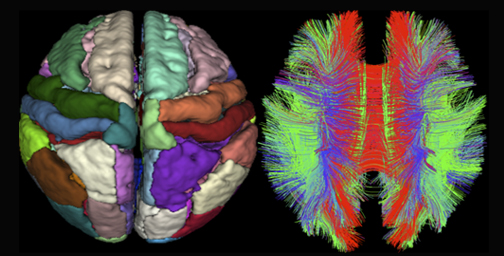
above) to map brain network connectivity in children recovering from severe TBI.
Severe traumatic brain injury (TBI) is the leading cause of death and long-term disability in children, affecting over 30,000 children each year.
Although clinicians use advanced neuroimaging tools such as magnetic resonance imaging (MRI) to diagnose TBI, little is known about how those imaging findings can be used to anticipate functional outcomes.
But thanks to a new four-year, $2M grant from the National Institutes of Health–National Institute of Neurological Disorders and Stroke, a research team led by Peter Ferrazzano, MD, will use MRI to identify brain network injuries that may predict specific neurocognitive deficits after TBI—information that may help clinicians determine appropriate therapy.
Connecting Brain Network Injury to Future Impairments
Dr. Ferrazzano’s research uses a new framework for understanding functional impairments after TBI, in which injury to the long-distance fiber tracts that connect brain network nodes—or direct injury to the nodes themselves—disrupts brain network function, resulting in cognitive or psychological impairments to the domain served by that network.
Using that framework, investigators will focus specifically on three well-defined brain networks:
- The Default Mode Network, which guides executive function and attention;
- The Hippocampal Memory Network, which guides memory encoding and recall; and
- The Fronto-Limbic Network, which guides anxiety and depression.
Partnering with the ADAPT Trial
Dr. Ferrazzano’s team is partnering with an existing multicenter pediatric TBI clinical trial (the Approaches and Decisions in Acute Pediatric TBI, or ADAPT, trial) for recruitment, data collection and analysis.
They will collect acute MRI scans from approximately 400 children with severe TBI who are enrolled in the ADAPT Trial. One year after injury, they will perform follow-up imaging, including advanced MRI techniques such as Diffusion Tensor Imaging and resting-state functional MRI, on 100 patients at 15 sites around the U.S. They will then correlate imaging findings with the extensive acute clinical data and comprehensive neuropsychological testing collected for the ADAPT trial.
The project is the largest MRI study of severe pediatric TBI to date. Dr. Ferrazzano hopes that it will provide valuable information for improved clinical decision making.
“Given the prevalence of brain injury in pediatric populations and its potential for devastating, lifelong deficits, improving outcomes in these children is an important public health goal,” Ferrazzano noted. “Being able to anticipate the needs of children suffering the aftereffects of brain injury will allow health care professionals to provide timely interventions and rehabilitation,” he added.
Dr. Ferrazzano’s collaborators include co-PI Andy Alexander, PhD (MR Physics, Waisman Lab for Brain Imaging and Behavior); Aaron Field, MD, PhD (Neuroradiology); Rasmus Birn, PhD (Psychiatry); Jeanette Mumford, PhD (Waisman Center); Paul Rathouz, PhD (Biostatistics and Medical Informatics); and Kate Bowen, PhD (Pediatric Neuropsychology).