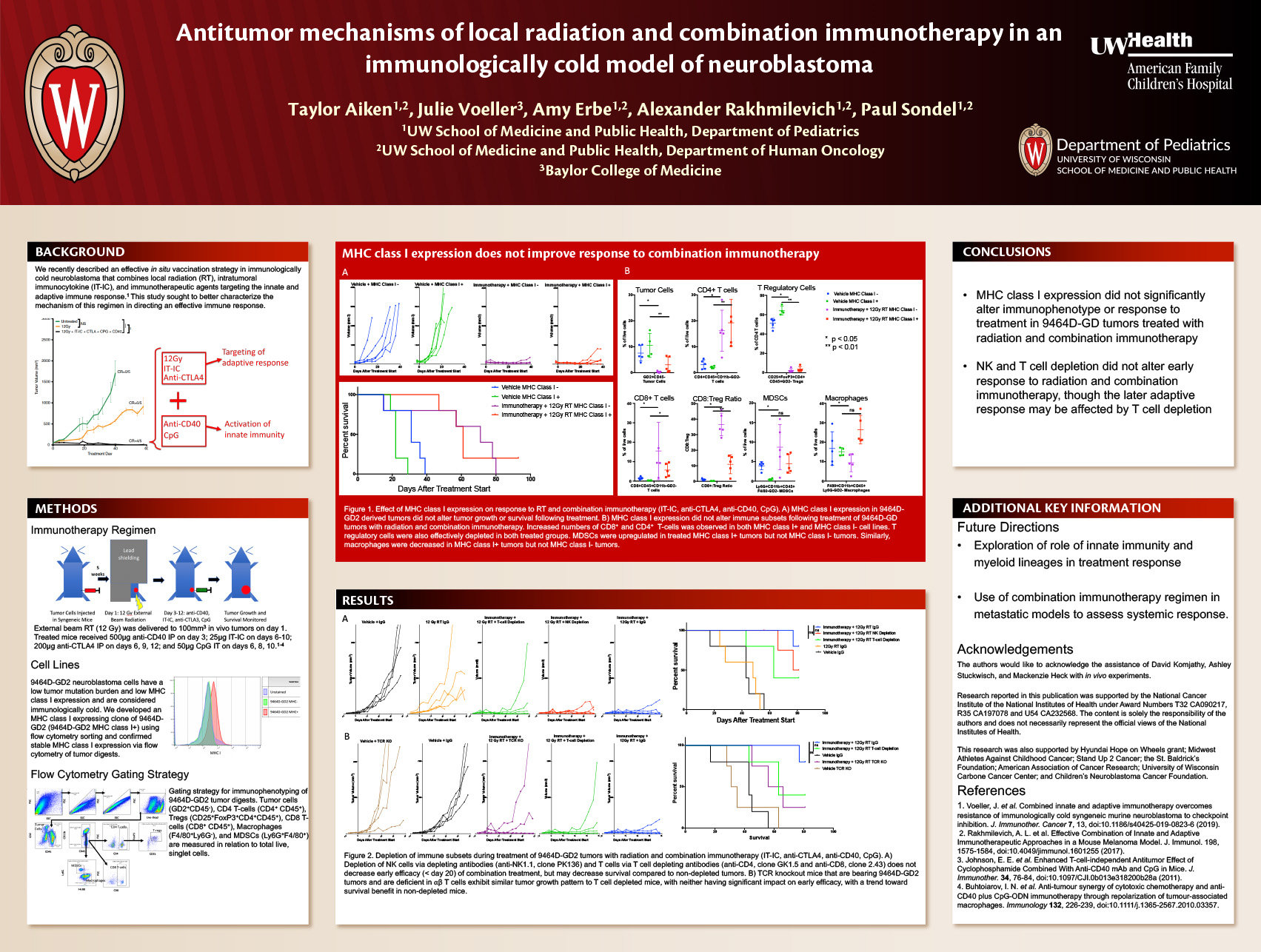
Click here for .pdf version of poster
Taylor Aiken, Julie Voeller, Amy Erbe-Gurel, Alexander Rakhmilevich, Paul Sondel
Introduction: The standard treatment for high-risk neuroblastoma includes a combination immunotherapeutic approach consisting of IL-2, GM-CSF, and monoclonal antibodies directed against GD2, a disialoganglioside preferentially expressed in neuroblastoma and melanoma. We recently described an effective preclinical in-situ vaccination strategy combining local radiation therapy (RT), intratumoral immunocytokine (IT-IC) which is IL-2-linked to anti-GD2 monoclonal antibody, checkpoint inhibition (anti-CTLA4), and drivers of innate immunity (anti-CD40 and CpG). Here we describe further mechanistic evaluation of this combination regimen in an immunologically cold model of neuroblastoma.
Methods: Mice bearing GD2-expressing neuroblastoma tumors (9464D-GD2) were treated with 12Gy RT and combination immunotherapy (IT-IC, anti-CTLA-4, CpG, anti-CD40) over 12 days. MHC class I positive and negative 9464D-GD2 cell lines were developed by flow cytometry sorting. Depletion of individual immune cell sets was achieved by depleting monoclonal antibodies and confirmed by flow cytometry. T-cell receptor deficient (TCR KO) mice were used to confirm findings in T-cell depletion experiments. Tumor growth and animal survival were assessed following treatment. Immune cell infiltrate was assessed in some mice by flow cytometry immediately following treatment.
Results: MHC class I expression did not slow untreated tumor growth or improve survival in mice bearing 9464D-GD2 tumors following treatment with RT and combination immunotherapy. MHC class I expression also did not alter individual immune cell subsets in treated tumors. Overall, increased infiltration of CD8 T-cells, CD4 T-cells, and deletion of T regulatory cells was observed in all treated tumors (p<0.05). The effectiveness of RT and combination immunotherapy was not completely abrogated by NK or T cell depletion, and TCR KO mice had similar tumor growth and survival to mice that underwent T-cell depletion.
Conclusions: Treatment with RT and combination immunotherapy (IT-IC, anti-CTLA4, anti-CD40, CpG) may act through mechanisms that are MHC class I, NK-cell and T-cell independent. Further investigation of the role of innate immunity and myeloid subsets in this scenario is warranted.
Association between gestational age adjusted TSH percentiles and neurodevelopmental outcomes among preterm infants
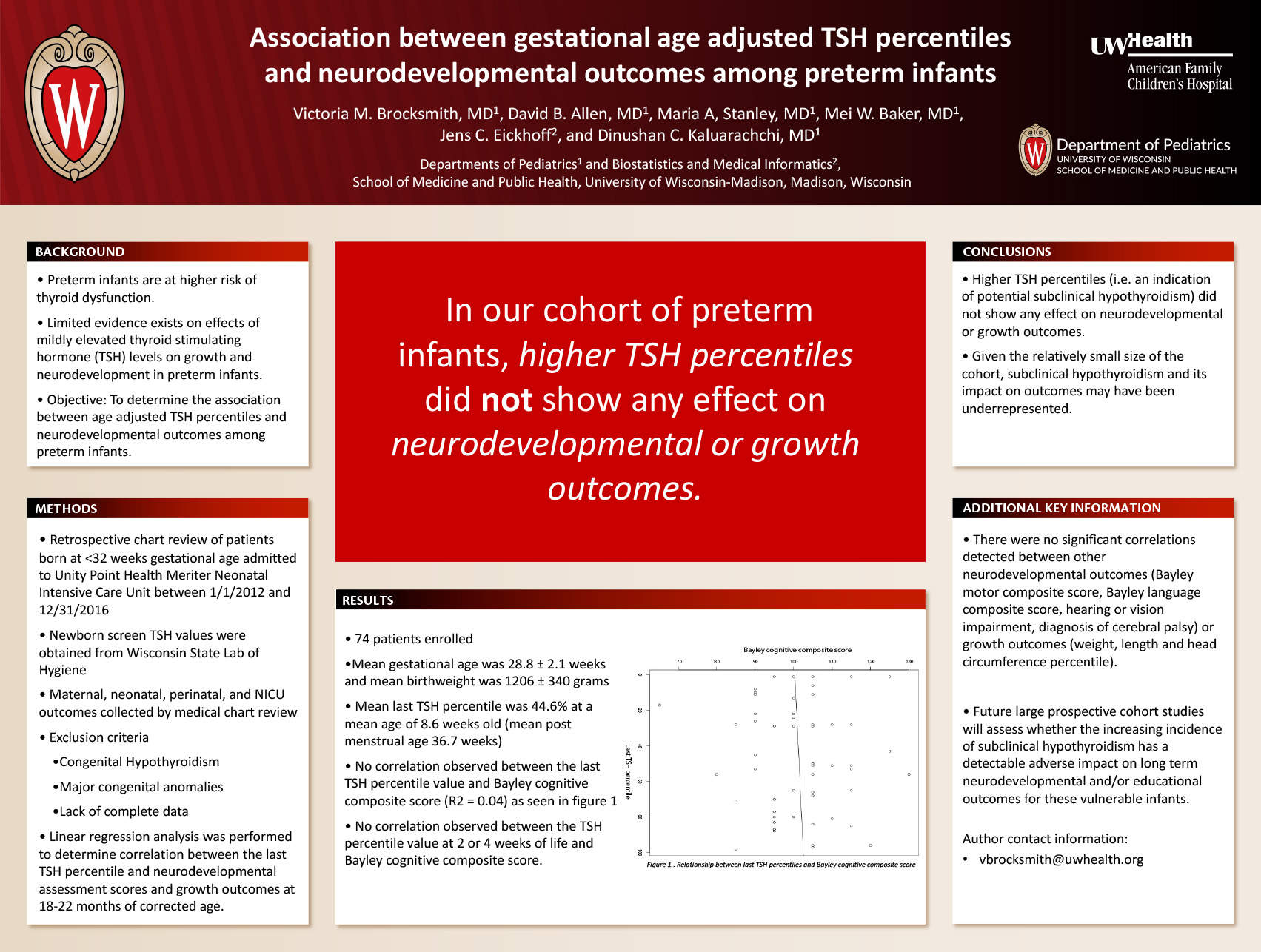
Click here for .pdf version of poster
Victoria M. Brocksmith1, David B. Allen1, Maria A. Stanley1, Mei W. Baker1, Sandra J. Dawe2, Jens C. Eickhoff2, Dinushan C. Kaluarachchi1
Institutions: 1. University of Wisconsin, Madison, WI, United States. 2. Biostatistics & Medical Informatics, University of Wisconsin-Madison, Madison, WI, United States.
Background
Preterm infants are at higher risk of thyroid dysfunction. One pattern of thyroid dysfunction is subclinical hypothyroidism (SCH) defined by elevated thyroid stimulating hormone (TSH) level and a normal serum free T4 level. Limited evidence exists on the effects of mildly elevated TSH levels on growth and development in preterm infants. The objective of this study was to determine the association between the age adjusted TSH percentiles and neurodevelopmental outcomes among preterm infants.
Methods
A retrospective review of patients born at < 32 weeks of gestation and admitted to Unity Point Health neonatal intensive care unit (NICU) from January 01, 2012 to December 31, 2016 was performed. Infants with a diagnosis of congenital hypothyroidism, major congenital anomalies, and incomplete data due to death or lack of neurodevelopmental assessment at 18-22 months were excluded. Serial newborn screening TSH values were obtained from the Wisconsin State Lab of Hygiene. Linear regression analysis was conducted to determine correlation between the last newborn screen TSH percentile collected prior to discharge from the NICU and neurodevelopmental assessment scores at 18 to 22 months of corrected gestational age.
Results
Seventy-four patients were enrolled in the study for whom the mean gestational age was 28.8 ± 2.1 weeks and mean birthweight was 1206 ± 340 grams. Mean last TSH percentile was 44.6% at a mean of 8.6 weeks of life (mean post menstrual age 36.7 weeks). There was no correlation observed between the last TSH percentile value and Bayley cognitive composite score (R2 = 0.04). Furthermore, there were no significant correlations detected between other neurodevelopmental outcomes (Bayley motor composite score, Bayley language composite score, hearing or vision impairment, diagnosis of cerebral palsy or growth outcomes (weight, length and head circumference percentile).
Conclusions
In our cohort of preterm infants, higher TSH percentiles (i.e. an indication of potential subclinical hypothyroidism) did not show any effect on neurodevelopmental or growth outcomes. However, given the relatively small size of the cohort, subclinical hypothyroidism and its impact on outcomes may have been underrepresented. Future large prospective cohort studies will assess whether the increasing incidence of subclinical hypothyroidism is having a detectable adverse impact on long term neurodevelopmental and/or educational outcomes for these vulnerable infants.
Gastrointestinal Parasites in Hispanic Immigrants
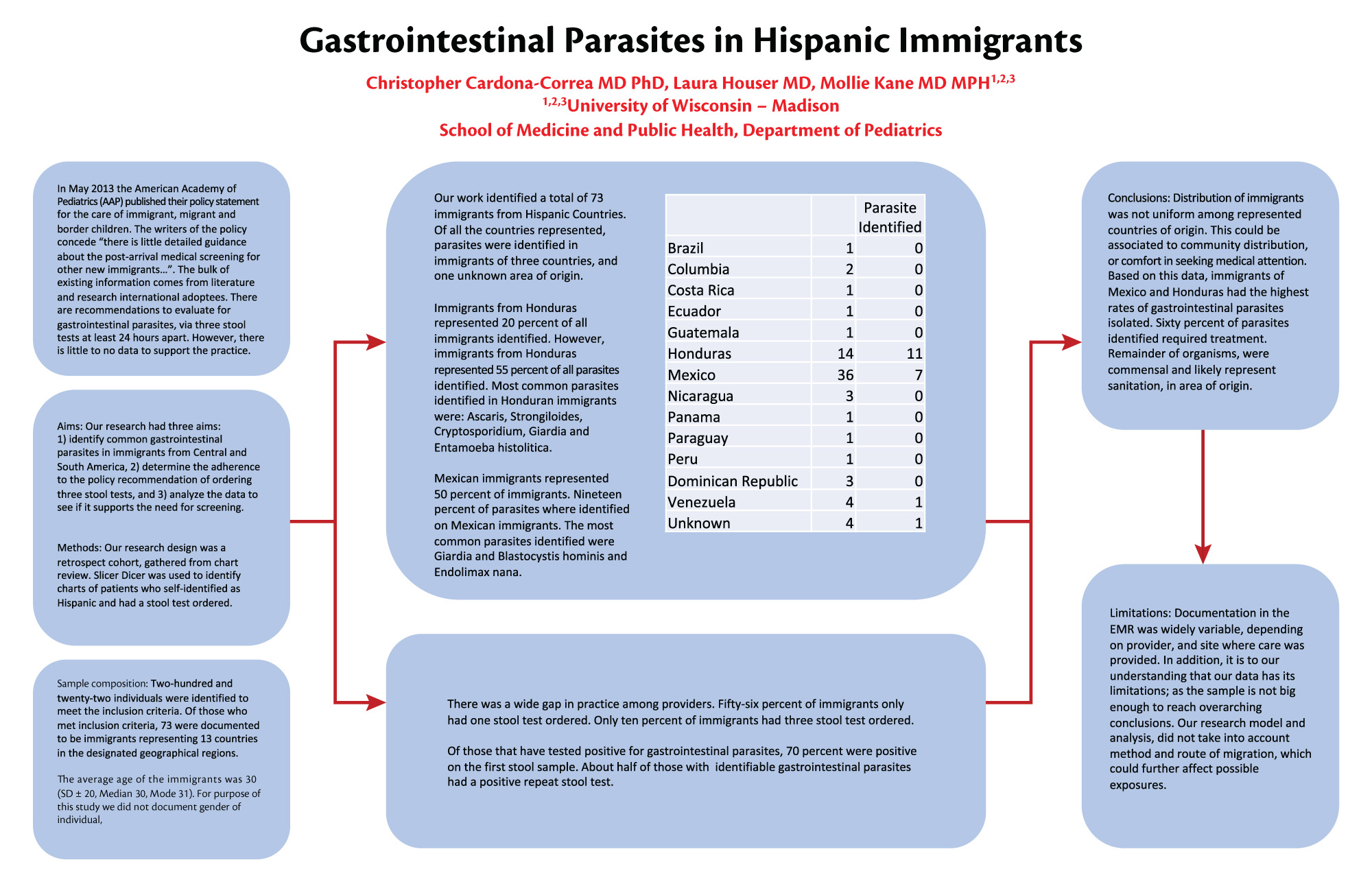
Click here for .pdf version of poster
Christopher Cardona-Correa MD PhD, Laura Houser MD, Mollie Kane MD
Background: In May 2013 the American Academy of Pediatrics (AAP) published their policy statement for the care of immigrant, migrant and border children. The writers of the policy concede “there is little detailed guidance about the post-arrival medical screening for other new immigrants…”. The bulk of existing information comes from literature and research international adoptees. There are recommendations to evaluate for gastrointestinal parasites, via three stool tests at least 24 hours apart. However, there is little to no data to support the practice.
Aims: Our research had three aims: 1) identify common gastrointestinal parasites in immigrants from Central and South America, 2) determine the adherence to the policy recommendation of ordering three stool tests, and 3) analyze the data to see if it supports the need for screening.
Results: Our research design was a retrospect cohort, gathered from chart review. Slicer Dicer was used to identify charts of patients who self-identified as Hispanic and had a stool test ordered. Two-hundred and twenty-two individuals were identified to meet the inclusion criteria. Of those who met inclusion criteria, 73 were documented to be immigrants representing 13 countries in the designated geographical regions. Twenty individuals had gastrointestinal parasites identified in stool samples. Data analysis is ongoing.
Conclusion: Initial medical encounters for immigrant families are stressful for families and providers, as they aim to tackle an extensive checklist of recommended health maintenance and screening practices in addition to other medical concerns. This work could guide the screening practices of gastrointestinal parasites, and as such streamline such encounters.
Maternal Stress And Depression Associations With Respiratory Viral Illnesses And Respiratory Phenotypes
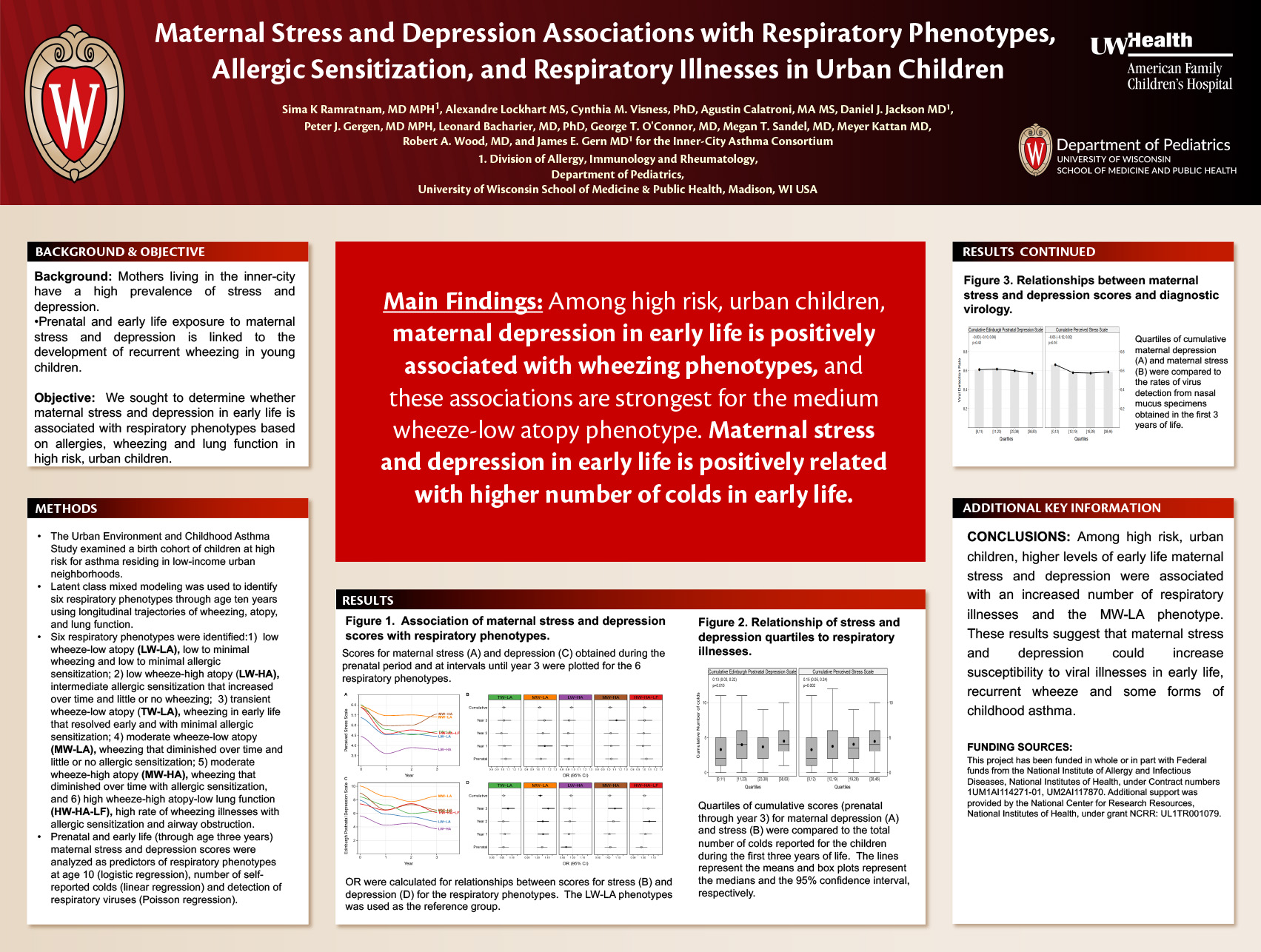
Click here for .pdf version of poster
K. Ramratnam1, A. Lockhart2, C. Visness3, A. Calatroni2, D. J. Jackson4, P. J. Gergen5, L. B. Bacharier6, G. T. O’Connor7, M. Sandel8, M. Kattan9, R. Wood10, J. E. Gern11; 1Pediatrics, University of Wisconsin-Madison School of Medicine and Public Health, Madison, WI, United States, 2Rho, Inc, Chapel Hill, NC, United States, 3Rho, Inc., Chapel Hill, NC, United States, 4Univ of Wisconsin, Madison, WI, United States, 5AAABB DAIT NIAID NIH, Rockville, MD, United States, 6St Louis Childrens Hosp, Saint Louis, MO, United States, 7Pulm Ctr, Boston Univ Sch of Med, Boston, MA, United States, 8Medicine, Boston University School of Medicine, Boston, MA, United States, 9Columbia Univ Med Ctr, New York, NY, United States, 10Pediatrics, Johns Hopkins School of Medicine, Baltimore, MD, United States, 11Univ of Wisconsin – Madison, Madison, WI, United States.
RATIONALE: Prenatal and early life exposure to maternal stress and depression is linked to the development of recurrent wheezing in young children. We sought to determine whether maternal stress and depression in early life is associated with respiratory phenotypes in urban children.
METHODS: The Urban Environment and Childhood Asthma Study examined a birth cohort of children at high risk for asthma residing in low-income urban neighborhoods. Latent class mixed modeling was used to identify six respiratory phenotypes through age ten years using longitudinal trajectories of wheezing, atopy, and lung function. Prenatal and early life (through age three years) maternal stress and depression scores were analyzed as predictors of respiratory phenotypes at age 10 (logistic regression), number of self-reported colds (linear regression) and detection of respiratory viruses (Poisson regression).
RESULTS: Scores for maternal stress and depression were positively related to multiple wheezing phenotypes. In particular, cumulative measures of maternal depression in the first three years were related to the medium wheeze-low atopy (MW-LA) phenotype (OR=1.03; [1.01, 1.05]; p<0.01, Figure). Considering indicators of respiratory health through age 10, there were multiple positive associations between early life scores for maternal stress and depression and trajectories of wheezing illnesses, but no consistent relationships with lung function and inverse relationships with the development of allergen specific IgE. Cumulative maternal stress and depression scores were associated with cumulative number of colds through age 3.
CONCLUSIONS: Among high risk, urban children, higher levels of early life maternal stress and depression were associated with an increased number of respiratory illnesses and the MW-LA phenotype. These results suggest that maternal stress and depression could increase susceptibility to viral illnesses in early life, recurrent wheeze and some forms of childhood asthma.
Are We What We Eat?: Identifying Microbial Communities of Fruits and Vegetables
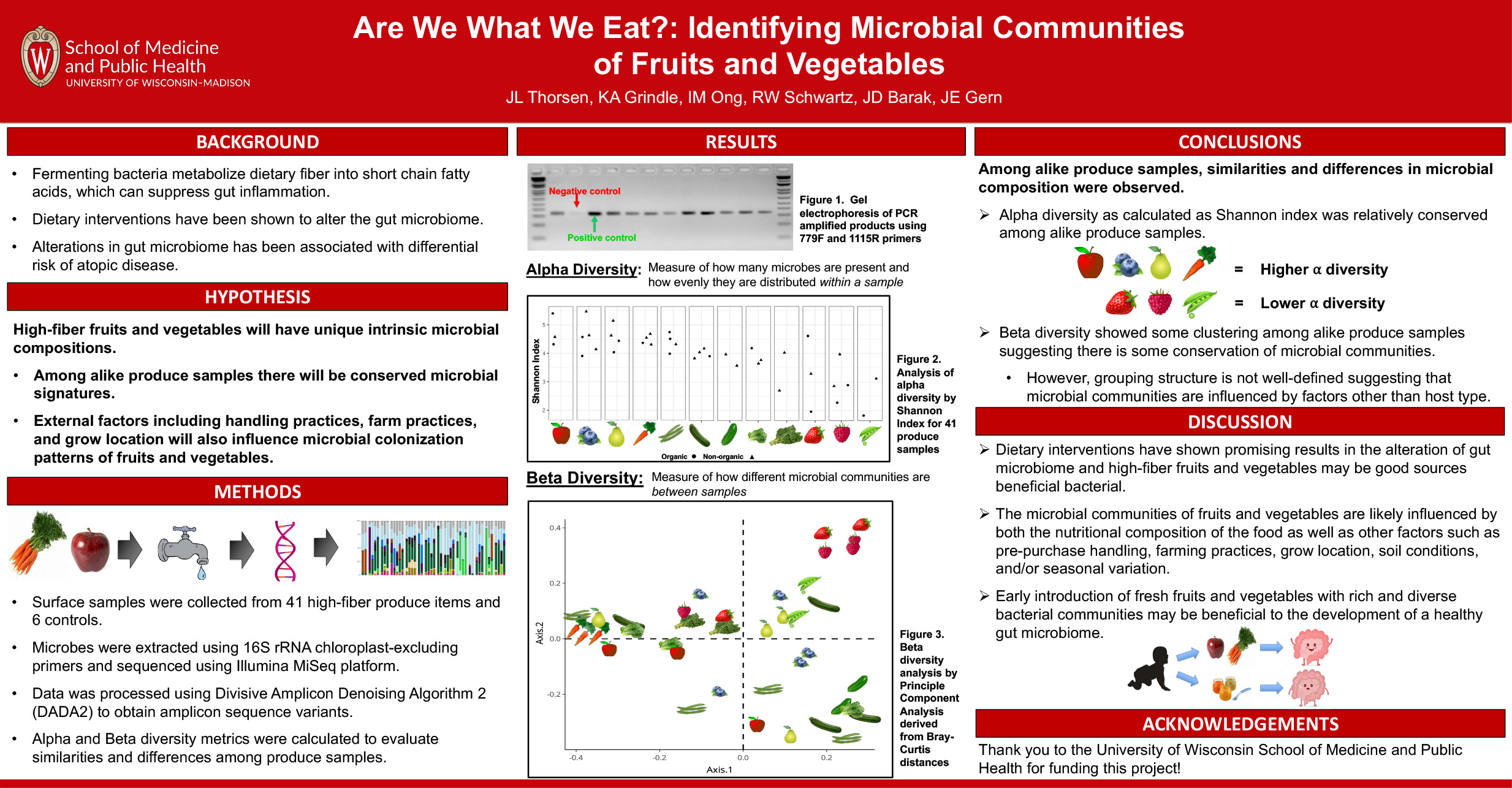
Click here for .pdf version of poster
Julia Thorsen; Kristine Grindle; Irene Ong; Jeri Barak; James E. Gern
Rationale: Diet can alter the gut microbiome and possibly the risk of atopic disease. Fermenting bacteria can metabolize dietary fiber into short-chain fatty acids, which can suppress gut inflammation and atopy. We hypothesize that high-fiber fruits and vegetables will have unique intrinsic microbial compositions related to their nutritional composition and could be sources of beneficial bacteria for the gut.
Methods: Surface samples were collected from 41 fresh, store-purchased produce items and 6 controls. Produce-associated microbes were extracted and amplified using 16S rRNA chloroplast-excluding primers and sequenced using Illumina MiSeq platform. DNA sequencing data was processed using Divisive Amplicon Denoising Algorithm 2 (DADA2) to obtain amplicon sequence variants (ASV). Alpha and Beta diversity metrics were calculated to evaluate similarities and differences among produce samples.
Results: Apple, blueberry, pear, carrot, and green bean had the highest microbial diversity (Shannon indices: 3.57-5.47). Snap pea and raspberry had the lowest microbial diversity (Shannon indices: 1.82-3.97). Beta diversity analysis revealed similar microbial communities between some alike produce samples (carrots, raspberries) as well as differences in microbial communities between alike produce samples (green beans). Among samples with high microbial diversity, abundant phyla included proteobacterium and firmicutes.
Conclusions: Among alike produce samples, similarities and differences in microbial composition were observed. Alpha diversity as calculated as Shannon index was relatively conserved among alike produce samples. Beta diversity showed some clustering among alike produce samples suggesting there is some conservation of microbial communities. However, beta diversity grouping structure is not well-defined. The microbial communities of fruits and vegetables are likely influenced by both the nutritional composition of the food as well as other factors such as pre-purchase handling, farming practices, grow location, soil conditions, and/or seasonal variation.
MRI Markers of Outcome after Severe Pediatric TBI
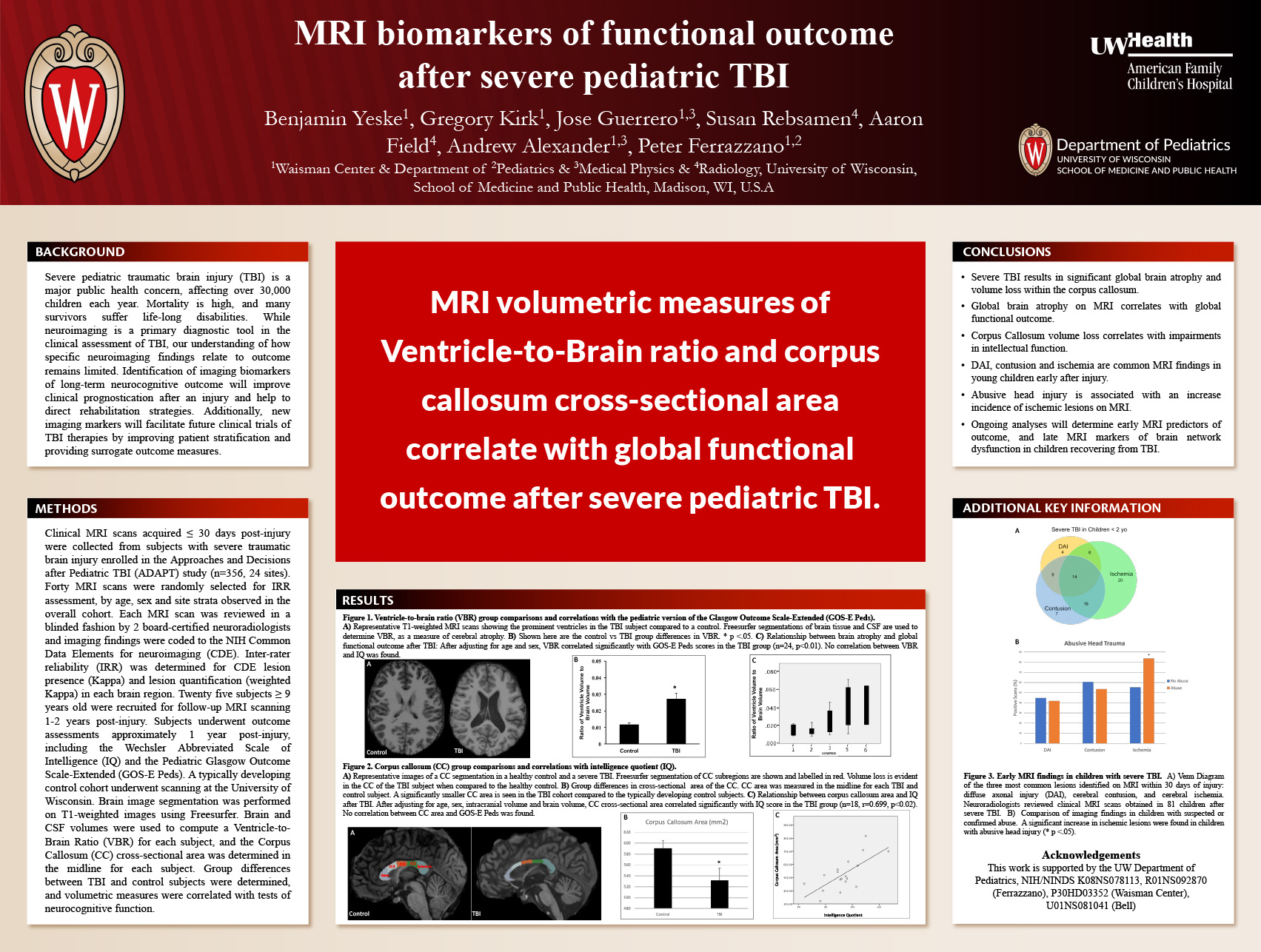
Click here for .pdf version of poster
Authors: Ben Yeske, Gregory Kirk, Jose Guerrero, Andy Alexander, Peter Ferrazzano
Background: Severe pediatric traumatic brain injury (TBI) is a major public health concern, affecting over 30,000 children each year. Mortality is high, and many survivors suffer life-long disabilities. While neuroimaging is a primary diagnostic tool in the clinical assessment of TBI, our understanding of how specific neuroimaging findings relate to outcome remains limited. Identification of imaging biomarkers of long-term neurocognitive outcome will improve clinical prognostication after an injury and help to direct rehabilitation strategies.
Methods: Clinical MRI scans acquired ≤ 30 days post-injury were collected from subjects with severe traumatic brain injury enrolled in the Approaches and Decisions after Pediatric TBI (ADAPT) study (n=356, 24 sites). Forty MRI scans were randomly selected for Inter- and Intra-rater reliability assessment. Each MRI scan was reviewed in a blinded fashion by 2 board-certified neuroradiologists and imaging findings were coded to the NIH Common Data Elements for neuroimaging (CDE). Twenty five subjects ≥ 9 years old were recruited for follow-up MRI scanning 1-2 years post-injury. Subjects underwent outcome assessments approximately 1 year post-injury, including the Wechsler Abbreviated Scale of Intelligence (IQ) and the Pediatric Glasgow Outcome Scale-Extended (GOS-E Peds). A typically developing control cohort underwent scanning at the University of Wisconsin. Brain image segmentation was performed on T1-weighted images using Freesurfer. Brain and CSF volumes were used to compute a Ventricle-to-Brain Ratio (VBR) for each subject, and the Corpus Callosum (CC) cross-sectional area was determined in the midline for each subject. Group differences between TBI and control subjects were determined, and volumetric measures were correlated with tests of neurocognitive function.
Results: Overall, 59% of children admitted to participating sites with severe TBI during the study period underwent MRI scanning during the first 30 days post-injury, and no differences in injury severity or presenting GCS were found between imaged and non-imaged TBI patients. Children who had an MRI were younger (5.7 vs. 8.18 years, p=0.03) and had longer ICU stays (22.13 vs. 11.41 days, p<0.001) compared to the non-imaged TBI cohort. Median time from injury to MRI scanning was 5.71 days, and at the time of MRI scanning many children were still receiving intensive therapies and monitoring, including mechanical ventilation (94%) and vasoactive infusions (39%). IRR for presence/absence and quantification of lesions was moderate to excellent across brain regions and lesion types. On follow-up MRI, the TBI group demonstrated higher VBR and lower CC area compared to the control cohort. After adjusting for age and sex, VBR correlated significantly with GOS-E Peds score in the TBI group (n=24, p<0.01). After adjusting for age, sex, intracranial volume and brain volume, CC cross-sectional area correlated significantly with IQ score in the TBI group (n=18, p<0.02).
Conclusion: MRI is frequently performed in children with severe TBI, often within days of injury. We found acceptable inter-rater reliability of most CDEs in clinical MRI scans acquired early after injury in children with severe TBI. Analysis of the entire cohort of clinical scans is now underway to identify MRI predictors of neurocognitive outcome after TBI. At 1-2 years post-injury, the MRI volumetric measures of ventricle-to-brain ratio and corpus callosum cross sectional area are markers of global cognitive function in children recovering from severe TBI. Ongoing analyses will determine regional brain volumes, and MRI measures of structural and functional brain network connectivity, to identify markers of specific neurocognitive dysfunction after TBI.
Prophylactic Peritoneal Drainage Improves Fluid Output after Congenital Heart Surgery
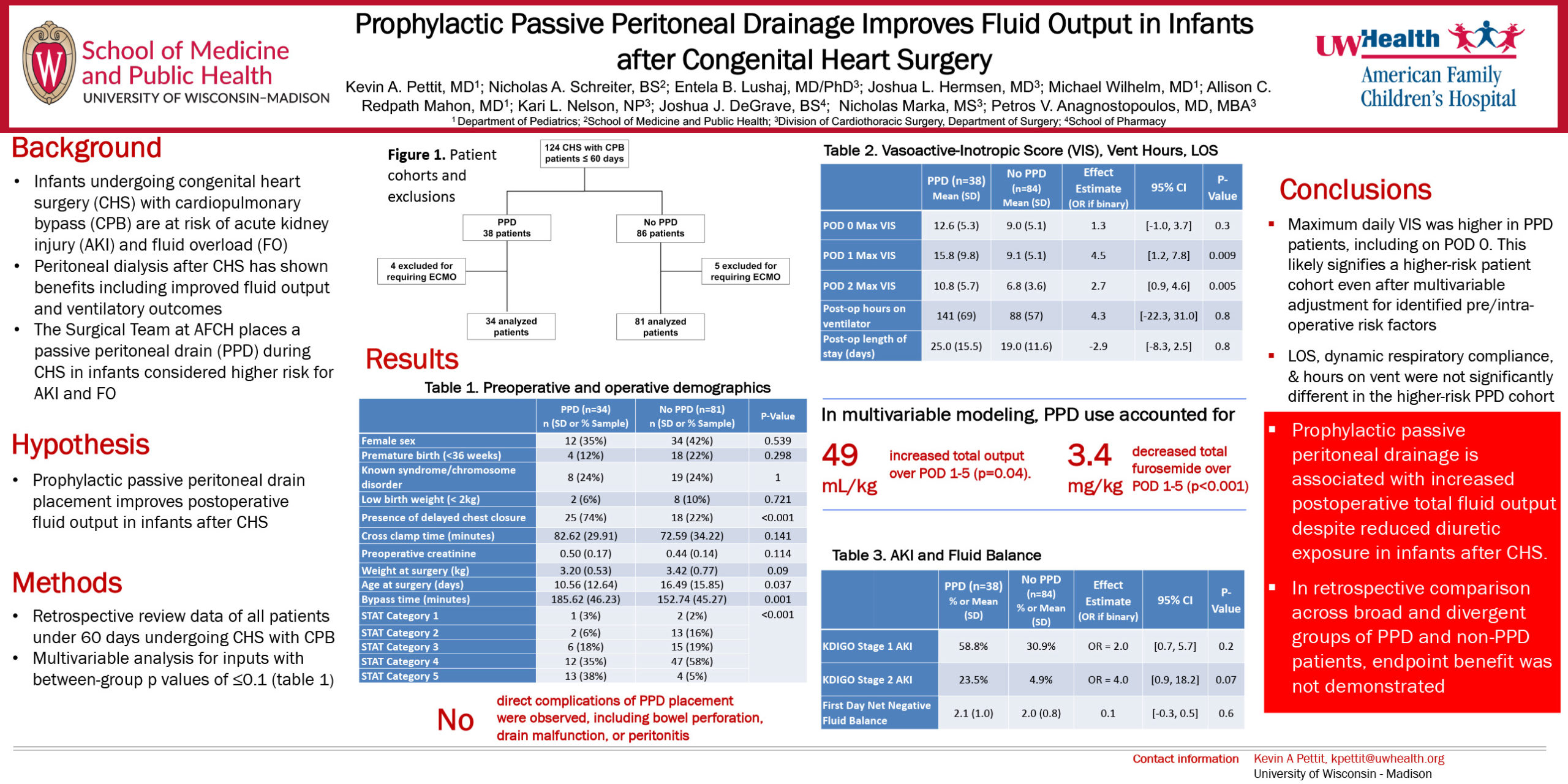
Click here for .pdf version of poster
Authors: Kevin A. Pettit, MD1; Nicholas A. Schreiter, BS2; Entela B. Lushaj3, MD/PhD; Joshua L. Hermsen, MD3; Michael Wilhelm, MD1; Allison C. Redpath Mahon1, MD; Kari L. Nelson, NP3, Joshua J. DeGrave, BS4; Nicholas Marka, MS3; Petros V. Anagnostopoulos, MD, MBA3
The American Family Children’s Hospital, University of Wisconsin Hospital and Clinics
1675 Highland Ave, Madison, WI 53792
1 Department of Pediatrics; 2School of Medicine and Public Health; 3Division of Cardiothoracic Surgery, Department of Surgery; 4School of Pharmacy
Background: Infants undergoing congenital heart surgery (CHS) with cardiopulmonary bypass (CPB) are at risk of acute kidney injury (AKI) and fluid overload. When used for dialysis after cardiac surgery, peritoneal catheters pose a low risk to the patient and have demonstrated benefits including reduced time to net-negative fluid balance and reduced ventilator hours. It is unclear whether the placement of passive peritoneal drains (PPDs) carry similar benefits, as small studies with dissimilar cohorts have yielded disparate results across different measures.
Objective: We hypothesized that PPD placement improves postoperative fluid output in high-risk infants after CHS. Our aim was to assess the effect of PPD placement on fluid management in these patients.
Methods: We analyzed 115 consecutive patients, age birth to 60 days, admitted to the PICU after CHS with CPB between 2012 and 2018. Patients who needed postoperative ECMO were excluded. Linear and logistic regression models compared postoperative fluid balances, diuretics administration, AKI, vasoactive-inotropic scores (VIS), time intubated, and length of stay after adjusting for pre/operative predictors including STAT category, bypass time, age, weight, and open chest status.
Results: PPD patients had higher STAT category (p=0.001), longer CPB times (p=0.001), and higher VIS on POD 1-3 (p≤0.005 daily). PPD patients also had higher AKI rates (p=0.01) that did not reach significance in multivariable modeling. There were no postoperative deaths. Postoperative hours of intubation, hospital length of stay, and POD 1-5 fluid intake did not differ between groups. Over POD 1-5, PPD use accounted for 48.8 mL/kg increased fluid output (95% CI [2.2, 95.4], p=0.043) and 3.41 mg/kg less furosemide administered (95% CI [1.69, 5.14], p<0.001). No PPD complications were observed.
Conclusions: Although PPD placement did not affect end-outcomes, it was used in higher acuity patients. PPD placement allows improved fluid output with lower diuretic administration and may be a useful postoperative fluid management adjunct in some complex CHS patients.
Predictors of Outcomes for Small for Gestational Age Neonates in the NICU
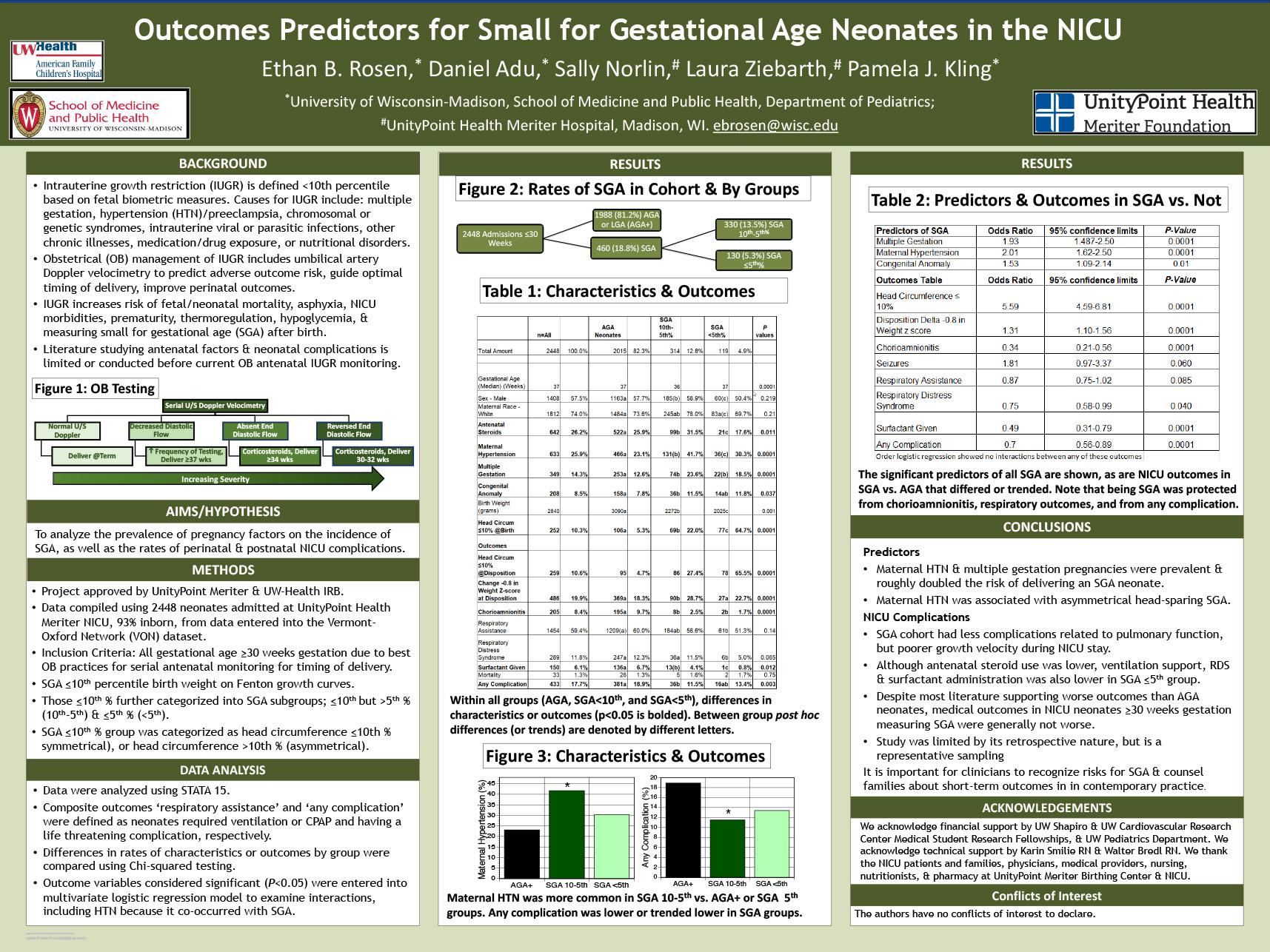
Click here for .pdf version of poster
Ethan B. Rosen, Daniel Adu, Sally Norlin, Laura Ziebarth, Pamela J. Kling
University of Wisconsin and UnityPoint Health Meriter, Madison WI
Background: Neonates born small for gestational age (SGA), are at-risk for developing many acute NICU complications, as well as chronic developmental issues. SGA is defined as body weight below <10th percentile for gestational age using the Fenton growth curve. Maternal hypertension (Htn), multiple gestation pregnancies, birth defects and congenital infections are all associated with neonatal SGA. Complications associated with SGA have historically included delayed transition, lower APGAR scores, respiratory support, poor growth, longer inpatient stays, and higher mortality. However, with current at-risk antenatal clinic monitoring practices of growth-restricted fetuses, predictors of postnatal outcomes in SGA neonates are poorly understood. Objective: To examine pregnancy factors to outcomes in SGA neonates in the NICU. Methods: A retrospective cohort study of our local NICU Vermont Oxford Network neonatal characteristics and outcome data from 2015 through 2018 was performed. Three groups were studied; AGA using > 10th using Fenton curve; 5th-10th percentile SGA or <5th percentile SGA. Both categorical and continuous data were analyzed. Neonates <30 weeks gestational age were excluded from the primary analysis due to best obstetrician practices in delaying SGA births to at least 30 weeks. Results: Of 2350 NICU admissions born ≥30 weeks, 18.8% were SGA <10th, with 13.5% between the 5-10th and 5.3% <5th percentile. 25% of SGA pregnancies experienced Htn. In both SGA <5% and SGA <10% groups, Htn predicted head circumferences at birth <10th percentile (p<0.005). In the SGA <5th group, Htn also predicted home O2 need (6.67% vs 1.42% in AGA, p<0.035). In survivors, chronic lung disease, infections, and extreme length of stay did not differ between groups. Death or morbidity did not differ between groups. Conclusions: In the NICU, being SGA <10th is common, but most are between the 5th-10th percentile and have better outcomes than those <5th percentile. It would be important to recognize and counsel families about NICU outcomes in contemporary practice.
Point-of-Care Lung Ultrasound to Diagnose the Etiology of Acute Respiratory Failure in the Pediatric Intensive Care Unit
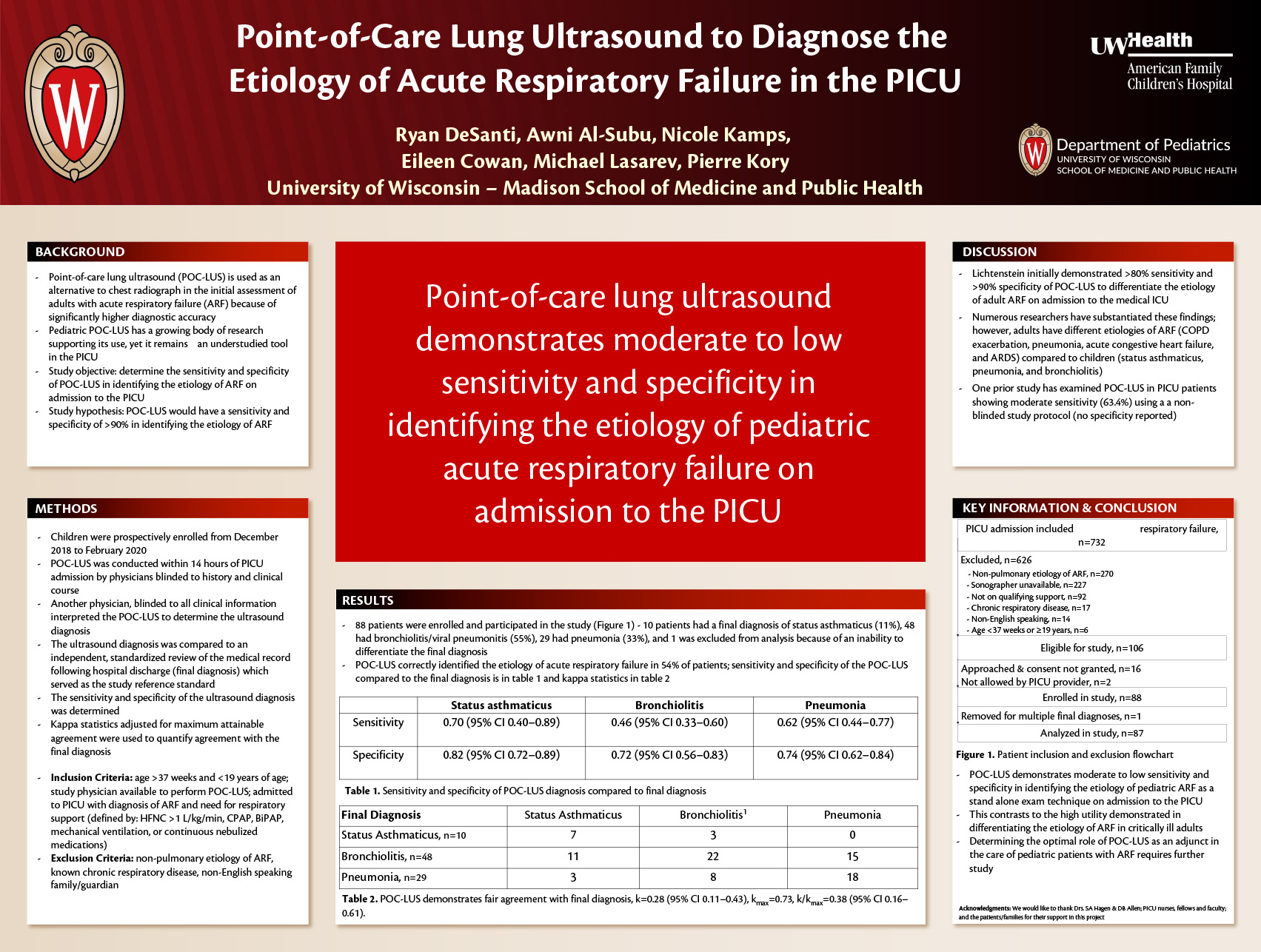
Click here for .pdf version of poster
Authors: Ryan L DeSanti, Pierre Kory, Eileen Cowan, Michael Lasarev, Awni M Al-Subu
Background: Point-of-care lung ultrasound (POC-LUS) is a non-invasive, safe imaging technology that can be used to rapidly and accurately differentiate the most common causes of acute respiratory failure (ARF) in adults. Despite widespread implementation, there remains a paucity of data supporting its use and training in pediatric critical care. Our objective was to determine the inter-rater reliability of ultrasound interpretation in pediatric ARF among intensivists trained and experienced in POC-LUS.
Methods: This was a planned secondary analysis of an observational study of children admitted to a 21-bed PICU undergoing POC-LUS for the evaluation of ARF. A three zone per hemi-thorax POC-LUS exam was conducted on admission by intensivists with focused ultrasound training. For each zone, an assessment of lung sliding, pleural line characteristics, and ultrasound artifacts was made. Findings were grouped into patterns correlating with discrete diagnoses of pediatric ARF. An intensivist experienced in POC-LUS, blinded to all clinical information, interpreted the trainee examination. Kappa statistics were used to determine provider agreement in the interpretation of ultrasound findings. Final patient diagnosis was determined by a blinded review of the chart following hospital discharge.
Results: Three trainees performed POC-LUS on 50 patients examining 6 zones per patient (300 total). The cohort included 6 (12%) patients with status asthmaticus, 28 (56%) with bronchiolitis, and 16 (32%) with pneumonia. There was moderate agreement between trainee and expert derived diagnoses at 60% (K=0.56, CI 0.031 – 0.80). Evaluation of the presence of lung sliding (K=-0.029; CI -0.045 – -0.012) and the presence of a normal pleural line (K=0.282; CI 0.087 – 0.476) was low. Interpretation of ultrasound artifacts ranged from moderate to high (K=0.452; CI 0.154 – 0.758 for pleural effusions to K=0.648; CI 0.550 – 0.736 for presence of A-lines).
Conclusions: There is moderate agreement between pediatric intensivists training in POC-LUS and an expert intensivist. While the body of data supporting the evaluation of adult patients with POC-LUS should not be extrapolated to pediatrics, this study adds to the limited evidence supporting point-of-care ultrasound training in the PICU.