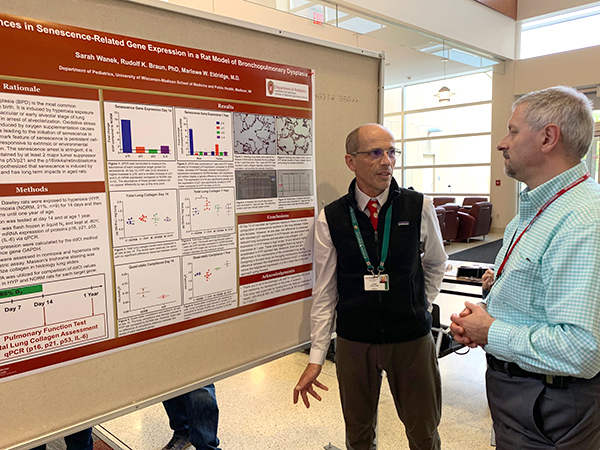
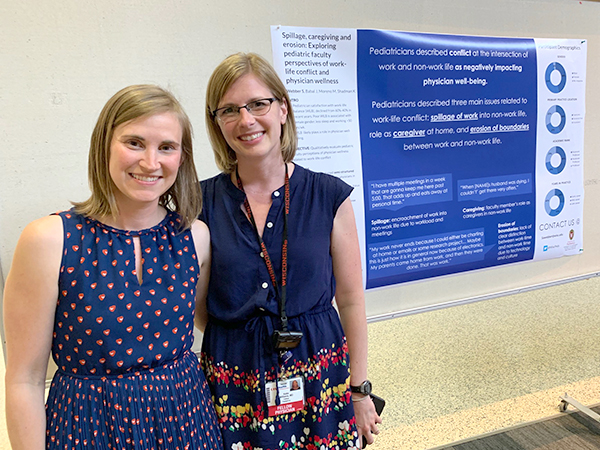
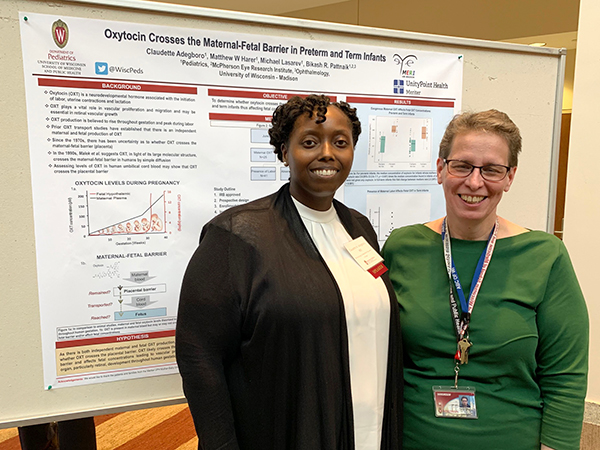
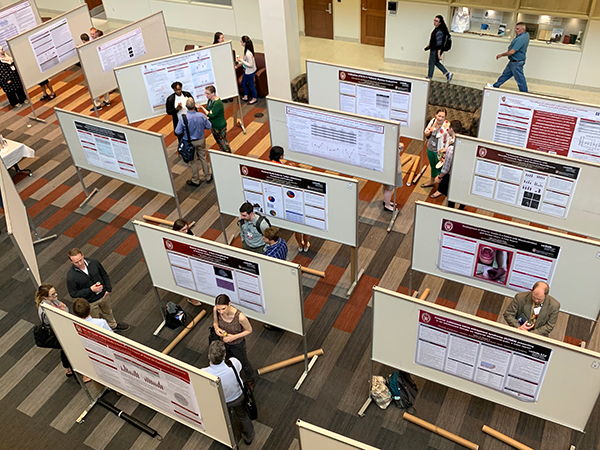
Lectures by the 2018 and 2019 Gerard B. Odell Research Award winners, along with rows of research posters filling the Health Sciences Learning Center (HSLC) were among the highlights of the Department of Pediatrics’ 2019 Spring Research Week, held May 28-31, 2019.
Dr. David McCulley on Congenital Diaphragmatic Hernia
On Thursday, May 30, David McCulley, MD (Assistant Professor, Division of Neonatology and Newborn Nursery), gave the 2019 Gerard B. Odell Lecture and Grand Rounds presentation, “Clinical and Basic Research Advances for Congenital Diaphragmatic Hernia.” (View video)
A congenital defect that occurs in one of every 3,500 live births, CDH is associated with impaired lung and pulmonary vascular development and function. Depending on severity, it has a 20 to 50 percent mortality rate.
At UW Health, Dr. McCulley and a multidisciplinary team created a standardized postnatal treatment protocol for CDH that over the past four years, improved survival and decreased the need for extracorporeal membrane oxygenation (ECMO). The team is currently investigating how the use of innovative ventilation techniques and bridled nastrogastric tubes can reduce the length of hospital stays and the need for gastrostromy tube placement in newborns with CDH.
Dr. McCulley then shifted his presentation into a discussion of the genetic mechanisms of CDH, which are poorly understood and the focus of his basic science research program.
He explained how a gene, pre-B-cell leukemia factor (Pbx1), which is required for diaphragm formation, controls postnatal growth of lung alveoli and pulmonary vasculature. He shared his recently published research showing that newborn mice without this gene fail to thrive after birth, die within two to three weeks, and have underdeveloped lungs, cardiac hypertrophy and pulmonary hypertension.
In addition, mice without a protein-coding gene called SIN3A also have abnormal diaphragm development, underdeveloped lungs, lung hypoplasia and pulmonary hypertension.
Dr. McCulley recently received his first R01 award from the National Institutes of Health National Heart, Lung, and Blood Institute to further study how these genetic variations impact the development of CDH.
Dr. Christian Capitini on Career Paths and Keys to Success
On Friday, May 31, Christian Capitini, MD (Assistant Professor, Division of Hematology, Oncology and Bone Marrow Transplant), presented the 2018 Odell Lecture and Research Day keynote address, “Unlocking the Physician-Scientist-Educator-Advocate Within.”
He reflected on how his career path as a cancer researcher began in high school, as a participant in a summer science research internship program. For the next 14 years, as he completed college, medical school, residency and fellowship training, he wove basic science research into each phase of his education. After serving for three years as an instructor at the National Cancer Institute, he joined the faculty of the Department of Pediatrics in 2011 as an assistant professor.
After explaining how graft-versus-host disease remains one of the key challenges in using allogeneic bone marrow transplant to treat childhood cancer, Dr. Capitini recalled how the 2013 creation of the Stand Up to Cancer/St.Baldrick’s Foundation Dream Team influenced his career. The Dream Team brought together scientists at the University of Wisconsin Carbone Cancer Center (including himself and his mentor, Paul Sondel, MD, PhD), and those from six other North American cancer centers to team up and develop new immune-based therapies for childhood cancer.
At UW-Madison, that award resulted in lab research on using natural-killer cells to target and treat neuroblastoma, resulting in Dr. Capitini’s first R01 award, and clinical research on using CAR T therapy for B-cell acute lymphoblastic leukemia. In 2017, the U.S. Food and Drug Administration approved the use of CAR T-cell therapy on select patients; today, American Family Children’s Hospital is one of over 50 sites certified to administer CAR T cells, largely through Dr. Capitini’s leadership.
Dr. Capitini then shared an acronym he read about that he considers to be the keys to a successful career in academic medicine: commitment, organization, mentorship, information and communication (or COMIC, for short).
He encouraged residents and fellows to start out by writing case reports or invited reviews, networking at national meetings, working in a lab, and writing and publishing research results.
And for those not yet certain of their career path, he closed with examples of less traditional careers in pediatrics, including government positions, serving as an expert witness or advising on public policy. He also emphasized maintaining a good work-life balance.
Six Oral Presentations and 80 Posters
Research Day continued with six oral presentations:
- “Near Infrared Spectroscopy Detects Acute Kidney Injury in Preterm Neonates” (Claudette Adegboro, MD; neonatology and newborn nursery fellow)
- “Newborn Screening Alone Insufficient to Improve Pulmonary and Mortality Outcomes for CF” (Christina Barreda, MD; pulmonology and sleep medicine fellow)
- “Incidence and Significance of Elevated Transaminases in Infants with Failure to Thrive” (Kristen A. Marten, MD; third-year resident and incoming chief resident)
- “The Pediatric Asthma Risk Score (PARS) Predicts Atopic and Non-atopic Asthma Better than the Asthma Predictive Index” (Eric M. Schauberger, DO, PhD; Assistant Professor, Division of Allergy, Immunology, and Rheumatology)
- “Infant Mortality Rates in Wisconsin Using Direct Adjustment Method” (Brandon D. Tomlin, MD; second-year resident)
- “Perceived Consequences of Work-related Technology” (Sarah A. Webber, MD; Assistant Professor, Division of Hospital Medicine)
It also included 80 abstracts by faculty, fellows, residents and students on display as posters in the HSLC atrium throughout Friday afternoon. Of these, 31 (39%) had been presented at April’s Pediatric Academic Societies (PAS) meeting: 28 as poster presentations and three as platform presentations.
Other activities during Research Week included a panel discussion on scholarly approaches to quality improvement; a lecture by Norman Fost, MD (Professor Emeritus, Division of Child Protection and Bioethics) on ethical considerations in pediatric research; and a presentation by James Gern, MD (Vice Chair for Research and Chief, Division of Allergy, Immunology and Rheumatology) and Kim Stevenson (Assistant Director of Research) on important updates in research proposal development and submission.
The Odell Lecture is named for Gerard B. Odell, MD, who directed the Department of Pediatrics’ Division of Gastroenterology and Nutrition from 1976 through 1991. Dr. Odell was internationally recognized for his research in the field of neonatal jaundice and bilirubin metabolism, and was highly influential in improving the quality of care for newborns and children with liver disease.
The Gerard B. Odell Research Award is given to an assistant or associate professor of pediatrics in recognition of outstanding research accomplishments and demonstrated potential for future contributions.