Inflammation is a hallmark of many human diseases and can lead to pain, organ dysfunction, and irreversible tissue damage. In the gastrointestinal tract, potentially inflammatory and damaging molecules — such as enzymes, acids, and the normal microbiome — are abundant, but these “normal” stressors do not lead to tissue inflammation.
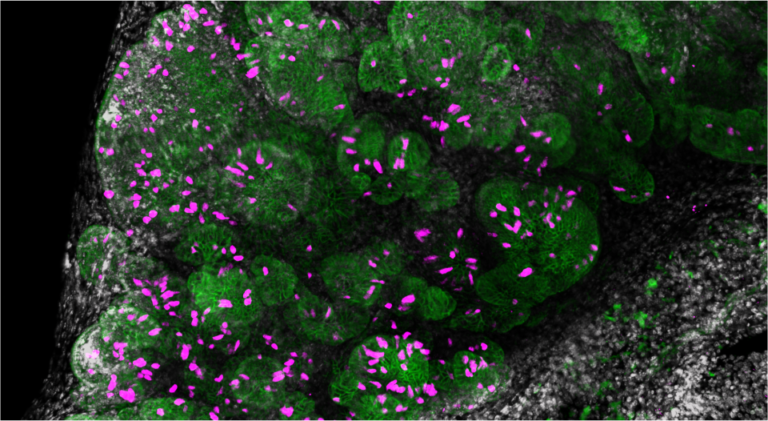
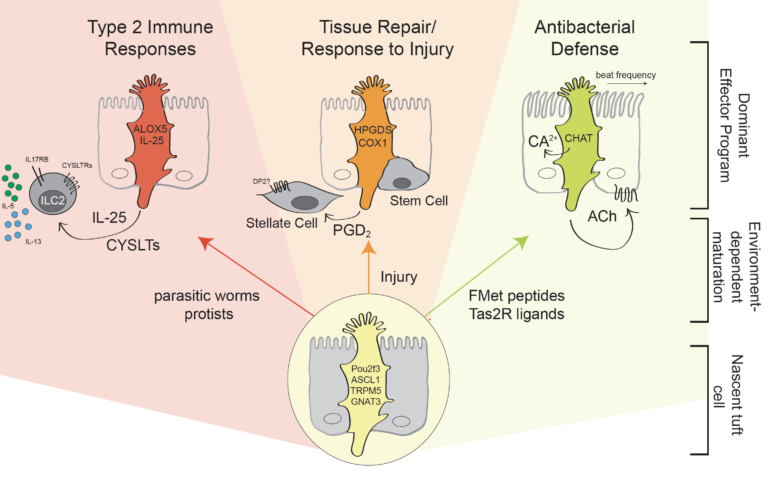
The O’Leary lab is studying how gastrointestinal tissues restrain immune activation in the face of harsh environments, while also retaining the capacity for a rapid response to pathogens. We are focused on how rare cells, called tuft cells, in the single cell epithelial barrier lining the gastrointestinal tract coordinate defensive and protective responses to changing conditions, including microbial metabolites. We are also investigating the role of barrier function and the microbiome in inflammation in the biliary tract (gallbladder and bile ducts), an understudied tissue with constant exposure to high concentrations of bile acids, which have damaging detergent-like properties. Bile acids themselves are potent signaling molecules, and modified by the microbiome. How this metabolically active set of molecules impacts immune cells remains unclear, and is a focus of our research.
We are accepting new graduate students in fall of 2023, and are hiring for a T32-supported postdoctoral fellow position! See job posting (search “O’Leary”): https://hr.wisc.edu/postdoc-and-research-intern-vacancies/
Research Opportunities – Graduate Students
For students interested in obtaining a PhD, Dr. O’Leary is a trainer for the Cellular and Molecular Pathology (CMP), Cellular and Molecular Biology (CMB), and the Microbiology Doctoral Training Program Graduate Programs. For more information, please click on the link for each program above.
Research Opportunities – Postdoctoral Fellows
Interested applicants with experience in tissue immunology, epithelial-immune interactions and/or the microbiome may send a cover letter, CV, and emails for 3 references to coleary@wisc.edu for consideration.
Research News

New Faculty Focus: Claire O’Leary
Q&A with Claire O’Leary, PhD, assistant professor, Division of Allergy, Immunology, and Rheumatology, and the O’Leary Research Group Hometown: St Paul, Minnesota Educational/professional background: I earned my BA in Molecular Biology (honors) and Spanish from …
November 3, 2022- More O'Leary Research Group News posts

Assistant Professor
coleary@wisc.edu