Fifteen months ago, associate professor (CHS) and pediatric cardiac electrophysiologist Nicholas Von Bergen, MD, joined the UW Department of Pediatrics faculty after having served as a visiting professor for the previous four years.
His presence has enabled the pediatric EP program at American Family Children’s Hospital (AFCH) to nearly double its clinical volume. He also maintains a thriving outreach program and is investigating new ways to improve outcomes for children with arrhythmias.
Full-Time Presence Plus Outreach
In 2010, after completing his medical degree, residency and pediatric cardiology fellowship at the University of Iowa Children’s Hospital, plus additional training in Michigan, Dr. Von Bergen began traveling to AFCH each month to perform EP diagnostic studies and associated treatment procedures.
In October 2014, he joined the UW faculty full-time, making him one of only three interventional pediatric cardiac electrophysiologists in Wisconsin.
He also still travels to hospitals in Iowa—as well as in South Dakota and Nevada—to perform procedures there. Among pediatric electrophysiologists, he has one of the higher individual procedural volumes in the country.
New Equipment Minimizes Radiation Exposure
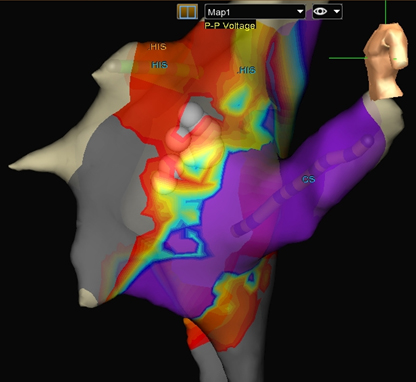
successful ablation for AVNRT.
Depending on the type and severity of a child’s arrhythmia, Dr. Von Bergen may implant a pacemaker or an implantable cardioverter-defibrillator, or perform a catheter-guided ablation, a treatment to burn or freeze the tissue that’s causing the abnormal rhythm.
Traditionally, physicians use fluoroscopy to visualize the catheter’s position during an ablation. AFCH, however, is one of a handful of centers that utilizes 3-D mapping instead of radiation for majority of those procedures, making them even safer.
An expert in this new technology, Dr. Von Bergen was the first in the world to report on no-radiation ablations in patients with ventricular tachycardia. He has also used 3-D mapping with ultra-low radiation to perform an ablation on a seven-pound infant, the smallest child known to have received such a procedure.
He is a firm believer that the radiation-free technique helps increase the accuracy and decreases the risks associated with ablation, and is training other physicians around the Midwest in the technique.
Better Mapping Techniques Improve Outcomes
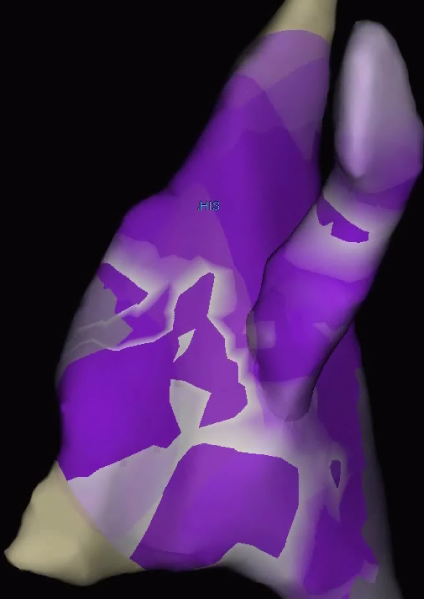
waves begin to collapse—a possible target
for ablation.
Dr. Von Bergen is also piloting research to improve outcomes for children with atrioventricular nodal re-entry tachycardia (AVNRT), a common supraventricular arrhythmia that manifests as a sudden-onset fast heart rate.
Because there is no foolproof way for physicians to identify the exact anatomic pathway that causes AVNRT, many ablations may require multiple test attempts at burning or freezing the tissue before the correct site is isolated. This type of arrhythmia still returns in up to 7 to 8 percent of children.
But one technique, called voltage mapping, may allow physicians to identify the area of the arrhythmia and direct the ablation to that spot.
In a 2014 article in Pediatric Cardiology, Dr. Von Bergen and his colleagues found that by using voltage mapping, they could successfully ablate AVNRT within three attempts in 63 percent of pediatric patients.
Now, he’s evaluating another technique, called propagation mapping, which monitors waves of energy as they flow through the heart. These waves of energy appear to collapse together in areas that are more likely to be the site of successful ablation.
Dr. Von Bergen hopes that by using voltage mapping and propagation mapping together, physicians can pinpoint treatment, prevent recurrences and potentially decrease the risk of damage to surrounding heart tissue.
He is leading the first study to evaluate these combined techniques, which, if proven successful, may ultimately improve the lives of children with AVNRT.